Abstract
Background
Connective tissue disease associated with interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD) alone have same pathological and imaging backgrounds. However, the differences between lung cancer development and the mortality risk between these two conditions are unclear. Incidence of primary lung cancer and all-cause mortality were studied between interstitial lung disease patients with and without connective tissue disease.
Methods
Data were extracted from the Korean National Health Insurance Research Database in 2009. A total of 12,787 cases of ILD without idiopathic pulmonary fibrosis and 2491 cases of CTD-ILD were diagnosed in 2009. The cohort was followed up until June 30, 2014. Incident lung cancers and all-cause mortality were ascertained.
Results
The overall incidence of lung cancer was 165.7 and 161.8 per 10,000 person-years in the CTD-ILD and ILD-only, respectively (rate ratio, 1.08; 95% confidence interval, 0.89–1.30). CTD-ILD patients in the 40–49 and 50–59 years old age groups had lung cancer incidence rates of 92.5 and 139.2, which were 2.0 and 1.7 times higher than those in the ILD-only, respectively. All-cause mortality was significantly higher in the CTD-ILD group compared to ILD-only group in patients aged 50–79 years. All-cause mortality of women in the 50–59, 60–69 and 70–79 age groups was 2.0, 1.8, and 1.4 times higher in the CTD-ILD group than in the ILD-only group, respectively.
Conclusions
CTD-ILD patients aged < 60 years had a higher lung cancer incidence than ILD-only patients in the same age group. Furthermore, CTD-ILD patients aged 50–79 years had higher all-cause mortality than ILD-only patients in the same age group.
Keywords: Lung cancer, Connective tissue diseases, Interstitial lung disease, Mortality
Background
Connective tissue diseases (CTDs) can result in the development of pulmonary manifestations and considered as major organ involvement. CTD may be accompanied by interstitial lung disease (ILD) due to rheumatoid arthritis (RA) in 20–62% of cases [1–4], systemic lupus erythematosus in up to 70% of cases [5, 6], systemic sclerosis in 40–90% of cases [7, 8], and myositis in 20–66% of cases [9–11].
Various CTDs share similar lung pathologies [12]. The number of germinal centers associated with lymphocyte aggregation increases, and most inflammatory lesions in patients with CTD associated with interstitial lung disease (CTD-ILD) are distinct compared to those of patients with ILD alone (ILD-only) [13]. These findings suggest that diverse collagen vascular-related ILDs can be grouped into a single category termed CTD-ILD. CTD-ILD and ILD also share the same lung pathology spectrum [14]. In addition, certain forms of CTD-ILD also share genetic features with other interstitial lung abnormalities [15–17]. Although CTD-ILD with a nonspecific interstitial pneumonia (NSIP) pattern is the most prevalent form [18], no specific radiographic pattern identifies the disease [19].
Patients with CTD are also prone to developing lung cancer. Systemic sclerosis, dermatomyositis/polymyositis, rheumatoid arthritis, and a variety of CTDs have been associated with a high incidence of lung cancer [20–22]. Moreover, CTD-ILD is more often associated with lung cancer than CTD alone. Because patients with ILD alone also have a high lung cancer incidence [23, 24], controlling for ILD is important during evaluations of the lung cancer incidence in CTD-ILD patients.
To identify a meaningful number of patients with lung cancer from among those with orphan lung diseases (e.g., ILD), large data sets must be utilized, such as entire national insurance databases. Korea has only one health insurance system, the National Health Insurance (NHI) service. Inclusion of a large number of patients with CTD-ILD and ILD with follow-up data may allow investigation of the relationship between CTD-ILD and lung cancer according to age and sex after controlling for the effects of ILD alone.
Thus, this nationwide, 5-year, longitudinal, population-based study investigated the incidence of lung cancer and all-cause mortality among patients with CTD-ILD compared to those with ILD among patients without idiopathic pulmonary fibrosis (ILD-only) to help clarify the disease behavior.
Methods
Subjects
This closed longitudinal cohort study included data collected from the National Health Insurance (NHI) system based on the entire population. Since each citizen in Korea has a unique resident registration number, data duplication was avoided. The NHI service—the only public insurance system operated by the Ministry of Health and Welfare in Korea—is compulsory and covers the entire population, without exceptions for seasonal or part-time workers or unemployed persons [25]. The current study was approved by the institutional review board (IRB) at Dongsan Hospital, Keimyung University School of Medicine (IRB 2015–05-006). The IRB waived the requirement for informed consent.
Case identification
According to the National Statistical Office of Korea, the mid-year population of people ≥40 years of age in 2009 was 22,280,691. Patients with ILD only were selected as control subjects. Patients with CTD-ILD or ILD only between January and December 2009 were enrolled. The International Classification of Diseases, 10th revision (ICD-10) codes were used as a key reference not only for disease diagnosis but also within the NHI database.
Specific codes for each CTD and IPF (J84.1A) have been implemented by the NHI service since (2009). Patients classified under autoimmune diseases including CTD, IPF, and lung cancer are eligible for a copayment reduction from the NHI; this is in line with the government’s improved policy regarding enhanced support for orphan diseases since 2009. Specific code for primary lung cancer (C34) has been implemented since 2005. When a patient is registered with CTD, IPF, or lung cancer, the physician should send the necessary eligibility documents to the NHI.
The cases and controls were identified between January and December 2009 and were followed up until June 2014. The diagnostic codes for primary lung cancer cases diagnosed before 2009 were maintained on the NHI database. New lung cancer cases were identified by counting new cases registered during the calendar year after excluding preexisting lung cancer. We counted newly developed lung cancer cases and death after 1 month of recruiting CTD-ILD and ILD-only cases to exclude cases simultaneously diagnosed as both ILD and lung cancer.
Death were identified using the NHI database. Deceased person is dropped off insurance coverage.
Definitions of ILD-only and CTD-ILD
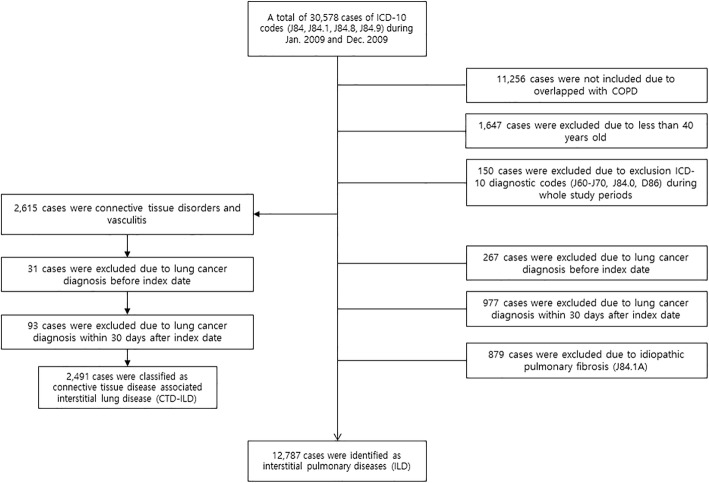
Based on the ICD-10 definitions, ILD-only was defined by code J84 for other ILD, excluding drug-induced ILD, interstitial emphysema, and lung diseases caused by external agents. In order to identify ILD without specific related diseases, connective tissue disease-associated ILD, hypersensitivity pneumonitis, sarcoidosis, and COPD were not included in the cohort. Code J84.x excluding J84.0, chronic pulmonary fibrosis due to inhalation of chemicals, gases, fumes, or vapors or that occurred following radiation therapy during the study period (Fig. 1).
Fig. 1.
Study flowchart. Flowchart of patient selection for CTD-ILD and ILD-only. COPD, chronic obstructive pulmonary disease; CTD-ILD, connective tissue disease-associated interstitial lung disease; ICD, International Classification of Disease; ILD, interstitial lung disease
The codes for identification of systemic CTD included M05 for rheumatoid arthritis, M07 for psoriatic and enteropathic arthropathies, M30 for polyarteritis, M31 for other necrotizing vasculopathies, M32 for systemic lupus erythematosus, M33 for dermatopolymyositis, M34 for systemic sclerosis, M35 for other systemic involvement of connective tissue, and M45 for ankylosing spondylitis. CTD-ILD was defined as any systemic CTD with J84 codes. In the ILD-only group, we excluded code J84.1A for idiopathic pulmonary fibrosis (IPF), which has been implemented since 2009, in much the same way as the new diagnostic criteria introduced in 2011 [26].
Data verification
Every patient with CTD, lung cancer, and IPF sends a document to the NHI that aligns with the diagnostic criteria of each CTD. All CTD patients registered in the NHI. All patients with cancer are registered in a separate national cancer database maintained by the National Cancer Center (NCC) and strictly validated before final registration. If patients change their lung cancer diagnosis, they are later dropped off from the cancer code.
Statistics
Age is reported using five-year units in the NHI data. We decided to divide the age groups by 10 years to account for the number of patients. The incidence rates of lung cancer per 10,000 person-years were calculated for patients with ILD with and without CTD according to the sex and age groups [27]. The incidence and mortality rates were compared as rate ratios (RRs) among different sex and age groups [28]. Kaplan-Meier curves were used to compare the development of lung cancer and all-cause mortality among patients with ILD with or without CTD. A sensitivity analysis was performed to assess the fragility of the results due to unmeasured confounding using the E-value methodology [29]. This E-value method estimates the minimum strength of association required between an unmeasured confounder and both the rate ratio of CTD-ILD to ILD-only and the risk of lung cancer development or mortality to overcome the statistically significant effect observed in a study where residual confounding is a potential problem (i.e., smoking). The reported P-values are two-sided, and those less than 0.05 are considered statistically significant. All analyses were performed using SPSS version 21 (IBM, Chicago, IL, USA) and the statistical software system R, version 3.5.2.
Results
Baseline demographics and follow-up duration
Women were predominant (71.1%) in the CTD-ILD group, whereas men were predominant (54.5%) in the ILD-only group. The median age was approximately 10 years less in patients with CTD-ILD compared to patients with ILD-only (Table 1). The median follow-up durations were 56.6 months (interquartile range [IQR], 48.3–64.9 months) and 54.8 months (IQR, 47.0–61.8 months) for the CTD-ILD and ILD-only groups, respectively.
Table 1.
Demographics of patients with connective tissue disease-associated with interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD)-only
| Characteristic | CTD-ILD (n = 2491), n (%) | ILD-only, n = 12,787), n (%) |
|---|---|---|
| Sex | ||
| Men | 721 (28.9) | 6969 (54.5) |
| Women | 1770 (71.1) | 5818 (45.5) |
| Age | ||
| Median (Q1, Q3) | 56 (51, 60) | 65 (55, 67) |
| 40–49 | 472 (18.9) | 1667 (13.0) |
| 50–59 | 685 (27.5) | 2679 (21.0) |
| 60–69 | 753 (30.2) | 3535 (27.6) |
| 70–79 | 493 (19.8) | 3446 (26.9) |
| ≥ 80 | 88 (3.5) | 1460 (11.4) |
Summarized based on the diagnosis at the top of the lists of International Statistical Classification of Diseases and Related Health Problems, 10th edition (ICD-10) codes of respiratory diseases
Lung cancer development in the CTD-ILD and ILD-only
A total of 165.7 and 161.8 lung cancer cases per 10,000 person-years were included in the CTD-ILD and ILD-only groups, respectively (Table 2). We evaluated the lung cancer incidence between the two groups based on age (40 to 59 years and greater than 60 years). Lung cancer was more common in CTD-ILD than in the ILD-only patients for age group 40 to 59 years (Fig. 2 and Table 2). The E values for the differences in the lung cancer incidence between the CTD-ILD and ILD-only groups were 3.59 in the age group 40 to 49 years and 2.87 in the age group 50 to 59 years (Fig. 3).
Table 2.
Lung cancer incidence per 10,000 person-years by age in patients with connective tissue disease-associated interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD)-only
| CTD-ILD | ILD-only | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Population (n) | Lung cancer cases (n) | Person-years of follow-up | Incidence | Population (n) | Lung cancer cases (n) | Person-years of follow-up | Incidence | RR | 95% CI | P value | E value |
| 40–49 | 472 | 19 | 2054.3 | 92.5 | 1667 | 28 | 6924.3 | 40.4 | 2.28 | 1.20–4.24 | 0.01 | 3.60 (1.00-NA) |
| 50–59 | 685 | 40 | 2873.7 | 139.2 | 2679 | 95 | 11,109.3 | 85.5 | 1.62 | 1.09–2.38 | 0.01 | 2.87 (1.43-NA) |
| 60–69 | 753 | 59 | 2988.0 | 197.5 | 3535 | 220 | 14,041.9 | 156.7 | 1.26 | 0.92–1.68 | 0.13 | |
| 70–79 | 493 | 41 | 1768.7 | 231.8 | 3446 | 258 | 12,371.2 | 208.5 | 1.11 | 0.77–1.55 | 0.57 | |
| > 80 | 88 | 6 | 271.4 | 221.1 | 1460 | 96 | 4232.2 | 226.8 | 0.97 | 0.34–2.20 | 1.00 | |
| Total | 2491 | 165 | 9956.1 | 165.7 | 12,787 | 697 | 48,679.0 | 143.2 | 1.15 | 0.97–1.37 | 0.10 | |
RR, rate ratio; CI, confidence interval; NA, not available; E value was calculated by VanderWeele and Ding method [29]
Fig. 2.
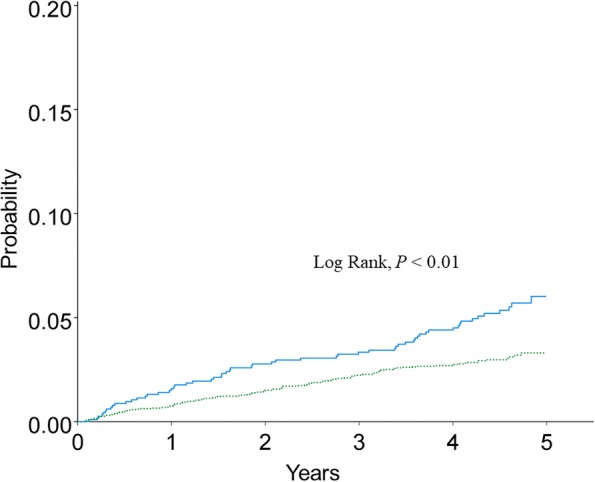
Kaplan-Meier curve for cumulative incidence of lung cancer below age 60 among the CTD-ILD (solid line) and ILD-only (dotted line). CTD-ILD connective tissue disease-associated interstitial lung disease, ILD-only interstitial lung disease
Fig. 3.
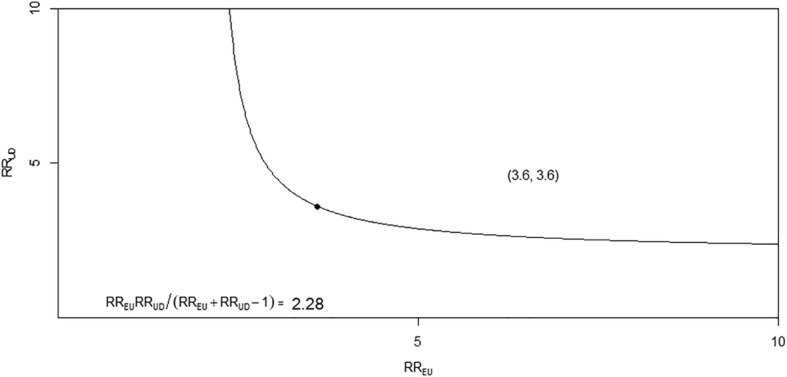
The minimum value required for the joint minimum strength of association of the risk ratio scale for an unmeasured confounder with the CTD-ILD and ILD-only groups to fully explain an observed treatment–outcome risk ratio of RR = 2.28 in the 40 to 49 years old age group. The E-value essentially sets the 2 parameters (RRUD and RREU) equal to each other to determine the required minimum for both values. The E-value estimate corresponds to the point (3.60, 3.60) in the 40 to 49 years old age group. RR, relative risk; E, exposure; U, unmeasured cofounder; D, outcome; RREU, maximum risk ratio for any specific level of the unmeasured confounders comparing the lung cancer incidence between the CTD-ILD and ILD-only; RRUD, maximum risk ratio for the outcome when comparing any 2 categories of the unmeasured confounders; CTD-ILD, connective tissue disease-associated interstitial lung disease; ILD-only, interstitial lung disease
Lung cancer development between the CTD-ILD and ILD-only according to sex and age
Among 40 to 49-years old men lung cancer incidence was more than three times higher in the CTD-ILD than in the ILD-only patients (Table 3). Among 50 to 59 years old women lung cancer incidence was more than two times higher in the CTD-ILD than in the ILD-only patients.
Table 3.
Lung cancer incidence per 10,000 person-years by sex and age in patients with connective tissue disease-associated interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD)-only
| Men | Women | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Incidence CTD-ILD | Incidence ILD Only | RR | 95% CI | P value | E value | Incidence CTD-ILD | Incidence ILD Only | RR | 95% CI | P value | E value |
| 40–49 | 161.7 | 48.8 | 3.23 | 1.11–9.39 | 0.03 | 5.91 (1.45-NA) | 77.2 | 41.2 | 1.91 | 0.63–5.81 | 0.25 | |
| 50–59 | 201.8 | 107.2 | 1.83 | 0.97–3.46 | 0.06 | 119.3 | 40.8 | 2.81 | 1.23–6.42 | 0.01 | 5.06 (1.76-NA) | |
| 60–69 | 294.2 | 286.4 | 1.02 | 0.67–1.54 | 0.90 | 152.2 | 83.1 | 1.78 | 0.99–3.18 | 0.05 | ||
| 70–79 | 352.3 | 288.8 | 1.20 | 0.75–1.93 | 0.43 | 170.6 | 129.1 | 1.31 | 0.74–2.32 | 0.35 | ||
| ≥ 80 | 414.3 | 424.9 | 1.00 | 0.36–2.77 | 0.99 | 114.4 | 318.0 | 0.43 | 0.10–1.78 | 0.24 | ||
| Total | 269.4 | 209.9 | 1.27 | 0.98–1.65 | 0.06 | 127.0 | 103.7 | 1.28 | 0.95–1.73 | 0.09 | ||
RR Rate ratio, CI confidence interval, NA not available, E value was calculated by VanderWeele and Ding method [29]
All-cause mortality in the CTD-ILD and ILD-only
The all-cause mortality rates were 347.1 and 351.1 cases per 10,000 person-years in the CTD-ILD and ILD-only groups, respectively (Table 4). In patients aged between 50 and 79 years, all-cause mortality was significantly higher in the CTD-ILD than in the ILD-only group (Table 4). Mean survival was 4.55 (95% confidence interval [CI], 4.53–4.57) years and 4.59 (95% CI, 4.54–4.63) years in the CTD-ILD and ILD-only groups, respectively (Fig. 4).
Table 4.
All-cause mortality per 10,000 person-years by age in patients with connective tissue disease-associated interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD)-only
| Age (years) | CTD-ILD | ILD-only | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population (n) | Deaths (n) | Person-years of follow-up | Mortality | Population (n) | Deaths (n) | Person-years of follow-up | Mortality | RR | 95% CI | P value | E value | |
| 40–49 | 472 | 21 | 2161.2 | 97.2 | 1667 | 54 | 7386.2 | 73.1 | 1.32 | 0.76–2.23 | 0.33 | |
| 50–59 | 685 | 59 | 3032.5 | 194.6 | 2679 | 149 | 11,785.1 | 126.4 | 1.53 | 1.11–2.09 | < 0.01 | 2.43 (1.45-NA) |
| 60–69 | 753 | 120 | 3208.8 | 374.0 | 3535 | 429 | 15,021.0 | 285.6 | 1.30 | 1.06–1.60 | 0.01 | 1.92 (1.31-NA) |
| 70–79 | 493 | 139 | 1990.8 | 698.2 | 3446 | 754 | 13,942.5 | 540.8 | 1.29 | 1.06–1.54 | < 0.01 | 1.90 (1.31-NA) |
| > 80 | 88 | 33 | 323.5 | 1020.1 | 1460 | 493 | 5386.4 | 915.3 | 1.11 | 0.75–1.58 | 0.59 | |
| total | 2491 | 372 | 10,716.9 | 347.1 | 12,787 | 1879 | 53,521.4 | 351.1 | 0.98 | 0.88–1.10 | 0.86 | |
RR Rate ratio, CI confidence interval, NA not available, E value was calculated by VanderWeele and Ding method [29]
Fig. 4.
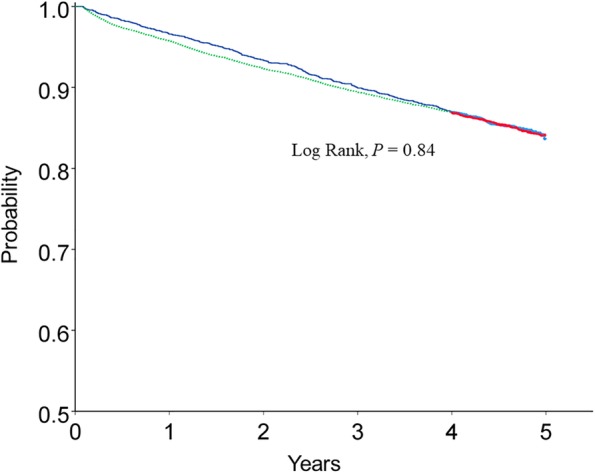
Kaplan-Meier curves for all-cause mortality for the CTD-ILD (solid line) and ILD-only (dotted line) patients. CTD-ILD connective tissue disease-associated interstitial lung disease; ILD-only interstitial lung disease
All-cause mortality between patients of both sexes in the CTD-ILD and ILD-only
Among men, the all-cause mortality rates were 468.0 and 394.4 cases per 10,000 person-years in the CTD-ILD and ILD-only groups, respectively. Among women, the all-cause mortality rates were 299.8 and 304.5 cases per 10,000 person-years in the CTD-ILD and ILD-only groups, respectively. Among men 40 to 49-years, the all-cause mortality rate was more than 1.5 times higher in the CTD-ILD than in the ILD-only group (Table 5). Among women aged 50 to 69 years, the all-cause mortality rate was approximately 1.8 to 2 times higher in the CTD-ILD than in the ILD-only group (Table 6).
Table 5.
All-cause mortality per 10,000 person-years by age in patients with connective tissue disease-associated interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD)-only in men
| Age (years) | CTD-ILD | ILD-only | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Population (n) | Deaths (n) | Person-years of follow-up | Mortality | Population (n) | Deaths (n) | Person-years of follow-up | Mortality | RR | 95% CI | P value | |
| 40–49 | 90 | 7 | 401.5 | 174.3 | 1002 | 38 | 4433.6 | 85.7 | 2.03 | 0.76–4.61 | 0.15 |
| 50–59 | 170 | 20 | 743.6 | 269.0 | 1559 | 107 | 6805.0 | 157.2 | 1.71 | 1.00–2.77 | 0.04 |
| 60–69 | 254 | 49 | 1054.7 | 464.6 | 2019 | 309 | 8418.7 | 367.0 | 1.26 | 0.97–1.71 | 0.15 |
| 70–79 | 172 | 52 | 686.9 | 757.0 | 1795 | 441 | 7176.5 | 614.5 | 1.23 | 0.90–1.64 | 0.18 |
| > 80 | 35 | 13 | 126.3 | 1029.1 | 594 | 235 | 2091.1 | 1123.8 | 0.91 | 0.48–1.59 | 0.89 |
| total | 721 | 141 | 3013.0 | 468.0 | 6969 | 1130 | 28,925.1 | 390.7 | 1.19 | 0.99–1.42 | 0.05 |
RR, Rate ratio; CI, confidence interval
Table 6.
All-cause mortality per 10,000 person-years by age in patients with connective tissue disease-associated interstitial lung disease (CTD-ILD) and interstitial lung disease (ILD)-only in women
| Age (years) | CTD-ILD | ILD-only | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population (n) | Deaths (n) | Person-years of follow-up | Mortality | Population (n) | Deaths (n) | Person-years of follow-up | Mortality | RR | 95% CI | P value | E value | |
| 40–49 | 382 | 14 | 1759.9 | 79.5 | 665 | 16 | 2952.5 | 54.2 | 1.46 | 0.66–3.20 | 0.38 | |
| 50–59 | 515 | 39 | 2289.4 | 170.4 | 1120 | 42 | 4980.1 | 84.3 | 2.01 | 1.27–3.20 | < 0.01 | 3.43 (1.85-NA) |
| 60–69 | 499 | 71 | 2154.8 | 329.5 | 1516 | 120 | 6602.2 | 181.8 | 1.81 | 1.33–2.45 | < 0.01 | 3.02 (1.99-NA) |
| 70–79 | 321 | 87 | 1304.2 | 667.1 | 1651 | 313 | 6766.0 | 462.6 | 1.44 | 1.12–1.83 | < 0.01 | 2.23 (1.48-NA) |
| > 80 | 53 | 20 | 197.2 | 1014.2 | 866 | 258 | 3295.2 | 783.0 | 1.29 | 0.77–2.04 | 0.32 | |
| total | 1770 | 231 | 7705.7 | 299.8 | 5818 | 749 | 24,596.3 | 304.5 | 0.98 | 0.84–1.14 | 0.86 | |
RR Rate ratio, CI, confidence interval, NA not available, E value was calculated by VanderWeele and Ding method [29]
Discussion
An increased lung cancer incidence in CTD-ILD patients compared to that in ILD-only patients was observed among those aged < 60 years. The lung cancer incidence rate ratios in men and women were 27 and 28%, respectively, in the CTD-ILD patients, which were higher than those with ILD-only. In 40 to 49 years old men lung cancer risk was 3.2 times higher for CTD-ILD patients than for those with ILD-only. The lung cancer risk for women in the 50 to 59 years age group was 2.8 times higher for CTD-ILD patients than for ILD-only patients. Although we could not exclude unmeasured confounders to eliminate the possibility of spurious results in these age groups, this result suggested that the mechanisms underlying enhanced lung cancer development in CTD-ILD patients involved a younger age for both men and women.
We previously reported the epidemiology of lung cancer in CTD-ILD, ILD, and idiopathic pulmonary fibrosis (IPF) patients [23, 30]. However, the number of lung cancer patients was small, and the data used to compare the lung cancer prevalence between the CTD-ILD and ILD-only groups were unstable [30]. Therefore, the previous study did not clearly show a difference in the lung cancer prevalence between the CTD-ILD and ILD-only. However, the other study demonstrated the lung cancer risk for IPF patients was significantly higher than ILD patients [23]. The present study included a whole national population that was followed for up to 5 years, which might have helped detect a significant difference in the lung cancer incidence between the CTD-ILD and ILD-only patients.
The incidence of lung cancer is high in men with RA [31–33]. In line with these studies, the present study shows that the lung cancer incidence was approximately two times higher in ILD irrespective of gender.
One objective of this study was to estimate the contribution of CTD to lung cancer development. In the younger age group (40 to 49 years), the lung cancer risk was 2.3 times higher in the CTD-ILD than in the ILD-only group, but the risk decreases with age. This phenomenon is commonly observed in both men and women. Based on these results, the following hypotheses can be considered. First, lung cancer development potential due to autoimmune responses is reduced as the patient ages. The second hypothesis is that autoimmunity combined with other factors contributes to an increased risk of lung cancer development at a young age. Third, the development of autoimmune lung disease related cancer may overlap with other powerful lung cancer-causing factors, such as the aging process; thus, lung cancer risk related to autoimmunity can be neglected.
The presence of fibrosing interstitial pneumonia in RA patients is associated with a lower survival rate than that of RA alone [34], and CTD-ILD has a poorer prognosis than idiopathic interstitial pneumonia [19]. ILD-only also revealed higher mortality than non-ILD control [35]. In contrast, several studies have shown opposite or neutral results in relation to survival [36–40]. In this population-based closed cohort study, aged between 50 to 79 years, mortality was higher in the CTD-ILD than the ILD-only group, especially for women.
Study limitations
We could not control for the confounding effects of unmeasured smoking on the development of lung cancer, because the NHI database did not include smoking history data. ILD carries an increased risk of lung cancer, even after correcting for or considering the smoking status [30, 41]. The odds ratio of smoking for lung cancer development in CTD-ILD patients was reported to be 1.2 [42]. The use of immunosuppressants for CTD-ILD may also increase the incidence of lung cancer [42]. Although we also did not control for the confounding effects of immunosuppressants in this study, immunosuppressants are tightly related to de novo malignancy [43, 44]. In this study, because no general population control without ILD was included, we could not measure the true magnitude of the effect of ILD on lung cancer development.
We identified CTD-ILD based on the ICD-10 code. However, no specific ICD-10 code is available for CTD-ILD, and no clear consensus diagnosis exists concerning what constitutes CTD-ILD based on the ICD-10 code. Additionally, the ICD-10 code does not include histological findings. The patient data are anonymized, which makes it impossible to trace information back to a medical record. Therefore, we did not perform further analyses according to lung cancer histology.
We excluded patients with a diagnosis of lung cancer before and 1 month after the index date. However, patients with lung cancer could be miscounted due to the occurrence of new cases in the early period of the cohort. Additionally, other risk factors, such as pulmonary function and high-resolution computed tomography (CT) findings for ILD, could not be evaluated, because the NHI primarily included medical claims.
Conclusions
We observed increased lung cancer incidence in younger (less than 60 years old) patients with CTD-ILD when compared to ILD-only. In addition, we found that all-cause mortality rate was higher in older CTD-ILD patients (50 to 79 years old) than in those ILD-only, especially in women. These results imply that a physician may pay more attention to lung cancer screening and management strategies for CTD-ILD patients.
Acknowledgements
We would like to thanks to Ms. Byeong Ju Park for the preparing data sets.
Abbreviations
- CT
Computed tomography
- CTD
Connective tissue disease
- ICD
International classification of disease
- ILD
Interstitial lung disease
- IPF
Idiopathic pulmonary fibrosis
- NCC
National cancer center
- NHI
National health insurance
- RA
Rheumatoid arthritis
Authors’ contributions
All authors have contributed either to the conception, original hypothesis, and design of the cohort. All authors have contributed to the writing and revisions of this article. Data acquisition was performed by CWL. and WIC., and analysis was performed by DYL, HJC, W-IC., and CWL. All authors had full access to all the data in the study. WIC. had final responsibility for the integrity of the data and the accuracy of the data analysis and the decision to submit for publication. All authors read and approved the final manuscript.
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIP) (No. 2014R1A5A2010008). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets supporting the conclusion of this article is not available due to National Health Insurance data management policy.
Ethics approval and consent to participate
The current study was approved by the institutional review board at Dongsan Hospital, Keimyung University School of Medicine (2015–05-006). The need for written informed consent was waived. This study was conducted in compliance with the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors state that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Won-Il Choi, Phone: +820532507996, Email: wichoi@dsmc.or.kr.
Dong Yoon Lee, Email: yardsticklee@gmail.com.
Hyun-Gi Choi, Email: jin9121@naver.com.
Choong Won Lee, Email: prevmi@gmail.com.
References
- 1.Gochuico BR, Avila NA, Chow CK, Novero LJ, Wu HP, Ren P, MacDonald SD, Travis WD, Stylianou MP, Rosas IO. Progressive preclinical interstitial lung disease in rheumatoid arthritis. Arch Intern Med. 2008;168:159–166. doi: 10.1001/archinternmed.2007.59. [DOI] [PubMed] [Google Scholar]
- 2.Dawson JK, Fewins HE, Desmond J, Lynch MP, Graham DR. Fibrosing alveolitis in patients with rheumatoid arthritis as assessed by high resolution computed tomography, chest radiography, and pulmonary function tests. Thorax. 2001;56:622–627. doi: 10.1136/thorax.56.8.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabbay E, Tarala R, Will R, Carroll G, Adler B, Cameron D, Lake FR. Interstitial lung disease in recent onset rheumatoid arthritis. Am J Respir Crit Care Med. 1997;156:528–535. doi: 10.1164/ajrccm.156.2.9609016. [DOI] [PubMed] [Google Scholar]
- 4.Bilgici A, Ulusoy H, Kuru O, Celenk C, Unsal M, Danaci M. Pulmonary involvement in rheumatoid arthritis. Rheumatol Int. 2005;25:429–435. doi: 10.1007/s00296-004-0472-y. [DOI] [PubMed] [Google Scholar]
- 5.Orens JB, Martinez FJ, Lynch JP., 3rd Pleuropulmonary manifestations of systemic lupus erythematosus. Rheum Dis Clin N Am. 1994;20:159–193. [PubMed] [Google Scholar]
- 6.Fenlon HM, Doran M, Sant SM, Breatnach E. High-resolution chest CT in systemic lupus erythematosus. AJR Am J Roentgenol. 1996;166:301–307. doi: 10.2214/ajr.166.2.8553934. [DOI] [PubMed] [Google Scholar]
- 7.Steen VD, Medsger TA. Changes in causes of death in systemic sclerosis, 1972-2002. Ann Rheum Dis. 2007;66:940–944. doi: 10.1136/ard.2006.066068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schurawitzki H, Stiglbauer R, Graninger W, Herold C, Polzleitner D, Burghuber OC, Tscholakoff D. Interstitial lung disease in progressive systemic sclerosis: high-resolution CT versus radiography. Radiology. 1990;176:755–759. doi: 10.1148/radiology.176.3.2389033. [DOI] [PubMed] [Google Scholar]
- 9.Chen IJ, Jan Wu YJ, Lin CW, Fan KW, Luo SF, Ho HH, Liou LB, Tsai WP, Chen JY, Yang CH, et al. Interstitial lung disease in polymyositis and dermatomyositis. Clin Rheumatol. 2009;28:639–646. doi: 10.1007/s10067-009-1110-6. [DOI] [PubMed] [Google Scholar]
- 10.Hayashi S, Tanaka M, Kobayashi H, Nakazono T, Satoh T, Fukuno Y, Aragane N, Tada Y, Koarada S, Ohta A, Nagasawa K. High-resolution computed tomography characterization of interstitial lung diseases in polymyositis/dermatomyositis. J Rheumatol. 2008;35:260–269. [PubMed] [Google Scholar]
- 11.Kang EH, Lee EB, Shin KC, Im CH, Chung DH, Han SK, Song YW. Interstitial lung disease in patients with polymyositis, dermatomyositis and amyopathic dermatomyositis. Rheumatology (Oxford) 2005;44:1282–1286. doi: 10.1093/rheumatology/keh723. [DOI] [PubMed] [Google Scholar]
- 12.Fischer A, du Bois R. Interstitial lung disease in connective tissue disorders. Lancet. 2012;380:689–698. doi: 10.1016/S0140-6736(12)61079-4. [DOI] [PubMed] [Google Scholar]
- 13.Song JW, Do KH, Kim MY, Jang SJ, Colby TV, Kim DS. Pathologic and radiologic differences between idiopathic and collagen vascular disease-related usual interstitial pneumonia. Chest. 2009;136:23–30. doi: 10.1378/chest.08-2572. [DOI] [PubMed] [Google Scholar]
- 14.American Thoracic S, European Respiratory S. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS executive committee, June 2001. Am J Respir Crit Care Med. 2002;165:277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 15.Juge PA, Lee JS, Ebstein E, Furukawa H, Dobrinskikh E, Gazal S, Kannengiesser C, Ottaviani S, Oka S, Tohma S, et al. MUC5B promoter variant and rheumatoid arthritis with interstitial lung disease. N Engl J Med. 2018;379:2209–2219. doi: 10.1056/NEJMoa1801562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunninghake GM, Hatabu H, Okajima Y, Gao W, Dupuis J, Latourelle JC, Nishino M, Araki T, Zazueta OE, Kurugol S, et al. MUC5B promoter polymorphism and interstitial lung abnormalities. N Engl J Med. 2013;368:2192–2200. doi: 10.1056/NEJMoa1216076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Albert RK, Schwartz DA. Revealing the secrets of idiopathic pulmonary fibrosis. N Engl J Med. 2019;380:94–96. doi: 10.1056/NEJMcibr1811639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Travis WD, Costabel U, Hansell DM, King TE, Jr, Lynch DA, Nicholson AG, Ryerson CJ, Ryu JH, Selman M, Wells AU, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kocheril SV, Appleton BE, Somers EC, Kazerooni EA, Flaherty KR, Martinez FJ, Gross BH, Crofford LJ. Comparison of disease progression and mortality of connective tissue disease-related interstitial lung disease and idiopathic interstitial pneumonia. Arthritis Rheum. 2005;53:549–557. doi: 10.1002/art.21322. [DOI] [PubMed] [Google Scholar]
- 20.Onishi A, Sugiyama D, Kumagai S, Morinobu A. Cancer incidence in systemic sclerosis: meta-analysis of population-based cohort studies. Arthritis Rheum. 2013;65:1913–1921. doi: 10.1002/art.37969. [DOI] [PubMed] [Google Scholar]
- 21.Takayanagi N, Tokunaga D, Tsuchiya Y, Miyahara Y, Ishiguro T, Yamaguchi S, Saito H, Ubukata M, Kurashima K, Yanagisawa T, et al. Lung cancer associated with rheumatoid arthritis and usual interstitial pneumonia. Nihon Kokyuki Gakkai Zasshi. 2008;46:438–442. [PubMed] [Google Scholar]
- 22.Adzic TN, Pesut DP, Nagorni-Obradovic LM, Stojsic JM, Vasiljevic MD, Bouros D. Clinical features of lung cancer in patients with connective tissue diseases: a 10-year hospital based study. Respir Med. 2008;102:620–624. doi: 10.1016/j.rmed.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 23.Choi WI, Park SH, Park BJ, Lee CW. Interstitial lung disease and lung Cancer development: a 5-year Nationwide population-based study. Cancer Res Treat. 2018;50:374–381. doi: 10.4143/crt.2017.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naccache JM, Gibiot Q, Monnet I, Antoine M, Wislez M, Chouaid C, Cadranel J. Lung cancer and interstitial lung disease: a literature review. J Thorac Dis. 2018;10:3829–3844. doi: 10.21037/jtd.2018.05.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim KS, Lee YJ. Developments and general features of national health insurance in Korea. Soc Work Public Health. 2010;25:142–157. doi: 10.1080/19371910903547017. [DOI] [PubMed] [Google Scholar]
- 26.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Szklo M, Nieto FJ: Epidemiology: Beyond the Basics. . Jones & Bartlett Learning Burlington; 2014.
- 28.A language and environment for statistical computing [http://www.R-project.org].
- 29.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–274. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- 30.Jung HI, Park JS, Lee MY, Park B, Kim HJ, Park SH, Choi WI, Lee CW. Prevalence of lung cancer in patients with interstitial lung disease is higher than in those with chronic obstructive pulmonary disease. Medicine (Baltimore) 2018;97:e0071. doi: 10.1097/MD.0000000000010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamada T, Nakajima A, Inoue E, Tanaka E, Taniguchi A, Momohara S, Yamanaka H. Incidence of malignancy in Japanese patients with rheumatoid arthritis. Rheumatol Int. 2011;31:1487–1492. doi: 10.1007/s00296-010-1524-0. [DOI] [PubMed] [Google Scholar]
- 32.Abasolo L, Judez E, Descalzo MA, Gonzalez-Alvaro I, Jover JA, Carmona L, Group ES Cancer in rheumatoid arthritis: occurrence, mortality, and associated factors in a south European population. Semin Arthritis Rheum. 2008;37:388–397. doi: 10.1016/j.semarthrit.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 33.Thomas E, Brewster DH, Black RJ, Macfarlane GJ. Risk of malignancy among patients with rheumatic conditions. Int J Cancer. 2000;88:497–502. doi: 10.1002/1097-0215(20001101)88:3<497::AID-IJC27>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 34.Solomon JJ, Ryu JH, Tazelaar HD, Myers JL, Tuder R, Cool CD, Curran-Everett D, Fischer A, Swigris JJ, Brown KK. Fibrosing interstitial pneumonia predicts survival in patients with rheumatoid arthritis-associated interstitial lung disease (RA-ILD) Respir Med. 2013;107:1247–1252. doi: 10.1016/j.rmed.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Choi WI, Park SH, Dauti S, Park BJ, Lee CW. Interstitial lung disease and risk of mortality: 11-year nationwide population-based study. Int J Tuberc Lung Dis. 2018;22:100–105. doi: 10.5588/ijtld.17.0167. [DOI] [PubMed] [Google Scholar]
- 36.Park JH, Kim DS, Park IN, Jang SJ, Kitaichi M, Nicholson AG, Colby TV. Prognosis of fibrotic interstitial pneumonia: idiopathic versus collagen vascular disease-related subtypes. Am J Respir Crit Care Med. 2007;175:705–711. doi: 10.1164/rccm.200607-912OC. [DOI] [PubMed] [Google Scholar]
- 37.Koduri G, Norton S, Young A, Cox N, Davies P, Devlin J, Dixey J, Gough A, Prouse P, Winfield J, et al. Interstitial lung disease has a poor prognosis in rheumatoid arthritis: results from an inception cohort. Rheumatology (Oxford) 2010;49:1483–1489. doi: 10.1093/rheumatology/keq035. [DOI] [PubMed] [Google Scholar]
- 38.Song JW, Lee HK, Lee CK, Chae EJ, Jang SJ, Colby TV, Kim DS. Sarcoidosis Vasc diffuse lung dis. 2013. Clinical course and outcome of rheumatoid arthritis-related usual interstitial pneumonia; pp. 103–112. [PubMed] [Google Scholar]
- 39.Moua T, Zamora Martinez AC, Baqir M, Vassallo R, Limper AH, Ryu JH. Predictors of diagnosis and survival in idiopathic pulmonary fibrosis and connective tissue disease-related usual interstitial pneumonia. Respir Res. 2014;15:154. doi: 10.1186/s12931-014-0154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hubbard R, Venn A. The impact of coexisting connective tissue disease on survival in patients with fibrosing alveolitis. Rheumatology (Oxford) 2002;41:676–679. doi: 10.1093/rheumatology/41.6.676. [DOI] [PubMed] [Google Scholar]
- 41.Hubbard R, Venn A, Lewis S, Britton J. Lung cancer and cryptogenic fibrosing alveolitis. A population-based cohort study. Am J Respir Crit Care Med. 2000;161:5–8. doi: 10.1164/ajrccm.161.1.9906062. [DOI] [PubMed] [Google Scholar]
- 42.Watanabe S, Saeki K, Waseda Y, Murata A, Takato H, Ichikawa Y, Yasui M, Kimura H, Hamaguchi Y, Matsushita T, et al. Lung cancer in connective tissue disease-associated interstitial lung disease: clinical features and impact on outcomes. J Thorac Dis. 2018;10:799–807. doi: 10.21037/jtd.2017.12.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gutierrez-Dalmau A, Campistol JM. Immunosuppressive therapy and malignancy in organ transplant recipients: a systematic review. Drugs. 2007;67:1167–1198. doi: 10.2165/00003495-200767080-00006. [DOI] [PubMed] [Google Scholar]
- 44.Kauffman HM, Cherikh WS, McBride MA, Cheng Y, Hanto DW. Post-transplant de novo malignancies in renal transplant recipients: the past and present. Transpl Int. 2006;19:607–620. doi: 10.1111/j.1432-2277.2006.00330.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusion of this article is not available due to National Health Insurance data management policy.