Abstract
We report the intentional occlusion of the middle meningeal artery arising from the lacrimal artery, a novel technique to improve drug delivery in a 14-month-old boy with a history of right sporadic unilateral cavitary retinoblastoma group D. The patient was referred to our institution for intra-arterial chemotherapy after two systemic chemotherapy treatments. The digital subtraction angiography showed a large middle meningeal artery arising from the right lacrimal artery and decrease choroidal enhancement thus decreased flow to the tumor. The ophthalmological examination after the first intra-arterial chemotherapy observed no tumor regression. Assuming a vascular steal, in the second intra-arterial chemotherapy session, the origin of the middle meningeal artery was occluded. Following this treatment, a significant response was observed at ophthalmological follow up. In the presented case, the efficacy of intra-arterial chemotherapy was improved after occlusion of a meningeal branch arising from the lacrimal artery, which was responsible for the vascular steal.
Keywords: Intra-arterial chemotherapy, ophthalmic artery, retinoblastoma
Background
Retinoblastoma is the most common primary ocular malignancy in childhood. The delivery of intra-arterial chemotherapy (IAC) has improved over time. Reese et al.1 in 1958 described chemotherapy delivery in the cervical portion of the internal carotid artery. To improve this non-selective technique, a temporary balloon occlusion of the internal carotid artery distal to the origin of the ophthalmic artery (OA) was attempted.2 Recently Abramson et al.3 proposed a direct catheterization of the OA, which is considered the standard of care in centers performing intra-arterial treatment for retinoblastoma. At the same time, alternative approaches and techniques were additionally described to improve drug availability to the tumor. We report on the case of a patient where we occluded the middle meningeal artery (MMA) to improve drug delivery to the tumor.
Case presentation
A 14-month-old boy with a history of right sporadic unilateral cavitary retinoblastoma group D was referred to our institution for IAC after two systemic chemotherapy treatments.
Treatment
In the first session of IAC, the selective angiogram of the ophthalmic artery showed a large meningeal MMA arising from the lacrimal artery. As the choroidal blush was visible, 4 mg of melphalan via the microcatheter situated at the origin of the ophthalmic artery were delivered. On subsequent ophthalmological examination, no tumor regression was observed. This observation made us think of a modified approach for the second IAC. A 4F guiding catheter (Terumo, Tokyo, Japan) was placed in the right internal carotid artery and a HeadwayDuo microcatheter over a 0.014 inch Traxcess microguidewire (Microvention, Tustin, California, US) advanced in the origin of the MMA, which was subsequently occluded by three detachable coils. The selective angiogram confirmed the occlusion of the MMA (Figure 1); 4 mg of melphalan was then delivered through the same microcatheter into the OA. The procedure was uneventful. Following this chemotherapy treatment, a significant response was observed at ophthalmological follow up. A third IAC was followed 1 month later by two sessions of intraophthalmic thermotherapy led to complete response with a type III regression of the tumor (Figure 2). At 3 months of follow up, there are no signs of active disease and the child is doing well.
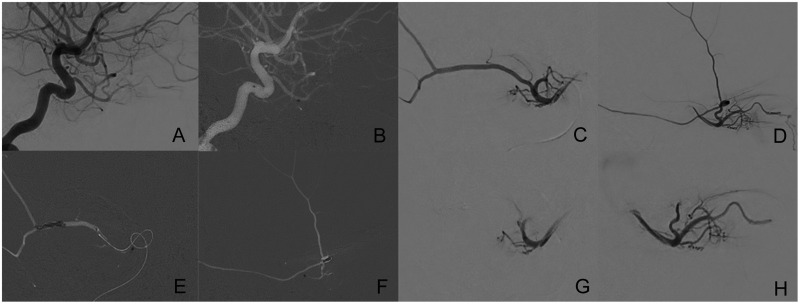
Figure 1.
(a) Lateral digital subtraction angiography (DSA) view of the internal carotid artery and ophtalmic artery. (b) Navigation of the microcatheter into the ophthalmic artery. (c) Anteroposterior and (d) lateral DSA views of the ophthalmic, lacrimal and middle meningeal artery. (e) Anteroposterior and (f) lateral DSA roadmap views after the delivery of the coils in the middle meningeal artery. (g) Anteroposterior and (h) lateral DSA views confirming the occlusions of the middle meningeal artery.
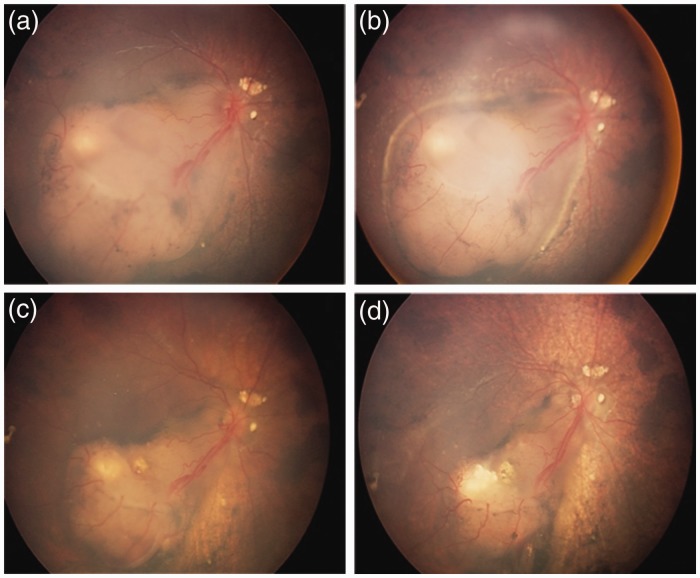
Figure 2.
(a) Ophthalmoscopy images before, (b) after first treatment with intra-arterial chemotherapy, (c) after second treatment with intra-arterial chemotherapy and occlusion of the middle meningeal artery, (d) after last intra-arterial chemotherapy.
Discussion
Direct catheterization of the ophthalmic artery is currently the optimal way to deliver IAC for intraocular retinoblastoma, as described by Abramsom et al.3 Nevertheless, as previously described,4 two technically challenging scenarios potentially undermine IAC outcome and are unfortunately frequently encountered in the angiograph room. The first scenario is the instability of the microcatheter at the ostium of the OA. To improve stability, different techniques have been proposed such as microcatheter shaping,4 a retrograde approach through the posterior communicating artery,5 and temporary balloon occlusion of the ICA.6 The second unfavorable scenario is when an adequate choroidal blush is unattainable even when OA catheterization is achieved. This can be explained by an inversion of the flow in the ophthalmic artery due to hemodynamic balance between ICA and external carotid artery (ECA). In cases of hemodynamic balance between ICA and ECA, Klufas et al.6 proposed selective injection of the chemotherapy in the orbital branch of the MMA. This technique appears safe and effective, but occasionally the intraorbital anastomosis is very small, rendering superselective catheterization unfeasible. In this case, to improve drug delivery, Bertelli et al.4 proposed injection of liquid adhesives into the extraorbital vessels arising from the ECA to alter intraorbital circulation. Additionally, temporary balloon occlusion of the ECA to redirect flow to the ICA and subsequently to the OA was described.7 Although these techniques are useful and generally effective in hemodynamic balance between ICA and ECA, it does not provide a solution for a vascular steal from large MMA coming from the lacrimal artery. In our patient, in the first procedure using a standard treatment strategy by placing the microcatheter at the origin of the OA, the tumor response was partial. This cannot be explained by the cavitary type of the tumor, known to be usually less responsive, as a significant decrease in tumor volume had been already observed initially after two cycles of systemic chemotherapy. We assumed that a large quantity of the drug was redirected into the MMA, causing only a partial tumor response. To improve drug availability to the target as suggested by Bertelli et al.4 in the ECA, we decided to occlude the origin of the MMA in the second session. Different agents can be used to occlude this artery, such as liquid embolic agents, flush coils and detachable coils. We decided to occlude the artery by detachable coils, which were delivered via a larger and stable microcatheter to ensure controlled and safe coil detachment. Furthermore, the caliber of the ophthalmic artery was unusually large and thus the selective catheterization was quick and not challenging. Occlusion of the origin of the MMA could potentially lead to a shrinkage of the OA, thus hampering the stability or navigation of the microcatheter for further procedures. However, in our third and last session, the caliber of the OA remained unchanged and the IAC was performed without incident.
Learning points
Intra-arterial chemotherapy of retinoblastoma has been shown to improve clinical outcome.
Drug delivery and availability might explain the limited response in some tumors.
By optimizing delivery and availability, we can improve the efficacy of IAC.
Further studies and cases are required to support this finding.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Reese AB, Hyman GA, Tapley ND, et al. The treatment of retinoblastoma by x-ray and triethylene melamine. AMA Arch Ophthalmol 1958; 60: 897–906. [DOI] [PubMed] [Google Scholar]
- 2.Yamane T, Kaneko A, Mohri M. The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Int J Clin Oncol 2004; 9: 69–73. [DOI] [PubMed] [Google Scholar]
- 3.Abramson DH, Dunkel IJ, Brodie SE, et al. A phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma initial results. Ophthalmology 2008; 115: 1398–1404, 404 e1. [DOI] [PubMed] [Google Scholar]
- 4.Bertelli E, Leonini S, Galimberti D, et al. Hemodynamic and anatomic variations require an adaptable approach during intra-arterial chemotherapy for intraocular retinoblastoma: Alternative routes, strategies, and follow-up. AJNR Am J Neuroradiol 2016; 37: 1289–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pham CT, Blanc R, Lumbroso-Le Rouic L, et al. Access to the ophthalmic artery by retrograde approach through the posterior communicating artery for intra-arterial chemotherapy of retinoblastoma. Neuroradiology 2012; 54: 845–848. [DOI] [PubMed] [Google Scholar]
- 6.Klufas MA, Gobin YP, Marr B, et al. Intra-arterial chemotherapy as a treatment for intraocular retinoblastoma: Alternatives to direct ophthalmic artery catheterization. AJNR Am J Neuroradiol 2012; 33: 1608–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abruzzo TA, Geller JI, Kimbrough DA, et al. Adjunctive techniques for optimization of ocular hemodynamics in children undergoing ophthalmic artery infusion chemotherapy. J Neurointerv Surg 2015; 7: 770–776. [DOI] [PubMed] [Google Scholar]