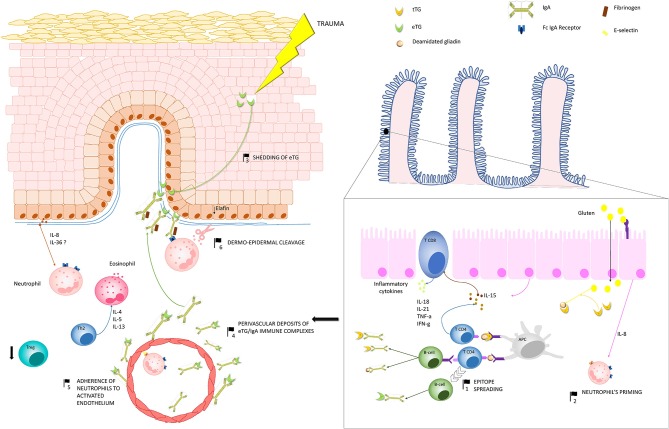
Figure 3.
Pathogenesis of dermatitis herpetiformis (DH): Production of IgA autoantibodies against eTG occurs in the gut, probably as a result of an epitope spreading phenomenon (1), due to the high sequence homology between tissue TG, which is a major autoantigen in coeliac disease, and eTG. Activation of innate immunity in the gut leads to increased release of IL-8, which is thought to be responsible for the initial priming of neutrophils (2). One theory suggests that, in region of trauma, keratinocyte damage leads to shedding of eTG to the dermal-epidermal junction (3), where it binds to anti-eTG IgA. An alternative hypothesis suggests that eTG/IgA complexes exists as circulating immune complexes, which can deposit both at the dermal-epidermal junction and around dermal vessels (4). A complex interplay between inflammatory cytokines and the activation of fibrinogen stimulate neutrophil adherence to the activated endothelium (5) and migration to the dermal papillae. Herein neutrophils, which probably bind to IgA aggregates through the Fc IgA receptor, release proteases, which finally induce the cleavage of the dermal-epidermal junction (6). In parallel, hyper-activation of Th2 cells activate eosinophils, which also co-operate with neutrophils to the cleavage of the dermal-epidermal junction. Down-regulation of Treg cells do also occur, favoring the maintenance of a pro-inflammatory microenvironment in DH skin. Abbreviations in the figure: eTG, epidermal transglutaminase; tTG, tissue transglutaminase; IL, interleukin; Th, T helper cell; Treg, regulatory T cell; APC, antigen presenting cell.