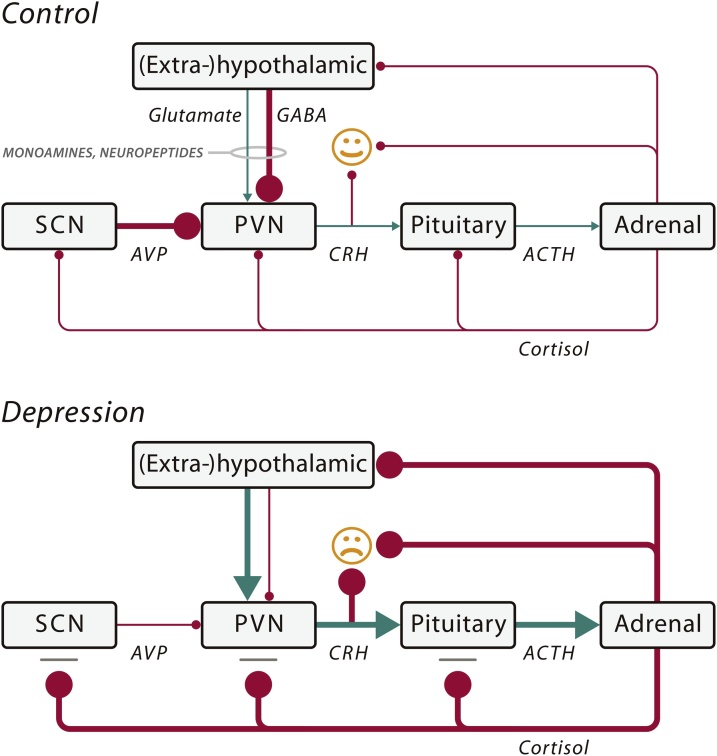
Fig. 1.
Schematic illustration of some of the key mechanisms that may cause a mood disorder by impaired input of neurotransmitters (monoamines and amino acids) and/or neuropeptides (arginine vasopressin (AVP), oxytocin (OXT)) on the hypothalamo–pituitary– adrenal (HPA) axis. In the control situation (normal mood), the corticotropinreleasing hormone (CRH) neurons of the stress axis (HPA axis) are inhibited by a γ-aminobutyric acid (GABA)-ergic input from (extra-)hypothalamic areas and by an AVP input from the suprachiasmatic nucleus (SCN). Some monoamines and neuropeptides (e.g., OXT) also inhibit the HPA axis. When there is depression, the HPA axis is activated by: (1) diminished GABAergic input; and/or (2) increased glutaminergic input from (extra-)hypothalamic sites; and/or (3) diminished inhibition by the SCN; and/or (4) stimulatory influence on the HPA axis by alterations in the monoamine or neuropeptide input; and/or (5) a deficient cortisol feedback effect due to the presence of glucocorticoid resistance. The resulting disinhibition of the paraventricular nucleus (PVN) causes a chronic rise in CRH and cortisol levels in depression, which causes mood changes through their action on the brain. The hyperactivity of the HPA axis may be due to a multitude of risk factors such as genetic polymorphisms, development sequelae, and environmental factors. A decreased amount of AVP mRNA of the SCN was found in depression, which seems to be the basis of the impaired circadian regulation of the HPA system in depression and a decreased inhibition of CRH neurons. Arrow: stimulation; Bar with ball-head: inhibition. The thickness of the lines indicates the strength of the effects. ACTH, adrenocorticotropic hormone. Modified from Fig. 1 of (Bao et al., 2012).