Figure 1.
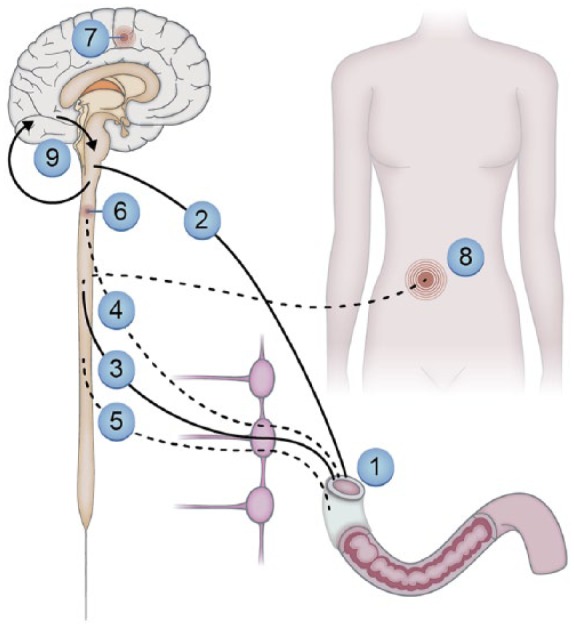
Neural pathways and mechanisms that may lead to pain and other sensory symptoms from the gastrointestinal system in people with diabetic neuropathy.
Neuropathic changes in the enteric nervous system where e.g., motility dysfunction can lead to sensory symptoms: (1) autonomic neuropathy influencing the parasympathetic (2) and (3) sympathetic pathways. Due to cross-talk between the nerve pathways and involvement of inhibitory pathways, this may indirectly modulate sensations from the gut; negative impact on visceral (4) (and somatic (5) if the peritoneum is involved) afferents lead to spontaneous and evoked pain. Structural and functional changes in the spinal cord (6) and brain (7) may lead to spontaneous and evoked pain, amplify afferent barrage and give abnormal referred pain to somatic structures (8). Spino-bulbo-spinal loops (9) that normally control pain intensity often malfunction in people with diabetes.
