Short abstract
Objective
We herein introduce a staged management protocol for AO/OTA type 43-C3.3 pilon fractures based on the four-column theory designed to protect the soft tissue.
Methods
Twenty-three patients with 25 type C3.3 pilon fractures underwent a staged procedure with four-column osteosynthesis from April 2014 to December 2016. The first stage involved immediate calcaneal traction or external fixation to span the ankle joint. When the soft tissue swelling decreased, the posterolateral approach was used to restore the lateral column and initially fix the posterior column. After 10 to 12 days, the third stage involved treatment of the anterior and medial columns through the anterior approach. Charts and radiographs were reviewed, and the American Orthopaedic Foot and Ankle Society (AOFAS) evaluation system was used to evaluate the postoperative outcomes.
Results
All fractures achieved union after a mean of 3.3 months (range, 2.0–5.7 months) after the third stage. A good or acceptable reduction rate was observed in 85.7% of the patients. Results from the AOFAS evaluation system indicated excellent or good postoperative ankle function in 81.0% of the patients.
Conclusion
This staged procedure protocol combined with the four-column theory is a feasible way to protect the soft tissue and reduce the fracture.
Keywords: Pilon, staged procedure, four-column concept, fracture, soft tissue, ankle
Introduction
A pilon fracture is a severe ankle fracture involving the articular surface with proximal extension.1 Pilon injury accounts for about 5% to 7% of all tibial fractures, and the incidence rate is relatively low. However, with the high incidence of high-energy trauma and accidental falls, the number of comminuted fractures has increased in recent years.2 Most complex pilon fractures are associated with severe soft tissue injuries, making the treatment challenging.
Optimal treatment of comminuted pilon fractures requires precise anatomical reduction accompanied by early functional exercise. However, this ideal is often hindered by many factors, such as infection, wound necrosis, and loss of bone mass, which result in poor treatment outcomes or even failure.3,4 Several methods have been advocated to manage complex pilon fractures, but an optimal fixation technique remains controversial. Some researchers prefer to use an external fixator to avoid soft tissue complications. However, external fixators are associated with pin-tract infection and other postoperative complications, such as nonunion, malunion, and a longer union time.
The two-stage procedure for fracture treatment involves external fixation in the first stage and conversion to internal fixation in the second stage. This technique has been successfully popularized in the treatment of severe pilon fractures worldwide.5,6
On the basis of the anatomical characteristics of the ankle joint, we propose a four-column classification to guide the treatment of comminuted pilon fractures.
This study was performed to describe use of the staged plate osteosynthesis procedure with the four-column theory to treat type C3.3 pilon fractures and to evaluate the wound healing and clinical and radiologic outcomes of this procedure.
Methods
This retrospective, single-center study was approved by the ethical review committee of the hospital (number 2018ZDSYLL027-P01). Verbal consent was obtained from all patients who participated in the study. Data were collected from patients who had undergone staged treatment with four-column osteosynthesis for AO/OTA type 43-C3.3 pilon fractures from April 2014 to December 2016.
Four-column classification
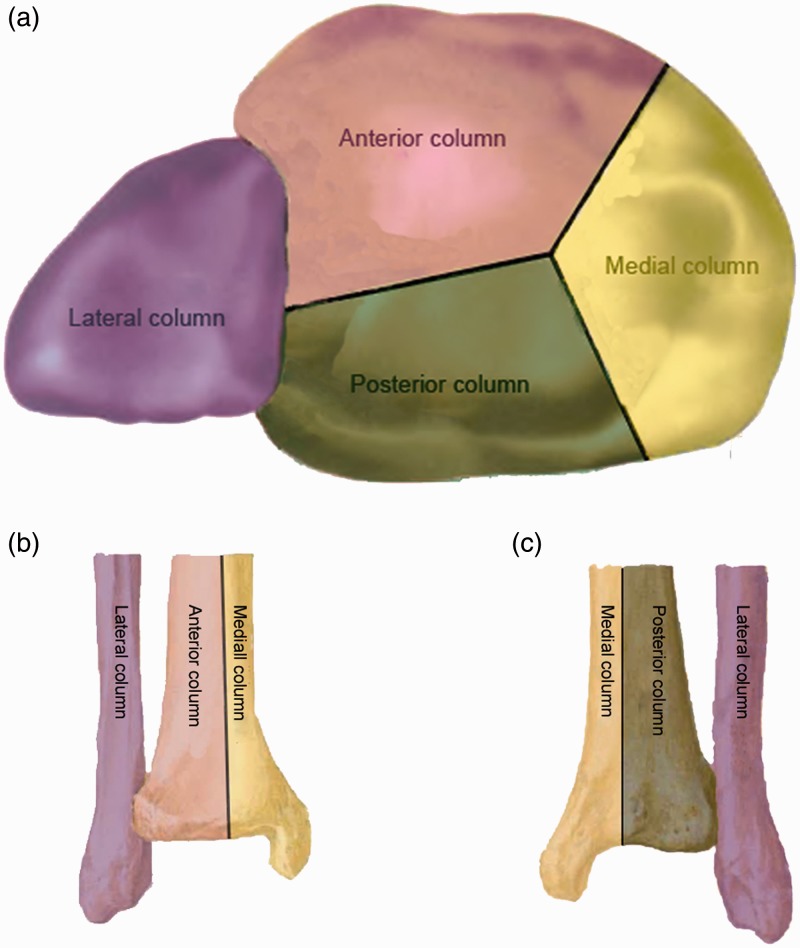
The four-column classification was proposed according to the anatomical characteristics of the tibial and fibular plafond. An intermalleolus line that connects the lateral malleolus and medial malleolus is used to divide the anterior and posterior columns. The medial one-third of the tibial plafond is defined as the medial column, and the distal fibula is regarded as the lateral column (Figure 1). The four-column classification can be summarized as follows:
Figure 1.
Schematic layout of four-column classification of tibial plafond. (a) Axial view of tibial plafond. (b) Anterior view of distal tibia. (c) Posterior view of distal tibia.
Lateral column: the distal fibula
Posterior column: the posterior part of the intermalleolus line with the distal tibial shaft
Anterior column: the anterior part of the intermalleolus line with the distal tibial shaft
Medial column: the medial one-third of the tibial plafond with the distal tibial shaft
Using the Ruedi–Allgower classification system,7 all fractures were classified as grade III. According to the four-column classification scheme, 20 fractures affected the lateral column, 20 fractures affected the posterior column, 20 fractures affected the anterior column, and 21 fractures affected the medial column. Overall, 3 fractures involved 3 columns and 18 fractures involved 4 columns.
Staged management
A staged procedure was carried out according to this new four-column theory.
All open pilon fractures were debrided within 6 hours. The wound was closed in Gustilo type I and II open fractures. Gustilo type III open fractures, which are often accompanied by highly contaminated wounds or extensive soft tissue damage, were treated with continuous vacuum-sealed drainage.
The first stage consisted of calcaneal traction or external fixation within 6 hours. A 3.5-mm Steinmann pin was used to traverse the posteroinferior calcaneus to span the ankle joint in closed fractures with less severe soft tissue injuries (grade C1). The traction pin could be removed before the second stage. Open fractures and closed fractures with severe soft tissue damage (grade C2) were treated by external fixation. Twelve patients were treated with skeletal traction and nine patients were treated with external fixation as the first-stage procedure. The external fixator was carefully positioned according to the soft tissue condition, and the pin site was located away from the subsequent surgical incision. The external fixator was applied as previously described using two or three 5-mm Schanz screws inserted into the medial side of the tibial diaphysis.8 The tuberosity of the calcaneus and the neck of the talus were feasible sites for placement of the distal pins, and the ankle was then distracted with the help of the fixator. Initial reduction was evaluated fluoroscopically, and the external fixator was assembled after confirmation. The aim of this stage is to regain the tibial length and allow healing of the soft tissue (Figure 2).
Figure 2.
External fixator was used in the first stage. (a, a’) Coronal and sagittal computed tomography scan of a left type C3.3 pilon fracture. (b, b’) Three-dimensional reconstruction view. (c, c’) Radiograph 2 days after the first-stage surgery.
To our knowledge, no clear clinical signs exist to determine the optimal time for the next procedure. We usually use the presence of wrinkles or epithelialization of fracture blisters. About 10 to 14 days after the external fixation, the posterolateral approach was chosen midway between the lateral border of the Achilles tendon and the distal fibula. Great attention was paid to identification and protection of the sural nerve when performing dissection in the subcutaneous plane. By retracting the peroneal tendons medially, the fibula fracture was exposed. Dissection was then continued through the area between the peroneal tendons and the flexor hallucis longus tendon to expose the posterior part of the distal tibia. Good exposure was achieved by retracting the flexor hallucis longus tendon medially and the peroneal tendons laterally. The fibula was often fixed first to restore the length of the limb. Very thin, small plates (Synthes, Oberdorf, Switzerland) were used to fix the posterior fragments to the tibial metaphysis or shaft. Screws were only used proximal to the plate to prevent the posterior fragment from moving backward. The articular surface was not restored because we could not obtain satisfactory exposure through this approach. To do this, the posterior column was established. This provided a stable structure for the comminuted fragments to be fixed in the third stage (Figure 3).
Figure 3.
(a, a’) Radiograph of a pilon injury in the left ankle of a 42-year-old man. (b, b’) Three-dimensional reconstruction view. (c, c’) Radiograph 2 days after the second-stage procedure. (d, d’) Radiograph 2 days after the final surgery.
At 10 to 12 days after the second stage, the articular surface was exposed through the anterior approach. The surgical incision using the anterior approach extended from the anterior tibial crest proximally to parallel to the second metatarsal bone distally. Great attention was paid to protection of the superficial peroneal nerve. Deep dissection was continued through the interval between the extensor digitorum longus and the extensor hallucis longus. For direct visualization and accurate reduction of the articular segment, an arthrotomy could be performed close to the fracture line. Good exposure of the comminuted tibial plafond was obtained by retracting the extensor hallucis longus medially and the extensor digitorum longus laterally. The articular fragments could be then restored and temporarily fixed to the posterior and lateral columns with Kirschner pins. Final fixation was accomplished using a low-profile anterolateral plate (Synthes) combined with anterolateral minimally invasive incisions if necessary. Auxiliary plates (Synthes) were used to fix the medial column if necessary (Figure 4). A bone deficit was usually present after reduction of the articular surface, so we performed grafting with artificial bone (Wright Medical Group, Memphis, TN, USA) in all cases to support the articular segment and prevent subsidence.
Figure 4.
(a, a’) Radiograph of a pilon injury in the left ankle of a 45-year-old man. (b, b’) Coronal and sagittal computed tomography scan of the pilon fracture. (c, c’) Three-dimensional reconstruction view. (d, d’) Radiograph 2 years after the final fixation. (e, e’) Coronal and sagittal computed tomography scan 2 years after the final surgery.
After the final operation, a splint or cast was provided to immobilize the ankle joint during the first 2 weeks until the sutures could be removed. Continuous ankle passive and active range-of-motion exercises were initiated from the third postoperative week. A minimum of 8 weeks of a non-weight-bearing status was advised, and partial weight-bearing exercises were allowed when callus formation was observed on X-ray examination. Patients were allowed to perform full weight-bearing ambulation only after complete union of the bone, especially in bilateral cases.
Postoperative evaluation
Radiographic follow-up including anteroposterior and lateral views of the ankle was performed at 1, 2, 3, 6, 12, 24, and 48 months following the operation. A postoperative computed tomography scan was conducted on 11 patients to evaluate the quality of reduction and healing (Figure 5). The Burwell and Charnley9 score, which served as the radiographic criterion for reduction, was used to evaluate the postoperative radiograph. Clinical follow-up was performed using the American Orthopaedic Foot and Ankle Society (AOFAS) evaluation system.10 This system includes clinician-based outcome measures that are used to evaluate patients’ pain, function, and alignment based on clinicians’ observations. The score for a fully normal ankle is 100. In this study, a total score of 90 to 100 was graded as excellent, 75 to 89 as good, 50 to 74 as moderate, and ≤49 as poor. Complications such as superficial infection, deep infection, delayed union, and nonunion were also recorded during follow-up. Superficial infection was defined as abnormal changes in skin color, skin warmth, and drainage over 72 hours, possibly with the addition of pus or increased microbial growth on cultures; however, the infection could be cured by local cleansing and oral antibiotics. Deep infection was defined as severe changes of wounds that required the patient to return to the operating room for debridement and intravenous antibiotics. Delayed union was defined as failure of the fracture to heal according to the radiographic criteria of healing within 3 months of injury, and nonunion was defined as failure of the fracture to heal according to the radiographic criteria of healing within 6 months of injury.11 Statistical analysis was performed using PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, IL, USA). Patients’ age, sex, fracture type, injury type, union time, and follow-up period were recorded, and the standard deviation was calculated. The radiographic outcome was Burwell and Charnley9 score. The clinical outcome data were the AOFAS score and early and late complications.
Figure 5.
(a, a’) Radiograph of a pilon injury in the right ankle of a 45-year-old man. (b, b’) Coronal and sagittal computed tomography scan of the pilon fracture. (c, c’) Three-dimensional reconstruction view. (d, d’) Radiograph 2 years after the final fixation. (e, e’) Coronal and sagittal computed tomography scan 2 years after the final surgery. (f, f’) Clinical outcome 2 years after the final surgery.
Results
Complete clinical and radiographic follow-up data were available for 21 of 23 patients in the analysis. The mean follow-up time was 24.4 (range, 12–43) months. The patients comprised 15 men and 6 women with a mean age of 43.5 years. Of the high-energy injuries, 13 were caused by traffic accidents and 8 by falls from a height. Three were open fractures, one of which was classified as grade I and the remaining two as grade III according to the Gustilo classification system.12 The soft tissue condition in closed fractures was evaluated by the Tscherne system.13 Among the 18 closed fractures, 12 were classified as grade C1 and 6 as grade C2. Five patients had an associated injury: two had cerebral trauma and three had associated fractures, two of which were bilateral pilon fractures (Table 1).
Table 1.
Patient demographics.
| Patients | N = 21 |
|---|---|
| Age, years | 43.5 ± 10.0 |
| Sex | |
| Male | 15 |
| Female | 6 |
| Operative ankle | |
| Right | 12 |
| Left | 9 |
| Fracture type | |
| Open | 3 |
| Closed | 18 |
| Injury type | |
| Traffic accident | 13 |
| Fall from height | 8 |
| Open fractures (Gustilo classification) | |
| I | 2 |
| III | 1 |
| Closed fractures (Tscherne system) | |
| C1 | 12 |
| C2 | 6 |
| Follow-up, months | 24.4 ± 6.8 |
| Associated injury | |
| Cerebral trauma | 2 |
| Associated fracture | 3 |
Data are presented as number of patients or mean ± standard deviation.
Calcaneal traction or external fixation was performed within 6 hours after injury. The average time from the first operation to restoration of the lateral and posterior column was 12 (range, 10–14) days. The mean interval between the second- and the third-stage procedure was 11.4 (range, 10–12) days. The clinical and radiological outcomes demonstrated that all of the patients achieved fracture union, and the average healing time was 3.3 (range, 2.0–5.7) months after the third-stage procedure.
Based on Burwell and Charnley’s radiologic evaluation system,9 the postoperative radiographs showed good and acceptable reduction rates in 85.7% of the patients. Twenty-one cases were available for the AOFAS Ankle-Hindfoot scale assessment, and excellent or good postoperative ankle function was found in 81.0% of the patients (Table 2).
Table 2.
Clinical and radiological outcomes.
| Patients | N = 21 |
|---|---|
| Clinical outcome (American Orthopaedic Foot and Ankle Society) | |
| Excellent (90–100) | 14 (66.7) |
| Good (75–89) | 3 (14.3) |
| Moderate (50–74) | 3 (14.3) |
| Poor (0–49) | 1 (4.8) |
| Quality of reduction (Burwell and Charnley’s radiology evaluation system) | |
| Anatomical | 15 (71.4) |
| Acceptable | 3 (14.3) |
| Poor | 3 (14.3) |
Data are presented as number (%) of patients.
Eight postoperative complications occurred (Table 3). One patient developed superficial infection, and the wound healed after daily dressing changes. One patient developed local skin necrosis, which was treated with vacuum-sealed drainage and subsequent flap transfer. Two patients developed traumatic arthritis. Four patients developed delayed union after the final procedure. No patients developed nonunion or malunion, and none required arthrodesis.
Table 3.
Complications.
| Patients | N = 21 |
|---|---|
| Superficial infection | 1 (4.8) |
| Local skin necrosis | 1 (4.8) |
| Delayed union | 4 (19.0) |
| Traumatic arthritis | 2 (9.5) |
Data are presented as number (%) of patients.
Discussion
All fractures achieved clinical and radiological union. Functional movement was restored in most of the patients as shown by the mean AOFAS score of 81. In fact, the outcome was excellent in 61.7% of the patients, good in 14.3%, moderate in 14.3%, and poor in 4.8%. Good and acceptable reduction rates were observed in 85.7% of the patients.
Various strategies have been advocated to manage severe pilon fractures, but few reports have described the management of type C pilon fractures. Davidovitch et al.14 compared the clinical outcomes between open reduction with internal fixation (ORIF) and external fixation in 2011. The two experimental groups were compared regarding the final range of ankle motion, but postoperative complications with respect to soft tissue injury appeared to be minimized by using a two-stage protocol for ORIF. The mean AOFAS scores in the external fixation and ORIF groups were 77.1 and 72.4, respectively.
Kim et al.15 reported the treatment of AO/OTA type C pilon fractures using the anterolateral minimally invasive plate osteosynthesis technique. They obtained good range of motion of the ankle joint and reasonable function with a fairly low wound complication rate. The mean AOFAS score was 89 at the last follow-up.
No author to date has solely reported the results of AO/OTA type 43-C3.3 pilon fractures alone. Therefore, this is the first report to describe the clinical outcomes and postoperative complications after the application of staged management and a combined approach for this type of fracture.
AO/OTA type 43-C3.3 pilon fractures are the most serious and complicated type of pilon fractures. Axial loading and torsion violence not only contribute to destruction of the tibia plafond, metaphysis, and shaft but also result in severe soft tissue trauma. Compared with low-energy injuries and other fracture types, this kind of fracture has the lowest rate of reduction and highest rates of soft tissue complications, infection, nonunion, and malunion rates. Thus, repair of this fracture with protection of the soft tissue is challenging.
The AO and Ruedi–Allgower systems are usually used to classify tibial pilon fractures. These two systems are all-inclusive and have a good prognostic value, but they cannot provide accurate information on fracture morphology for surgical planning.
The four-column classification was first introduced by Tang et al.,16 who viewed fractures in the lateral part of the distal tibia plafond and the fibula as lateral-column fractures. However, the lateral part of the distal tibia plafond and the fibula were separately restored and fixed in comminuted pilon fractures. It is more reasonable to view the fibula as a single column. Thus, this new four-column theory provides reliable and effective prognoses for surgical treatment of AO/OTA type 43-C3.3 pilon fractures.
A staged procedure protocol was used in this study to protect the soft tissue and stimulate bone healing. The space between the posterolateral and anterior approach ensured at least 7 cm of skin as a bridge to minimize soft tissue and wound complications. Additionally, the posterior and lateral column established in the second stage provided a stable structure for the comminuted fragments to be fixed in the third stage.
Restoration of the articular surface in the second stage is not recommended. Good exposure of the tibia plafond cannot be gained via the posterolateral approach. Moreover, high-energy AO/OTA type 43-C3.3 pilon fractures are often associated with a posterior fragment that is displaced. The posterolateral approach offers direct visualization for reduction of the posterior distal fragment of the tibial pilon. Although the joint surface itself cannot be visualized, this reduction allows the anterior components to be secured to a stable posterior fragment at a later date.17 Four delayed unions occurred in this type of fracture despite stable fixation of the four columns and bone grafting. The reason for these cases of delayed union might be the poor soft tissue condition and indispensable exposure. Although most fractures of this kind were closed, 12 were classified as grade C1 and 6 as grade C2 according to the Tscherne classification system. Furthermore, the fracture line of AO/OTA type 43-C3.3 pilon fractures stretched to the tibia shaft. Exposure of the articular surface, comminuted metaphysis, and diaphysis would necessitate relatively long incisions and dissections. These procedures would interfere with the blood supply to some extent.
In our opinion, the treatment plan should differ from that of lower-energy rotational type pilon fractures, and the interval should be prolonged for high-energy fractures. Only one patient in the present study developed a superficial infection, and another patient developed local skin necrosis that was managed by vacuum-sealed drainage and subsequent flap transfer.
The limitations of our study are as follows. First, this retrospective study had no control group with similar fractures that were treated with alternative methods. Because AO/OTA type 43-C3.3 pilon fractures are rare injuries, it is very difficult to perform a randomized controlled trial to make direct comparisons of any treatment methods. Second, the duration of follow-up was relatively short; conditions such as traumatic arthritis may appear with longer monitoring periods. Finally, bias might have been present in some results when the clinical outcome was only evaluated by the AOFAS evaluation system. We would like to adopt more measurement tools to reduce such bias in a future study.
Conclusion
The herein-described staged procedure protocol combined with the four-column theory is a feasible method for soft tissue protection and fracture reduction. Although the initial outcomes are encouraging, more cases and trials are needed to confirm the efficiency of our proposed treatment.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Michelson J, Moskovitz P, Labropoulos P. The nomenclature for intra-articular vertical impact fractures of the tibial plafond: pilon versus pylon. Foot Ankle Int 2004; 25: 149–150. [DOI] [PubMed] [Google Scholar]
- 2.Mauffrey C, Vasario G, Battiston B, et al. Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg 2011; 77: 432–440. [PubMed] [Google Scholar]
- 3.Barei DP, Nork SE, Mills WJ, et al. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma 2004; 18: 649–657. [DOI] [PubMed] [Google Scholar]
- 4.Bhandari M, Zlowodzki M, Tornetta P, 3rd, et al. Intramedullary nailing following external fixation in femoral and tibial shaft fractures. J Orthop Trauma 2005; 19: 140–144. [DOI] [PubMed] [Google Scholar]
- 5.Barbieri R, Schenk R, Koval K, et al. Hybrid external fixation in the treatment of tibial plafond fractures. Clin Orthop Relat Res 1996; 332: 16–22. [DOI] [PubMed] [Google Scholar]
- 6.Bonar SK, Marsh JL. Unilateral external fixation for severe pilon fractures. Foot Ankle 1993; 14: 57–64. [DOI] [PubMed] [Google Scholar]
- 7.Ruedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res 1979; 138: 105–110. [PubMed] [Google Scholar]
- 8.Okcu G, Aktuglu K. Intra-articular fractures of the tibial plafond. A comparison of the results using articulated and ring external fixators. J Bone Joint Surg Br 2004; 86: 868–875. [DOI] [PubMed] [Google Scholar]
- 9.Burwell HN, Charnley AD. The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement. J Bone Joint Surg Br 1965; 47: 634–660. [PubMed] [Google Scholar]
- 10.Kaikkonen A, Kannus P, Järvinen M. A performance test protocol and scoring scale for the evaluation of ankle injuries. Am J Sports Med 1994; 22: 462–469. [DOI] [PubMed] [Google Scholar]
- 11.Cui X, Chen H, Rui Y, et al. Two-stage open reduction and internal fixation versus limited internal fixation combined with external fixation: a meta-analysis of postoperative complications in patients with severe pilon fractures. J Int Med Res 2018; 46: 2525–2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 1976; 58: 453–458. [PubMed] [Google Scholar]
- 13.Tscherne H, Oestern HJ. A new classification of soft-tissue damage in open and closed fractures (author's transl). Unfallheilkunde 1982; 85: 111–115. [PubMed] [Google Scholar]
- 14.Davidovitch RI, Elkhechen RJ, Romo S, et al. Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA type 43C). Foot Ankle Int 2011; 32: 955–961. [DOI] [PubMed] [Google Scholar]
- 15.Kim GB, Shon OJ, Park CH. Treatment of AO/OTA type C pilon fractures through the anterolateral approach combined with the medial MIPO technique. Foot Ankle Int 2018; 39: 426–432. [DOI] [PubMed] [Google Scholar]
- 16.Tang X, Tang PF, Wang MY, et al. Pilon fractures: a new classification and therapeutic strategies. Chin Med J (Engl) 2012; 125: 2487–2492. [PubMed] [Google Scholar]
- 17.Ketz J, Sanders R. Staged posterior tibial plating for the treatment of Orthopaedic Trauma Association 43C2 and 43C3 tibial pilon fractures. J Orthop Trauma 2012; 26: 341–347. [DOI] [PubMed] [Google Scholar]