Abstract
Introduction
The characteristics of radial pressure pulse waves (RPPW) provide an essential diagnostic technique in Traditional Chinese Medicine (TCM). The purpose of this research is to develop a study protocol that integrates the concept of TCM and traditional acupuncture treatment with modern scientific tools utilizing a quasi-experimental design. We will investigate the effects of acupuncture on the RPPW in study participants with low back pain (LBP) using modern tools, including the pulse sphygmograph, the fingertip-to-floor test, the Faces Pain Scale-Revised, the Oswestry Disability Index, the Health Status Questionnaire, and the Constitution in Chinese Medicine Questionnaire.
Methods
We will attempt to recruit 80 eligible subjects with LBP based on our predefined inclusion and exclusion criteria. Acupuncture intervention will be performed bilaterally on Shenshu (BL23), Dachangshu (BL25) and Weizhong (BL40) for 20 min. Objective and subjective baseline assessments and outcome evaluations will be performed at a specific time before and after the intervention. This paper describes the methods of our original research approved by the China Medical University Hospital's Research Ethics Committee. Recruitment is in progress and data collection will continue until March 2019.
Conclusions
To our knowledge, this preliminary study is the first attempt to investigate the effects of acupuncture on the RPPW in LBP subjects using a pulse sphygmograph and other modern tools. The findings will also investigate the effectiveness of the selected acupuncture point combinations for LBP. We hope this preliminary study will provide a basic foundation for a large-scale research study that involves randomisation in the future.
Keywords: Acupuncture, low back pain, lumbago, pulse diagnosis, radial pressure pulse wave, Traditional Chinese Medicine, protocol
1. Introduction
The characteristics of radial pressure pulse waves (RPPW) provide an essential diagnostic technique in Traditional Chinese Medicine (TCM). Traditionally, physicians palpate the radial pulse to diagnose the TCM syndrome differentiation of the diseases in addition to other clinical observations. The pulse diagnosis also guides the physician in the clinical decision-making of the treatment strategy and evaluates its effectiveness.
There are 28 types of radial pulse profiles documented in the ancient TCM texts. Each profile is characterised by its pulse depth, pulse rate, pulse waveform, pulse density and pulse intensity. Conventionally, the wrist radial pulse is palpated by the physician using the index, middle and fourth fingers simultaneously or individually. The radial pulse is divided into three regions that represent the positions of Cun, Guan and Chi pulse. Each pulse corresponds to the meridians and the visceral organs as illustrated in Fig. 1 [1].
Fig. 1.
Current practice of pulse diagnosis in TCM.
The conventional method of pulse diagnosis relies absolutely on the physician's finger sensitivity and his personal experiential judgement. These subjective assessments can lead to inconsistency in diagnosis and treatments. Hogeboom (2001) and Coeytaux et al. (2006) studied the variability in the diagnosis and treatments of acupuncturists. They concluded that TCM diagnosis and the choice of treatment regimens varied widely among physicians [2,3].
Therefore, with the development of modern scientific tools like the pulse sphygmograph, the digitalisation of pulse profiles has provided quantitative and objective assessments of the radial pulse. Table 1 provides the significant developments of some modern scientific tools.
Table 1.
Some significant developments of modern scientific tools in Taiwan and Korea since 1950s.
| Time-line | Publications/Researchers | Significant developments |
|---|---|---|
| 1950s | Zhu Yan (China) |
|
| 1960s | Zhao-Fu, Fei (China) |
|
| 1976 | Shu-You, Wang (Taiwan) |
|
| 1984 | Ling-Yun, Wei (Taiwan) |
|
| 1987–1989 | Wei-Kung, Wang (Taiwan) |
|
| 2005–2012 | Chin-Ming, Huang (Taiwan) |
|
| 2013 | Korea Institute of Oriental Medicine, Daejeon (Korea) |
|
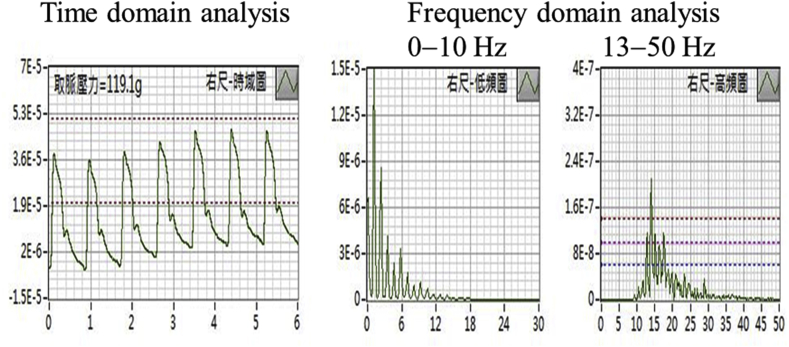
Both the time domain and frequency domain analyses are frequently used to investigate the radial pulse wave dynamics. The time domain analysis can investigate the amplitude and shape of the arterial waveform while the frequency domain analysis can determine the fluctuation of the spectral energy (SE) in the radial pulse waves. Fig. 2 illustrates a typical presentation of the time domain and frequency domain analyses in the pulse sphygmograph used in our study.
Fig. 2.
A typical presentation of the time domain and frequency domain analyses of the right Chi pulse.
Tsai et al. (2018) concluded that the time domain analysis provides a significant variation in the hemodynamic characteristics in the different radial pulse positions and indicators [10]. Moreover, Huang et al. (2011) investigated the radial pressure pulse parameters using the frequency domain analysis and reported a significant difference in SE at the Cun, Guan, and Chi pulses [11].
In this study, we focused our investigation on changes in RPPW during acupuncture intervention in low back pain (LBP) participants using the frequency domain analysis. Based on the Taiwan National Health Insurance 2016 statistical reports, dorsalgia ranked second for musculoskeletal and connective tissue diseases seen at all TCM outpatient clinics [12]. Globally, LBP ranked as the leading cause of years lived with disability in 2016 and has contributed 57.6 million years lived with disability, reported for 328 diseases and injuries in 195 countries [13].
Table 2 provides the classification of LBP based on syndrome-aetiology differentiation in TCM [14].
Table 2.
Classification of LBP based on syndrome-aetiology differentiation.
| Type of Syndrome | Syndrome Classification of LBP | Cause(s) | Pain Description |
|---|---|---|---|
| Repletion | 1. Cold damp syndrome | Cold and dampness |
|
| 2. Damp heat syndrome | Dampness and excessive heat |
|
|
| 3. Blood stasis syndrome | Blood stasis |
|
|
| Vacuity | 4. Kidney deficiency syndrome | Kidney Vacuity |
|
Differential diagnosis ultimately leads to different treatment strategies. In Chapter 17 of Huang Di Nei Jing, it is documented that ‘The lumbus represents the house of the kidneys’. To validate our hypothesis that acupuncture affects the Chi pulse (which reflects the kidney Qi) in LBP subjects more significantly than the other two pulse positions, we will investigate the high-frequency spectral energy in the radial pulse before and after acupuncture using the pulse sphygmograph. In addition, other objective and subjective assessments like the fingertip-to-floor (FTF) test and the Faces Pain Scale-Revised (FPS-R) test will be included to evaluate the effectiveness of the acupuncture intervention on LBP. The Oswestry Disability Index (ODI), the Health Status Questionnaire, and the Constitution in Chinese Medicine Questionnaire (CCMQ) will also be used to evaluate functional status and body constitution of each subject. The CCMQ was published by the China Association of Chinese Medicine in 2009 to assess the basic body constitution of the subjects based on TCM principles [15,16].
2. Materials and methods
2.1. Study design
This quasi-experimental study is a single arm, pre-post intervention study that integrates the concept of TCM and traditional acupuncture treatments with modern scientific tools. This type of nonrandomised, pre-post intervention design has been used before to evaluate the benefits of specific interventions in healthcare settings [17].
2.1.1. Protocol overview and setting
The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 checklist is being used to guide our study. Fig. 3 illustrates the flow diagram of the study and Table 3 provides the study schedule for enrolment, intervention, and outcome measurements.
Fig. 3.
The flow diagram of the study.
Table 3.
Study schedule for enrolment, intervention, and outcome measurements.
| STUDY PERIOD |
|||||
|---|---|---|---|---|---|
| Enrolment | Allocation | ||||
| TIMEPOINT | -t3 | -t2 | -t1 | 0 | t1 |
| ENROLMENT: | |||||
| Eligibility screen | X | ||||
| Informed consent | X | ||||
| Allocation | X | X | X | X | |
| INTERVENTIONS: | |||||
| Acupuncture | X | ||||
| ASSESSMENTS: | |||||
| Baseline Assessment: (1) Vital Signs (Body Temperature, Blood Pressure, Pulse rate) | X | X | X | ||
| Baseline Assessment: (2) Health Status Questionnaire | X | ||||
| Baseline Assessment: (3) Constitution in Chinese Medicine Questionnaire (CCMQ) | X | ||||
| Baseline Assessment: (4) Oswestry Disability Index (ODI) | X | ||||
| Baseline Assessment & Secondary Outcome measures: (5) Faces Pain Scale – Revised (FPS-R) | X | X | |||
|
Primary outcome measures: Radial Pressure Pulse-wave (RPPW) |
X | X | X | ||
|
Secondary Outcome measures: Range of Motion: Fingertip-to-Floor (FTF) test |
X | X | |||
The study will be conducted in the Acupuncture Department of the China Medical University Hospital (CMUH), Taichung, Taiwan with the approval of the CMUH Research Ethics Committee (REC) under protocol numbers CMUH107-REC2-022 and CMUH107-REC2-022 (AR-1). Recruitment will be promoted through advertisements on the hospital's websites, bulletin boards, advertisement tickers, and regular internal hospital circulars. The list of potential subjects will be consolidated, and the research assistant will contact the subjects to guide them through the informed consent process. Informed consent in the format approved by the REC will be explained and written consent will be obtained from the subjects. Subjects will be given the right to reject participation in the study at any time without prejudice to their medical care, and they will not be obliged to provide a reason for withdrawal. Eligible subjects will receive a session of acupuncture treatment in this intervention study.
2.1.2. Subjects and sample size
We will attempt to recruit 80 subjects to ensure a sufficient sample size for statistical analysis of the various types of LBP based on TCM syndrome differentiation. All subjects will receive the same intervention. Methods of randomisation and blinding will not be taken into consideration since this is a pre-post intervention study.
A previous study by Huang et al. (2012) reported a significant mean change in the spectral energy 13–50 Hz (SE13–50Hz) before and after acupuncture [8]. Kim et al. (2017) and Shin et al. (2016) had anticipated a 5% type 1 error, 80% power and 5% drop rates based on the mean change and standard deviation derived from Huang et al.‘s study [9,10]. They had estimated a sample size of 25 based on a single arm study without a control group. However, there is currently a lack of preceding data on the prevalence ratios of various types of LBP. Therefore, we estimate a sample size of 80 will be sufficient for statistical analysis using Huang et al.‘s (2012) study as a reference.
To be eligible in our study, subjects need to be at least 20 years old, of either gender, and with a chief complaint of LBP. They also need to be diagnosed with one of the following three types of LBP: lumbago (ICD-9-CM 724.2), lower back pain: loin pain, low back strain and lumbago not otherwise specified (NOS) (ICD-10-CM M54.5), or lumbago with sciatica (ICD-10-CM M54.4).
An identification code will be used in the evaluation forms, such as in the ODI, the Health Status Questionnaire, the CCMQ and the pulse assessment reports, to maintain the confidentiality of personal information. The list of subjects and identification codes will be maintained by the principal investigator. Subjects will be advised to avoid smoking or taking caffeinated drinks like coffee, tea or cola before treatment on the day of their acupuncture session.
Subjects with the following conditions will be excluded from our study: (a) subjects who are pregnant or lactating; (b) subjects with chronic heart failure, carcinomas under chemotherapy, psychological, or psychiatric disorders; (c) subjects with heart diseases and transplanted devices such as pacemakers; (d) subjects with acute infections such as upper respiratory infections, acute gastroenteritis, or urinary tract infections; (e) subjects unable to undergo evaluation with the pulse sphygmograph; (f) subjects with alcohol abuse or drug addiction; (g) subjects with communication disorders; (h) subjects who refuse to either provide informed consent or participate in the study; (i) subjects who are excluded at the principal investigator's discretion; (j) subjects who have participated in other clinical trials within the last three months; and (k) subjects who are allergic to metal.
2.2. Study procedure
Fig. 4 provides the study procedure and the estimated duration of the procedure.
Fig. 4.
Study procedure and the estimated duration of the procedure.
The baseline assessment and the objective and subjective evaluations will be conducted in an environment with an ambient temperature of 25 °C. These assessments are summarised in Table 4.
Table 4.
Baseline assessments and evaluations.
| Type of assessments | Objective | Subjective |
|---|---|---|
| Baseline Assessments |
|
|
| Primary outcome measure |
|
|
| Secondary outcome measures |
|
|
2.2.1. Baseline assessments
2.2.1.1. Vital signs
Vital signs including body temperature, systolic blood pressure, diastolic blood pressure and radial pulse rate will be assessed at the specified intervals before and after the acupuncture procedure. Vital signs (1) will serve as the baseline control at rest while the stability of vital signs (2) and (3) before and after the intervention will be compared.
2.2.1.2. The Health Status Questionnaire and the Constitution in Chinese Medicine Questionnaire (CCMQ)
Information of age, gender, body weight, body height, and health status will be obtained from each subject through the questionnaire. To analyse the various types of LBP, we will also gather additional information like the region of pain, type of pain and pain duration.
There are nine types of body constitution including Normality, Qi deficiency, Yin deficiency, Yang deficiency, Phlegm-dampness, Damp-heat, Blood stasis, Qi depressed and Inherited special constitutions. Each subject will answer seven to eight questions in each category. A higher score from the scoring algorithm indicates the likelihood of a specific type of body constitution. A 2013 study proved the validity, reliability, and responsiveness of the CCMQ in Hong Kong Chinese people [18]. The correlation between the body constitutions and the various types of LBP based on TCM syndrome differentiation will be evaluated.
2.2.1.3. The Oswestry Disability Index (ODI)
A Chinese 2.1 version of the ODI will be adopted. The ODI is one of the most common outcome measures of functional status used in the clinical management of spinal disorders [19,20].
2.2.2. Primary and secondary outcome measures
We will use the assessment of RPPW with a pulse sphygmograph at specific intervals before and after the acupuncture treatment as our primary outcome measure. The Cun, Guan and Chi pulse of both hands will be assessed with the subjects sitting in a comfortable position. Each pulse position will be marked on the wrists so that subsequent assessments can be applied consistently at the same location. The RPPW will be recorded when the best spectrogram displays the greatest amplitude. The electrical pulse signal received in the sensor is digitalised and processed through the Fast Fourier Transformation. A summation of the spectral energy in the 0–10 Hz (SE0–10Hz), 10–50 Hz (SE10–50Hz) and 13–50 Hz (SE13–50Hz) ranges will be obtained. Fig. 5 illustrates a typical graphical presentation of the pulse profile provided by the device.
Fig. 5.
A typical pulse profile provided by the pulse sphygmograph.
Pain and restricted spinal range of motion are frequently experienced by LBP patients. Hence, the following secondary outcome measures will be used to evaluate the effectiveness of the acupuncture treatment.
2.2.2.1. Range of motion: fingertip-to-floor (FTF) test
The FTF test will be conducted to evaluate flexibility in the range of motion before and after acupuncture. Subjects will be instructed to stand and bend forward as much as possible and attempt to reach the floor using their fingertips. The vertical distance from the index fingertip to the floor will be measured using a standard measuring tape. Ekedahl et al. (2012) suggested that the FTF test provides good validity in acute or subacute LBP [21]. Hence, this method will be adopted as an objective evaluation of the effectiveness of the acupoints.
2.2.2.2. Faces Pain Scale-Revised (FPS-R)
Pain intensity will be measured using the FPS-R developed by the International Association for the Study of Pain [22]. FPS-R is a self-reporting measure of pain intensity. A scale of six faces represented by 0, 2, 4, 6, 8 and 10 from left to right will be used. The 0 face denotes ‘no pain’ and the 10 face denotes ‘worst pain possible’. According to Miro et al. (2005), the FPS-R is the preferred tool to assess pain intensity in the elderly [23]. As we anticipate a number of elderly subjects with LBP in our study, we have adopted the FPS-R. Each subject will be asked to select the appropriate scale of pain before and after the intervention.
2.2.3. Acupuncture intervention
The subjects will be asked to lie in the prone position. Acupuncture needles will be perpendicularly inserted at the acupoints on the bladder meridian after the regions are disinfected with alcohol swabs. The acupoints of Shenshu (BL23), Dachangshu (BL25), and Weizhong (BL40) are located bilaterally in the lower back region based on the definition in the WHO Standard Acupuncture Point Locations in the Western Pacific Region [24]. The acupuncture needles will be inserted at the needle depth safety range of 0.5–1.5 cun (12.5–40 mm) for BL23, and 0.5–1 cun (12.5–25 mm) for BL25 and BL40 [25]. De qi (needling sensation) will be induced when inserting the needle and again 10 min after the insertion. The needles will be retained for 20 min before removal.
In the event that a subject experiences unbearable discomfort during the intervention, the study will be paused immediately and medical care will be given to the subject. The principal investigator will be informed to investigate the reason and decide whether to continue the study with the subject.
2.3. Devices and materials
Disposable, sterile, stainless steel acupuncture needles (0.22 mm × 30 mm, Yukuang Acupuncture Needles, Taiwan) will be used in the acupuncture intervention.
The following noninvasive devices will be adopted in the study for the baseline assessment and primary outcome measures before and after the intervention.
2.3.1. Pulse sphygmograph
The Huang-T1 Pulse Sphygmograph (Skylark Device and Systems Co., Ltd., Taiwan) will be used in this preliminary study to assess the feasibility of the protocol design. The study will be conducted with Asia Plus Pen Pulse Analysis System Model PPAS-96 (Asia Plus Bio Tech Co., Ltd, Taiwan) once the device becomes available upon approval from the Taiwan Food and Drug Administration.
The Huang-T1 Pulse Sphygmograph is a noninvasive device that digitalises the biological signal of RPPW and provides graphical analysis. It consists of a 3D pulse detector with a stable X-Y-Z axial movable framework. The electronic device contains a high precision pressure sensor, a filter, an amplifier and a signal recording card connected to signal analysis software. The frequency response is 0.1–50 Hz and the sampling rate is 3000 Hz. It was also used in the study by Huang et al. (2012) to investigate acupuncture effects on the radial pulse spectrum in dyspepsia [7].
The Asia Plus Pen Pulse Analysis System Model PPAS-96 is an upgraded design compared to the Huang-T1 Pulse Sphygmograph but without modification of the internal mechanical structure. It will facilitate a better operating experience for its users. The device consists of a high precision pressure sensor pen and a pulse analyser. Fig. 6 illustrates the two models of pulse sphygmograph used in the study.
Fig. 6.
Two models of the pulse sphymograph used in the study.
2.3.2. Terumo Digital Blood Pressure Monitor ES-P401
The systolic blood pressure, diastolic blood pressure, and pulse rate will be monitored using Terumo Digital Blood Pressure Monitor ES-P401 (Japan).
2.3.3. Exergen comfort scanner temporal thermometer
The Exergen Comfort Scanner Temporal Thermometer (USA) will be used to monitor the core body temperature by gently stroking across the temporal artery on the forehead. In a study comparing rectal temperature against temporal artery, tympanic and infrared skin temperature scans, it was reported that the mean difference compared to the rectal measurement was 0 °C, 0.49 °C and 0.34 °C respectively [26].
2.4. Data management and monitoring
The information of each subject will be maintained in individual spreadsheets in Microsoft Excel 2016. The data will then be consolidated into one final spreadsheet for comparison purposes. There will be no omission of data throughout the study. The results of all the assessments and evaluations will be digitalised and stored in USB flash drive with a secured password for at least three years before disposal by the principal investigator.
We anticipate that the study will be completed within the specified time approved by the REC and that no substantial safety issues will be encountered by the subjects. Therefore, a data monitoring committee will not be needed. Any adverse events or unintended effects of the intervention will be collected, assessed and reported immediately.
2.5. Hypothesis and statistical analyses
We hypothesise that (a) the SE13–50Hz in the RPPW of the Chi pulse in LBP subjects will be an effective indicator to evaluate the acupuncture treatment, and that (b) the FTF test and FPS-R test will show improvement after the acupuncture.
We will compare baseline characteristics such as gender, age, body mass index, vital signs, ODI, FPS-R, CCMQ, FTF, and the RPPW in various types of LBP. The results of the analysis will be presented as the means, standard deviations, 95% CIs, t-values and p-values using SAS statistical software (Version 9.4, SAS Institute, Cary, NC). The significance level for all tests will be set to 0.05 (two-sided). A paired t-test will be used to determine the significance of the change in RPPW induced by the acupuncture stimulation.
3. Discussion
In the development of evidence-based medicine, it is vital to produce clinical evidence from systematic research in TCM to facilitate its integration into a complete healthcare system together with western medicine [27]. Considerable effort has been taken by researchers to develop various modern scientific tools to map TCM's empirical knowledge to its scientific equivalents.
To our knowledge, this preliminary study is the first attempt to investigate the effects of acupuncture on RPPW in LBP subjects using a pulse sphygmograph and other modern tools. Our findings will enhance our understanding of the effectiveness of the selected acupuncture point combinations for treatment of LBP. In addition, we will be able to determine the prevalence of various types of LBP based on TCM syndrome differentiation in Taiwan. Although this quasi-experimental study is limited by its lack of random assignment and reduced internal validity, we have attempted to identify the threats to the validity of the findings and have addressed these in our study design. For instance, the same acupuncturist will apply the acupuncture at the same acupoint, and the baseline assessment of vital signs and pulse diagnosis will be used as a control to compare stability 20 and 30 min before the acupuncture intervention. We hope this preliminary study will provide a basic foundation for a large-scale research study that involves randomisation in the future.
Trial status
Recruitment of subjects is in progress.
Declarations
Ethics approval and consent to participate
This study protocol is approved by the CMUH REC, Taichung, Taiwan under protocol numbers CMUH107-REC2-022 and CMUH107-REC2-022 (AR-1). The final protocol version 1.4, dated 26 March 2018, will be used. This study has been registered at www.clinicaltrials.gov (NCT03501771) on 17 April 2018.
Important protocol modifications approved by the REC will be communicated to the relevant parties including the investigators and research staff through emails and meetings.
The study purpose, study procedures and potential risks of the study, including the provision of compensation to those who suffer harm from the trial, have been included in the informed consent form. Trial procedures will be explained to all subjects and they will be requested to endorse the informed consent form before participating in the study.
Availability of data and material
Not applicable.
Conflicts of interest
The authors declare there are no competing financial interests.
Funding
This work was partly supported by the Chinese Medicine Research Center, China Medical University [grant number CMRC-CHM-0].
Author contributions
HPN and CMH have contributed equally as first authors. HPN drafted this manuscript. HPN, YCL, and CMH are responsible for the protocol design and methodology. YCL and CMH will be responsible for the ultimate decision to terminate the trial and provide final approval of the manuscript. WCH will be responsible for the statistical analysis. All authors will have full access to the results of the study as well as the capacity to revise and approve the final manuscript.
Acknowledgements
This work was partly supported by the Chinese Medicine Research Center of China Medical University, Taiwan from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education in Taiwan (CMRC-CHM-0). We also acknowledge the support of CMUH for the use of its facilities. We would like to thank our research assistant, Ms. Paula Lu Wen-Chi, for the recruitment of participants, Mdm Mei-Jung Yen for her technical assistance in the pulse assessment, and all the participants for their collaboration.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2019.100384.
Contributor Information
Hui-Ping Ng, Email: huiping.ng@outlook.com.
Chin-Ming Huang, Email: huangcm1005@yahoo.com.tw.
Wen-Chao Ho, Email: wcho@mail.cmu.edu.tw.
Yu-Chen Lee, Email: d5167@mail.cmuh.org.tw.
Abbreviations
- CCMQ
Constitution in Chinese Medicine Questionnaire
- FPS-R
Faces Pain Scale-Revised
- FTF
fingertip-to-floor
- LBP
low back pain
- ODI
Oswestry Disability Index
- RPPW
radial pressure pulse waves
- TCM
Traditional Chinese Medicine
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Huang C.M. Zhi Yin Chu Ban She; Taiwan: 2015. Zhong Yi Mai Zhen Xue [Pulse Diagnosis in Traditional Chinese Medicine] [Google Scholar]
- 2.Hogeboom C.J., Sherman K.J., Cherkin D.C. Variation in diagnosis and treatment of chronic low back pain by traditional Chinese medicine acupuncturists. Complement. Ther. Med. 2001;9(3):154–166. doi: 10.1054/ctim.2001.0457. [DOI] [PubMed] [Google Scholar]
- 3.Coeytaux R.R., Chen W., Lindemuth C.E., Tan Y., Reilly A.C. Variability in the diagnosis and point selection for persons with frequent headache by traditional Chinese medicine acupuncturists. J. Altern. Complement. Med. 2006;12(9):863–872. doi: 10.1089/acm.2006.12.863. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y.G. TCM pulse contour analysis correlate first-derivative to frequency domain: on dr. Wang's stringy (Xian) pulse. J. Chin. Med. 2014;25(1):23–39. [Google Scholar]
- 5.Wei C.T.L.L.Y., Chow P. A New scientific method of pulse diagnosis. Am. J. Acupunct. 1984;12(3):205–218. [Google Scholar]
- 6.Wang Y.Y., Chang S.L., Wu Y.E., Hsu T.L., Wang W.K. Resonance. The missing phenomenon in hemodynamics. Circ. Res. 1991;69(1):246–249. doi: 10.1161/01.res.69.1.246. [DOI] [PubMed] [Google Scholar]
- 7.Huang C.M., Chang H.C., Li T.C., Chen C.C., Liao Y.T., Kao S.T. Acupuncture effects on the pulse spectrum of radial pressure pulse in dyspepsia. Am. J. Chin. Med. 2012;40(3):443–454. doi: 10.1142/S0192415X12500346. [DOI] [PubMed] [Google Scholar]
- 8.Huang C.M., Wei C.C., Liao Y.T., Chang H.C., Kao S.T., Li T.C. Developing the effective method of spectral harmonic energy ratio to analyze the arterial pulse spectrum, Evidence-based complementary and alternative medicine. eCAM. 2011;2011:342462. doi: 10.1093/ecam/neq054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bae J.-H., Jeon Y.J., Kim J.Y., Kim J.U. New assessment model of pulse depth based on sensor displacement in pulse diagnostic devices. Evid. Based Complement Altern. Med. 2013;2013:9. doi: 10.1155/2013/938641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai Y.-N., Chang Y.-H., Huang Y.-C., Jui-Shan Lin S., Lee S.-M., Cheng Y.-Y., Su Y.-C. The use of time-domain analysis on the choice of measurement location for pulse diagnosis research: a pilot study. J. Chin. Med. Assoc. 2018:1–9. doi: 10.1016/j.jcma.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Huang C.M., Chang H.C., Kao S.T., Li T.C., Wei C.C., Chen C.C., Chen F.J., Tsou S.S. Radial pressure pulse and heart rate variability in normotensive and hypertensive subjects. J. Altern. Complement. Med. 2011;17(10):945–952. doi: 10.1089/acm.2010.0326. [DOI] [PubMed] [Google Scholar]
- 12.MOHW National. Ministry of Health and Welfare; Taiwan: 2016. Health Isurance Statistical Report for Outpatient Clinics in 2016. [Google Scholar]
- 13.G.D.a.I.I.a.P. Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao H., Liu B.-y., Liu Z.-s., Xie L.-m., Fang Y.-g., Zhu Y., Li S.-n., Sun Y.-x., Han M.-j. Clinical practice guidelines of using acupuncture for low back pain. World J. Acupuncture-Moxibustion. 2016;26(4):1–13. [Google Scholar]
- 15.Wang Q., Zhu Y.B., Xue H.S., Li S. 2006. Primary Compiling of Constitution in Chinese Medicine Questionnaire. [Google Scholar]
- 16.Wang Q. Classification and diagnosis basis of nine basic constitutions in Chinese medicine. Journal of Beijing University of Traditional Chinese Medicine. 2005;28(4):1–8. [Google Scholar]
- 17.Harris A.D., McGregor J.C., Perencevich E.N., Furuno J.P., Zhu J., Peterson D.E., Finkelstein J. The use and interpretation of quasi-experimental studies in medical informatics. J. Am. Med. Inform. Assoc. : JAMIA. 2006;13(1):16–23. doi: 10.1197/jamia.M1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong W., Lam C.L.K., Wong V.T., Yang Z.M., Ziea E.T.C., Kwan A.K.L. Validation of the constitution in Chinese medicine Questionnaire: does the traditional Chinese medicine concept of body constitution exist?, evidence-based complementary and alternative medicine. eCAM. 2013;2013:481–491. doi: 10.1155/2013/481491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fritz J.M., Irrgang J.J. A comparison of a modified Oswestry low back pain disability Questionnaire and the Quebec back pain disability scale. Phys. Ther. 2001;81(2):776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 20.Lue Y.-J., Hsieh C.-L., Huang M.-H., Lin G.-T., Lu Y.-M. ODI 中文版 Chinese ODI. 2013;2 1. [Google Scholar]
- 21.Ekedahl H., Jonsson B., Frobell R.B. Fingertip-to-floor test and straight leg raising test: validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Arch. Phys. Med. Rehabil. 2012;93(12):2210–2215. doi: 10.1016/j.apmr.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 22.Hicks C.L., von Baeyer C.L., Spafford P.A., van Korlaar I., Goodenough B. The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain. 2001;93(2):173–183. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- 23.Miro J., Huguet A., Nieto R., Paredes S., Baos J. Evaluation of reliability, validity, and preference for a pain intensity scale for use with the elderly. J. Pain : official journal of the American Pain Society. 2005;6(11):727–735. doi: 10.1016/j.jpain.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 24.WHO, Xi Tai Ping Yang Di Qu . Chinese Medical Association of Acupuncture; Taiwan: 2010. WHO Biao Zhun Zhen Jiu Xue Wei [WHO Standards Acupuncture Point Locations in Western Pacific Region] [Google Scholar]
- 25.Lin J.-G. JYIN Publishing Company; Taiwan: 2009. Newly Edited Color Book of Acupuncture and Moxibustion. [Google Scholar]
- 26.Allegaert K., Casteels K., van Gorp I., Bogaert G. Tympanic, infrared skin, and temporal artery scan Thermometers compared with rectal measurement in children: a real-life assessment. Curr. Ther. Res. 2014;76:34–38. doi: 10.1016/j.curtheres.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fung F.Y., Linn Y.C. Developing traditional Chinese medicine in the era of evidence-based medicine: current evidences and challenges, evidence-based complementary and alternative medicine. eCAM. 2015;2015:425037. doi: 10.1155/2015/425037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.