Abstract
We report a case of disseminated cryptococcosis in a treatment-naïve chronic lymphocytic leukemia (CLL) patient. A 60-year-old man presented with a two-week history of intermittent fevers, frontal headaches, night sweats, weight loss and multiple pink papules on hands and face. Cryptococcemia was found by blood culture unexpectedly. Further investigation confirmed cryptococcal meningitis and skin disease. He responded to two week amphotericin B and flucytosine followed by four-week amphotericin B and fluconazole, three-month high dose fluconazole (800 mg/day), and maintenance fluconazole (400 mg/day) thereafter. CSF pleocytosis persisted until day 203 while cryptococcal antigen in the CSF persisted at day 334 of treatment.
Keywords: Cryptococcus, Chronic lymphocytic leukemia
Introduction
Cryptococcosis is an opportunistic infection caused by encapsulated yeast, mainly Cryptococcus neoformans, or less commonly C. gatii [1]. The majority of patients with symptomatic cryptococcosis have a clearly identified underlying immunocompromised condition. The most common underlying condition is human immunodeficiency virus (HIV) infection. The global burden of cryptococcosis in HIV-infected patients was estimated to be 6.0% in people with a CD4 cell count of less than 100 cells/μL [2]. Moreover, the incidence of cryptococcal meningitis in HIV-infected patients was estimated to be close to one million person per year [3]. The mortality rate per 100 person-years is 15.3 [95%CI, 12.2–18.4] in the combined antiretroviral treatment era [4].
Non-HIV conditions that may be associated with predisposition to cryptococcosis include corticosteroid therapy [5], cytotoxic chemotherapy, immunotherapy agents [5,6], idiopathic CD4 lymphocytopenia [7], organ transplantation [8], and decompensated liver cirrhosis [9]. In a restrospective series of 302 patients with cryptococcal infections, 39 (12.9%) of patients had no obvious risk factors for developing the infection [10].
Chronic lymphocytic leukemia (CLL) is the most common leukemia in adults in the Western hemisphere [11]. An initial course of illness is relatively benign. Treatment for advanced CLL disease is generally comprised of cytotoxic chemotherapy such as fludarabine, cyclophosphamide and rituximab [12]. Newer agents such as ibrutinib are also emerging [11]. It is well-known that infection represents a major cause of death in patients with CLL. The majority of infections affect the lower respiratory tract, and are usually caused by bacteria such as Streptococcus pneumoniae, Staphylococcus aureus and Haemophilus influenzae [13]. Patients with CLL are known to have hypogammaglobulinemia, suppression of helper T-cells, T-cell subset imbalances, diminished T-cell response to proliferative signals, inverted CD4/CD8 T-cell ratios, with a decreased CD4 T cells count and high level of cytotoxic CD8 T cells were also previously described in patients with CLL [[14], [15], [16], [17]], which have been associated with an increased rate of infection.
Opportunistic infections have been reported sporadically in patients with advanced CLL on treatment [13,18]. In most of these cases, it is thought that the treatment for CLL predisposes to opportunistic infections. However, untreated CLL is not typically seen as a risk factor for cryptococcosis. We report an atypical case of disseminated cryptococcosis, and aim to review previous case reports of cryptococcosis in untreated CLL.
Case report
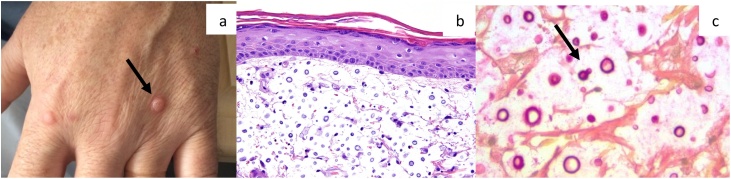
A 60-year-old man with untreated B-cell chronic lymphocytic leukemia (CLL), under a watchful waiting strategy, presented to a primary-care hospital with a two week history of intermittent fevers, mild frontal headaches, night sweats, weight loss, multiple papular pink skin lesions on his hands and face, and fatigue. Two weeks prior to presentation he had spent a week in Jamaica; while there he noticed an asymptomatic skin-coloured firm papule on the dorsum of his right hand, which gradually developed over two weeks to papules on his other hand, arms, posterior neck and face. On physical exam, he had palpable bilateral axillary lymph nodes and one palpable right inguinal lymph node. His rash consisted of multiple skin-colored to pink round papules with an erythematous rim, primarily over the patient’s dorsal hands (Fig. 1a), face and posterior neck. His cardiac, respiratory, gastrointestinal and genitourinary exams were unremarkable. His blood work showed a white blood cell count of 1 190 cells/μL, a hemoglobin of 9.5 g/dL and platelet count of 201 000 cells/μL. A CT chest showed no change in the size of previous pulmonary nodules, which prior biopsy had shown to be due to CLL infiltrates, as well as stable hepatosplenomegaly, axillary, mediastinal and hilar lymphadenopathy. Human immunodeficiency virus (HIV) serology was negative.
Fig. 1.
A. Rash on the patient’s hand upon initial presentation. B. Section of skin biopsy with hematoxylin and eosin stain, original magnification 20 × . C. Photomicrograph of the skin biopsy showing large numbers of yeast forms surrounded by a clear space, typical of the thick capsule of Cryptococcus. (Mucicarmine, magnification 63x, courtesy of Dr. Bruce Burns).
On day six of incubation, the patient’s blood cultures became positive with Cryptococcus spp. The patient was referred to our hospital, a tertiary-care hospital, on the same day and we report this as day 1 of admission. He was immediately started on liposomal amphotericin B (5 mg/kg IV q24 h). Flucytosine was not readily available because a special request was required. A biopsy of the skin lesion was performed on day 2 of admission (pathology shown in Fig. 1b and c). Lumbar puncture was performed to rule out meningitis. The cerebrospinal fluid (CSF) analysis showed 1 385 cells/μL total nucleated cells, 41% lymphocytes, 21.6 mg/dL glucose, 60 mg/dL protein, and the CSF culture showed growth of Cryptococcus neoformans, confirming cryptococcal meningitis.
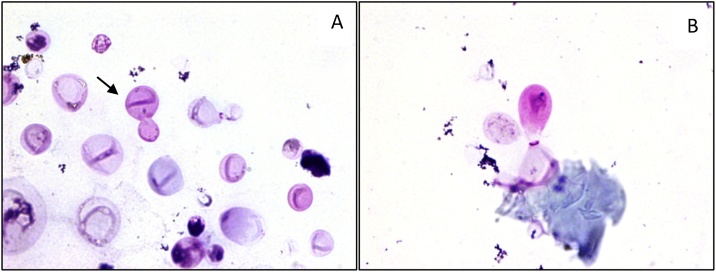
Repeat CSF on day 14 showed evidence of infection with presence of yeast cells visible by microscropy (Fig. 2a). Fluconazole 800 mg daily was added while waiting for flucytosine. Three weeks into the patient’s treatment, fluconazole was stopped and flucytosine was started at 2 g orally every 6 h. However, this was interrupted for few days due to cytopenia. The dosage was subsequently adjusted to 2 g every 12 h to enable completion of 2-week induction treatment with dual therapy of amphotericin B and flucytosine.
Fig. 2.
Cerebrospinal fluid A. Yeast cells on day 14 of treatment and B. Degenerating yeast cells on day 334 of treatment. (May-Grünwald-Giemsa, original magnification 100x oil immersion.).
Due to the extent of the disease, the treating team decided to give dual therapy for an extended duration, but flucytosine was changed to fluconazole. This dual therapy was continued until day 40 of treatment before transitioning to high-dose fluconazole monotherapy. Repeated CSF analysis at that time demonstrated persistent pleocytosis with total nucleated cells of 69 cells/μL, and cryptococcal antigen at a titer of 1:2048. During which time, the patient developed headache and floaters in his right eye. An MRI revealed multiple high T2 signal foci throughout the basal ganglia, thalamus and midbrain with associated edema, and new significant bilateral edema of the optic nerves extending to the optic discs; small cryptococcomas could not be ruled out. A neuro-ophthalmologist concluded that the patient’s symptoms were due to increased intracranial pressure. Subsequent lumbar puncture on day 100 of treatment showed 62 total nucleated cells/μL with further reduction in the cryptococcal antigen titer to 1:1024. The CSF opening pressure was unfortunately not measured. His ocular symptoms improved gradually over four weeks and remained asymptomatic over the course of this treatment. Therefore, the treating team was comfortable in starting the patient on maintenance therapy with fluconazole 400 mg daily on day 126. Interestingly, a repeat CSF analysis on day 334 of treatment showed a reduction in total nucleated cells to 3 cells/μL but cryptococcal antigen was still detected at a titer of 1:128 (Table 1).
Table 1.
Characteristics of the cerebrospinal fluid (CSF) throughout the course of the cryptococcal infection.
| Time from first treatment | Day 1 | Day 14 | Day 42 | Day 100 | Day 203 | Day 334 |
|---|---|---|---|---|---|---|
| CSF total nucleated cells (cells/μL) | 1385 | 77 | 69 | 62 | 10 | 3 |
| CSF percent neutrophils | 0% | 2% | 0% | 1% | Not available | Not available |
| CSF percent lymphocytes | 41% | 92% | 98% | 97% | Not available | Rare lymphocyte on scanning |
| CSF glucose (mg/dL) | 21.6 | 10.8 | 18 | 23.4 | 52.2 | 55.8 |
| Serum glucose (mg/dL) | 99 | 93.6 | 93.6 | Not available | 95.4 | Not available |
| CSF protein (mg/dL) | 60 | 66 | 55 | 73 | 34 | 30 |
| CSF Gram Stain | Not available | Many white cells Moderate yeast cells | Moderate white cells No organisms seen | Many white cells No organisms seen | Not available | Few white cells No organisms seen (but yeast cells noted in hematology cytospin prep) |
| CSF culture | Light growth Cryptococcus neoformans | No growth | No growth | No growth | No growth | No growth |
| CSF cryptococcal antigen titer | Not available | Not available | 1:2048 | 1:1024 | 1:512 | 1:128 |
| Antifungal treatment | IV fluconazole 800 mg, transitioned to Amphotericin B 400 mg q24h | Fluconazole 400 mg daily and Amphotericin B 400 mg q24h | Fluconazole 800 mg daily | Fluconazole 800 mg daily | Fluconazole 400 mg daily | Fluconazole 400 mg daily |
Meanwhile, the patient developed transfusion-dependent anemia, thrombocytopenia, and increased lymphadenopathy which were likely related to his underlying CLL. His hematologist therefore started the patient on ibrutinib, a Bruton tyrosine kinase inhibitor, for the treatment of CLL on day 342. Due to potential drug-drug interaction between ibrutinib and fluconazole through CYP3A4, reduced dose of ibrutinib at 140 mg daily was recommended. He has done dramatically well without worsening cryptococcosis at two-year follow-up. We plan to continue fluconazole for life as a secondary prophylaxis.
Discussion
We conducted a search for case reports or case series of cryptococcal infection in patients with CLL. We found 52 cases reported previously. Of 52, two occurred in treatment naïve CLL patients. Together with our case report, there are thus three cases in total (Table 2). All cases had documented C. neoformans, not C. gatii infection. All patients were male. The average age was 72 years old (range 60–84). CLL disease stage was not reported in two other cases [19,20]. The patient from our case was dignosed with RAI Stage I previously, however, at the time of his presentation with cryptococcosis, he appeared to progress to RAI Stage II, subsequently needing CLL treatment. All patients had disseminated disease. Two had CNS involvement [19] including our case who had a severe and prolonged CNS infection with pleocytosis and high titer of cryptococcal antigen and visible degenerating cryptococcal yeast cells in the CSF on day 334 of treatment (Fig. 2b).
Table 2.
Summary of reported Cryptococcus neoformans infection cases in untreated patients with CLL (N = 3).
| Paper | Age/Sex | CLL Stage | Clinical Presentation | Time from Presentation to Diagnosis | Extent of disease | Treatment for Cryptococcus | Outcomes | Cryptococcal CSF titers |
|---|---|---|---|---|---|---|---|---|
| Johannsson et al. 2009 [19] | 84 M | Not reported | Insidious left groin pain for several months not limiting activity. Weight loss and intermittent nausea for several months. Two-week history of sudden onset fever and sharp left groin pain. Mild frontal headache with decreased and painful range of motion of left prosthetic hip. |
Presumably within one week | Hip joint and CNS | Induction: Amphotericin B for 12 days (total dose of 800 mg). Maintenance: Oral fluconazole 400 mg daily continued for greater than 10 months. |
Resolution of symptoms after 12 days of treatment. Resection and arthroplasty performed after 10 months of medical treatment. Evidence of chronic inflammation. |
1:1 in undiluted CSF |
| Muller et al. 2010 [20] |
73 M | Not reported | Three-month history of an asymptomatic, ulcerated, rapidly growing nodule/mass on the left temporal region with severe left eyelid edema. Vision was not affected. |
Presumably within one week | Skin and blood. | Fluconazole 400 mg daily followed by voriconazole 400 mg daily for a total of 2 weeks. | 50% reduction of the skin lesion after 2 weeks of treatment. | LP not done. |
| This report | 60 M | Rai stage II | Two-week history of intermittent fevers, mild frontal headaches, night sweats, weight loss and pink papular nodular lesions on his hands and face. | Six days. | Skin, CNS and blood. | Induction: Amphotericin B and flucytosine with a transition to Amphotericin B and high dose fluconazole (800 mg/d) due to cytopenia for six weeks. Maintenance: Fluconazole 800 mg/d transitioned to 400 mg/d. |
High intracranial pressure seven weeks after treatment. Infectious symptoms resolved while on maintenance therapy. Asymptomatic at one year. | 1:2048 on Day 42 of treatment. |
Abbreviations – CLLchronic lymphocytic leukemia, CSFcerebrospinal fluid, LPlumbar puncture, CNScentral nervous system.
All presented subacutely. Fever and headache are the most common symptoms (66.7%) while none presented with alteration of consciousness. Skin lesions of our case were nodular while lesions of the other reported case were ulcerative [20]. None had cryptococcal pneumonia. All patients received fluconazole but two also received amphotericin B during induction phase. Flucytosine was only used in our case. The patient developed significant cytopenia but responded well to a decreased dose. There was no death with average follow up time of 12 months (range 2 weeks to 24 months).
A key component of the immune response in combating a cryptococcosis infection consists of cell-mediated immune responses through CD4+ and CD8+ T-cells, as described in a review by Perfect and Bicanic [21]. This has been validated in mice, where depletion of CD4 + T-cells has been shown to exacerbate CNS infection of Cryptococcus [22]. Epidemiologically, idiopathic CD4+ lymphopenia is the highest risk factor for Cryptococcus infection in non-HIV patients [23]. In a recent study by Allahmoradi et al., T-cells were isolated from twenty five untreated CLL patients and found to have a significantly lower percentage of CD4 + T-cells when compared to healthy controls [17]. This study also found that CD4 + T-cells from CLL patients had impaired proliferation and cytokine production when compared to healthy controls. Forconi and Moss described in their review how T-cells are functionally impaired in CLL, with impaired synapse between T-cells and antigen presenting cells [24]. It can be hypothesized that patients with CLL who have impaired function of their CD4+T-cells are at a higher risk for infection by pathogens such as Cryptococcus, which are typically recognized by a cell-mediated immunity. The decrease in immune response is also supported by the decreased response in untreated CLL patients to the conjugated pneumococcal vaccine. Pasiarski et al. described how 58.3% of CLL patients produced an adequate response to vaccination as compared to 100% of the control healthy patients [25]. The antibodies created by the proliferating B-cells in CLL have been characterized as pathogenic and target-restricted, suggesting that patients with CLL have defective humoral immunity in addition to the inadequate cell-mediated immune response [26].
While HIV-infected patients with cryptococcosis typically present with headache, fever, and altered mental status, CLL patients present with symptoms that may not initially suggest a cryptococcal infection, such as weight loss and cough [27,28]. As a result of the atypical presentation, patients were often treated with antibacterials for a bacterial infection before the true diagnosis was revealed [[28], [29], [30]]. Our case highlights the importance of recognizing the broad spectrum of infections that can present in patients with CLL.
Conclusion
Our case highlights the rare disseminated cryptococcosis in a fully treatment-naïve CLL patient, suggesting that hematologic malignancies predispose patients to a variety of opportunistic infections. Presentations are non-specific but outcome is favorable. Persistent CSF cryptococcal antigen can be seen. Physicians should be aware of possibility of disseminated cryptococcosis in patients with treatment-naïve CLL.
Conflicts of interest
We have no conflicts of interest to declare.
Author contribution
JC – supervised Adam Suleman, edited and reviewed the manuscript.
AS – reviewed the case, literatures and wrote original draft.
RP – performed literature search, provided input from histological aspect and reviewed manuscript.
CF – provided input from hematology aspect and reviewed manuscript.
References
- 1.Warkentien T., Crum-Cianflone N.F. An update on cryptococcosis among HIV-Infected persons. Int J STD AIDS. 2010;21:679–684. doi: 10.1258/ijsa.2010.010182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajasingham R., Smith R.M., Park B.J., Jarvis J.N., Govender N.P., Chiller T.M. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17:873–881. doi: 10.1016/S1473-3099(17)30243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park B.J., Wannemuehler K.A., Marston B.J., Govender N., Pappas P.G., Chiller T.M. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 4.Lortholary O., Poizat G., Zeller V., Neuville S., Boibieux A., Alvarez M. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS Lond Engl. 2006;20:2183–2191. doi: 10.1097/01.aids.0000252060.80704.68. [DOI] [PubMed] [Google Scholar]
- 5.Liao T.-L., Chen Y.-M., Chen D.-Y. Risk factors for cryptococcal infection among patients with rheumatoid arthritis receiving different immunosuppressive medications. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2016;22:815. doi: 10.1016/j.cmi.2016.05.030. e1-815.e3. [DOI] [PubMed] [Google Scholar]
- 6.Shih C.-C., Chen Y.-C., Chang S.-C., Luh K.-T., Hsieh W.-C. Cryptococcal meningitis in non‐HIV‐infected patients. QJM Int J Med. 2000;93:245–251. doi: 10.1093/qjmed/93.4.245. [DOI] [PubMed] [Google Scholar]
- 7.Zonios D.I., Falloon J., Huang C.-Y., Chaitt D., Bennett J.E. Cryptococcosis and idiopathic CD4 lymphocytopenia. Medicine (Baltimore) 2007;86:78–92. doi: 10.1097/md.0b013e31803b52f5. [DOI] [PubMed] [Google Scholar]
- 8.Singh N., Dromer F., Perfect J.R., Lortholary O. Cryptococcosis in solid organ transplant recipients: current state-of-the-Science. Clin Infect Dis Off Publ Infect Dis Soc Am. 2008;47:1321–1327. doi: 10.1086/592690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin Y.-Y., Shiau S., Fang C.-T. Risk factors for invasive Cryptococcus neoformans diseases: a case-control study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0119090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brizendine K.D., Baddley J.W., Pappas P.G. Predictors of mortality and differences in clinical features among patients with cryptococcosis according to immune status. PLoS One. 2013;8 doi: 10.1371/journal.pone.0060431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain N., Chen Q., Ayer T., O’Brien S.M., Keating M., Wierda W. Prevalence and economic burden of chronic lymphocytic leukemia (CLL) in the era of oral targeted therapies. Blood. 2015;126 doi: 10.1200/JCO.2016.68.2856. 871–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Badoux X.C., Keating M.J., Wang X., O’Brien S.M., Ferrajoli A., Faderl S. Fludarabine, cyclophosphamide, and rituximab chemoimmunotherapy is highly effective treatment for relapsed patients with CLL. Blood. 2011;117:3016–3024. doi: 10.1182/blood-2010-08-304683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dearden C. Disease-specific complications of chronic lymphocytic leukemia. Hematol Am Soc Hematol Educ Program. 2008:450–456. doi: 10.1182/asheducation-2008.1.450. [DOI] [PubMed] [Google Scholar]
- 14.Itälä M., Helenius H., Nikoskelainen J., Remes K. Infections and serum IgG levels in patients with chronic lymphocytic leukemia. Eur J Haematol. 1992;48:266–270. doi: 10.1111/j.1600-0609.1992.tb01805.x. [DOI] [PubMed] [Google Scholar]
- 15.Ravandi F., O’Brien S. Immune defects in patients with chronic lymphocytic leukemia. Cancer Immunol Immunother CII. 2006;55:197–209. doi: 10.1007/s00262-005-0015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonzalez-Rodriguez A.P., Contesti J., Huergo-Zapico L., Lopez-Soto A., Fernández-Guizán A., Acebes-Huerta A. Prognostic significance of CD8 and CD4 T cells in chronic lymphocytic leukemia. Leuk Lymphoma. 2010;51:1829–1836. doi: 10.3109/10428194.2010.503820. [DOI] [PubMed] [Google Scholar]
- 17.Allahmoradi E., Taghiloo S., Tehrani M., Hossein-Nattaj H., Janbabaei G., Shekarriz R. CD4+ t cells are exhausted and show functional defects in chronic lymphocytic leukemia. Iran J Immunol IJI. 2017;14:257–269. doi:IJIv14i4A1. [PubMed] [Google Scholar]
- 18.Morrison V.A. Infectious complications in patients with chronic lymphocytic leukemia: pathogenesis, spectrum of infection, and approaches to prophylaxis. Clin Lymphoma Myeloma. 2009;9:365–370. doi: 10.3816/CLM.2009.n.071. [DOI] [PubMed] [Google Scholar]
- 19.Johannsson B., Callaghan J.J. Prosthetic hip infection due to Cryptococcus neoformans: case report. Diagn Microbiol Infect Dis. 2009;64:76–79. doi: 10.1016/j.diagmicrobio.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Müller C.S., Schmaltz R., Vogt T. Secondary cutaneous cryptococcosis mimicking a malignant ulcerated tumor of the facial skin in an immunosuppressed patient. Eur J Dermatol EJD. 2010;20:657–658. doi: 10.1684/ejd.2010.1043. [DOI] [PubMed] [Google Scholar]
- 21.Perfect J.R., Bicanic T. Cryptococcosis Diagnosis and Treatment: What Do We Know Now. Fungal Genet Biol FG B. 2015;78:49–54. doi: 10.1016/j.fgb.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buchanan K.L., Doyle H.A. Requirement for CD4+ t lymphocytes in host resistance against Cryptococcus neoformans in the central nervous system of immunized mice. Infect Immun. 2000;68:456–462. doi: 10.1128/iai.68.2.456-462.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williamson P.R., Jarvis J.N., Panackal A.A., Fisher M.C., Molloy S.F., Loyse A. Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat Rev Neurol. 2017;13:13–24. doi: 10.1038/nrneurol.2016.167. [DOI] [PubMed] [Google Scholar]
- 24.Forconi F., Moss P. Perturbation of the normal immune system in patients with CLL. Blood. 2015;126:573–581. doi: 10.1182/blood-2015-03-567388. [DOI] [PubMed] [Google Scholar]
- 25.Pasiarski M., Rolinski J., Grywalska E., Stelmach-Goldys A., Korona-Glowniak I., Gozdz S. Antibody and plasmablast response to 13-valent pneumococcal conjugate vaccine in chronic lymphocytic leukemia patients--preliminary report. PLoS One. 2014;9 doi: 10.1371/journal.pone.0114966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caligaris-Cappio F. B-chronic lymphocytic leukemia: a malignancy of anti-self B cells. Blood. 1996;87:2615–2620. [PubMed] [Google Scholar]
- 27.Marchand T., Revest M., Tattevin P., Chevrier S., Poullot E., Lamy T. Early cryptococcal meningitis following treatment with rituximab, fludarabine and cyclophosphamide in a patient with chronic lymphocytic leukemia. Leuk Lymphoma. 2013;54:643–645. doi: 10.3109/10428194.2012.717081. [DOI] [PubMed] [Google Scholar]
- 28.Okamoto K., Proia L.A., Demarais P.L. Disseminated cryptococcal disease in a patient with chronic lymphocytic leukemia on ibrutinib. Case Rep Infect Dis. 2016 doi: 10.1155/2016/4642831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.IMAJ Israel Med Assoc J. 2009;11(July (7)) Cryptococcal Meningitis in Chronic Lymphocytic Leukemia Patients n.d https://www.ima.org.il/MedicineIMAJ/viewarticle.aspx?year=2009&month=07&page=437(accessed October 28, 2017) [Google Scholar]
- 30.Dizdar O.S., Karakeçili F., Coşkun B.N., Ener B., Ali R., Mıstık R. Fatal cryptococcal meningitis in a patient with chronic lymphocytic leukemia. Mediterr J Hematol Infect Dis. 2012;4 doi: 10.4084/MJHID.2012.039. [DOI] [PMC free article] [PubMed] [Google Scholar]