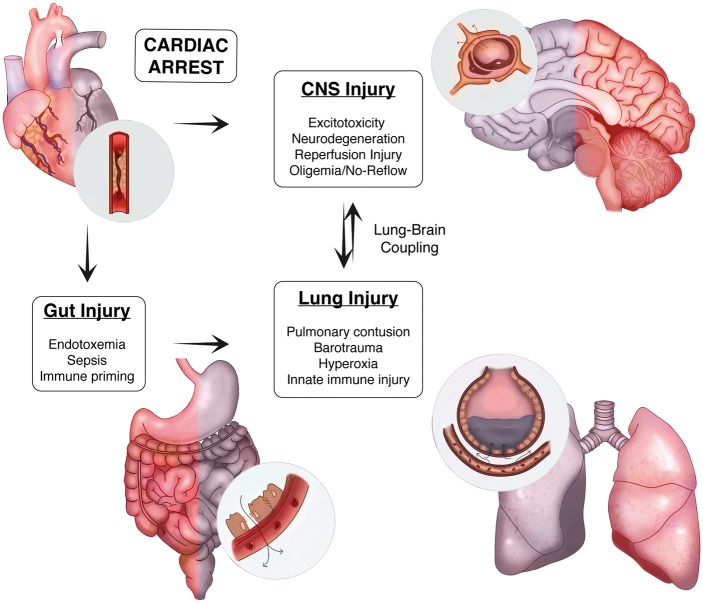
Figure 1.
Lung–brain coupling in the post-cardiac arrest syndrome. Acute myocardial ischemia and associated ventricular arrhythmia induce end organ ischemic injury by perturbing systemic perfusion. In the CNS, ischemia induces cellular injury directly through both acute and delayed mechanisms. In the periphery, ischemia damages the physical, biochemical, and immune defenses present within the intestinal mucosae resulting in the translocation of gastrointestinal flora and systemic release of pro-inflammatory molecules and microorganisms. With the return of spontaneous circulation and tissue reperfusion, hematogenous spread of DAMPs from the CNS and PAMPs from the gut trigger acute lung inflammation. These systemic factors, combined with a variety of iatrogenic insults to the lung during the early phase of treatment, contribute to a feed-forward mechanism of reperfusion injury that heightens post-ischemic neuroinflammation.