Figure 3. Interactions between fungi and the immune system of the skin.
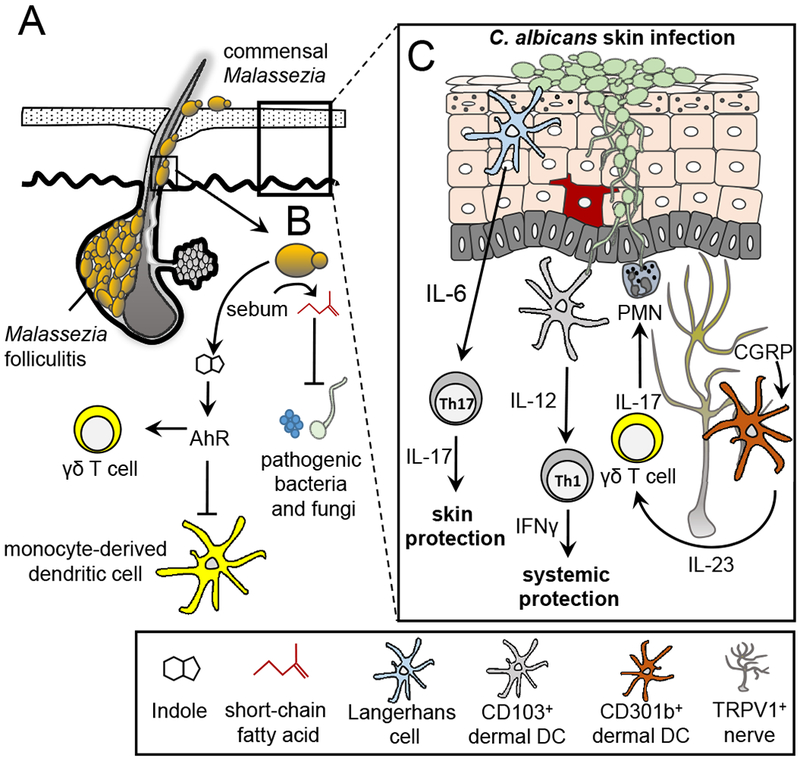
(A) Malassezia species are associated with areas of the skin where sebaceous secretions are present. These fungi utilize long chain fatty acids such as sebum as required carbon sources. Malassezia yeasts have been associated with dermatologic conditions such as Malassezia folliculitis. Normally confined to the infundibulum region of the skin, Malassezia yeasts can invade into the hair follicle causing damage and inflammation. (B) Metabolic byproducts of Malassezia yeasts are important in skin homeostasis. Short chain fatty acids produced from the metabolic breakdown of sebum have dual anti-bacterial and anti-mycotic properties. Potent Ahr indolic ligands produced by Malassezia can inhibit phagocyte responses to TLR stimulation and contribute to cutaneous invariant γδ T cell homeostasis in the skin. (C) Immune responses to Candida albicans skin infection are compartmentalized. In the epidermis, Dectin-1 engagement on LC by C. albicans yeasts stimulates IL-6 production leading to the induction of Th17 CD4+ T cell differentiation and skin immunity. CD103+ dermal DCs detect hyphae C. albicans and produce IL-12 thus priming Th1 CD4+ T cell differentiation and providing systemic protection. Skin TRPV1+ nociceptive nerves are able to detect C. albicans and respond by secreting CGRP which acts on nearby CD301b+ dermal DCs to produce IL-23. γδ T cells respond to IL-23 stimulation by producing IL-17 which activates neutrophils and stimulates anti-microbial peptide production by keratinocytes.
