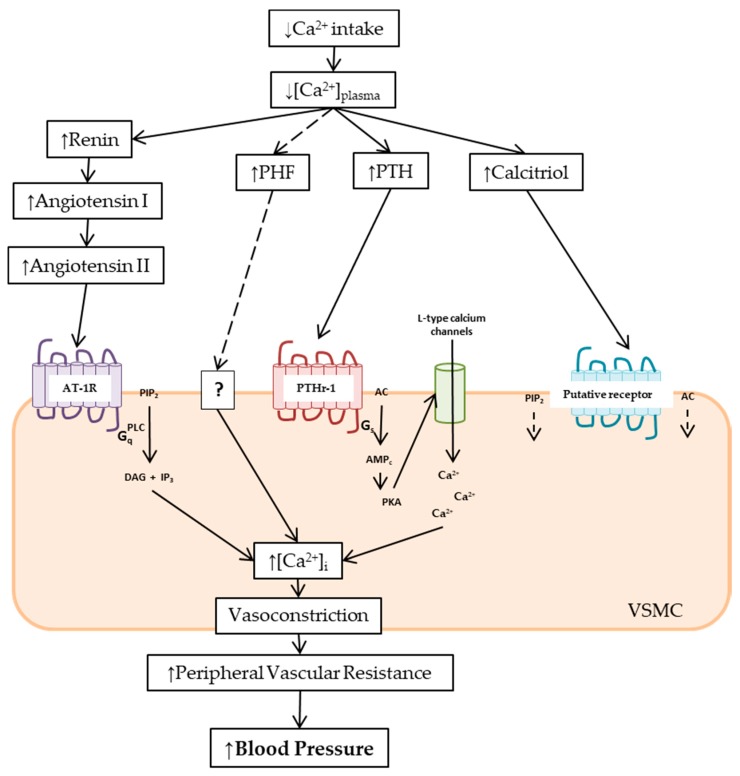
Figure 1.
Scheme of the mechanisms involved in the rise of blood pressure in low calcium intake by an increase in peripheral vascular resistance. Low calcium intake decreases plasmatic calcium concentration ([Ca2+]plasma), stimulating the release of parathyroid hormone (PTH) and parathyroid hypertensive factor (PHF), the synthesis of calcitriol, and the activation of the renin–angiotensin–aldosterone system (RAAS). In vascular smooth muscle cells (VSMC), angiotensin II via the angiotensin II type I receptor (AT1R)/Gq/phospholipase C (PLC)/inositol trisphosphate (IP3) pathway, PTH via PTHr-1/Gs/3′,5′-cyclic adenosine monophosphate (cAMP)/protein kinase A (PKA), and calcitriol via adenylate cyclase (AC)/cAMP/PKA and PLC/IP3 signaling pathways increased the intracellular calcium concentration ([Ca2+]i). The rise of [Ca2+]i leads to vasoconstriction, and hence increases in peripheral vascular resistance and blood pressure. The PHF mechanism of action remains unknown. See text for further details.