Abstract
Objective: To assess the long‐term results of short‐segment pedicle instrumentation for thoracolumbar and lumbar burst fractures.
Methods: From February 1987 to June 1995, 89 patients with thoracolumbar or lumbar burst fracture were treated with short‐segment pedicle instrumentation, and 68 (76.4%) of them were followed up for an average of 8.0 years (range, 5–13 years). Radiographs were taken pre‐ and post‐ operatively, before implant removal and at final follow‐up. Computerized tomography (CT) scans of the fractured vertebrae were done on 18 patients, with their consent, at final follow‐up.
Results: At final follow‐up, neurological status had improved at least one grade in the Frankel Grading system in 90.8% patients who had presented incomplete paralysis preoperatively, and low back pain was evaluated as Denis' P1 in 60.3%, P2 in 35.3% and P3 in 4.4% of patients. An average of 2.5 mm (range, 0–6.5 mm) of implant deformation was recorded before implant removal, and implant failure was noted in 11 (16.2%) patients. At final follow‐up, loss of correction of the anterior vertebral body height and Cobb angle averaged 1.9% and 12.1°, leaving residual correction rates of 30.5% and 5.8°, respectively. The loss of correction occurred mainly at adjacent disc spaces, and collapse of the vertebral body was more severe at its center. CT scan revealed an obvious gap, which communicated with the adjacent disc space, in the vertebral body of 16 of the 18 patients scanned. Local kyphosis of more than 20° existed in five patients and three of them had low back pain.
Conclusion: Short‐segment pedicle instrumentation provides satisfactory reduction for thoracolumbar and lumbar burst fractures. The relatively high incidence of implant failure and the loss of correction may be caused by various factors, and more adequate fusion is recommended.
Keywords: Lumbar, Spinal fractures, Treatment outcome
Introduction
Thoracolumbar and lumbar burst fractures are frequent injuries in clinical practice. Since short‐segment pedicle instrumentation was introduced for the treatment of thoracic and lumbar fractures, satisfactory results have frequently been reported, and this procedure has become a commonly chosen option for burst fractures 1 , 2 , 3 . It provides powerful reduction of vertebral body height and local lordosis, as well as indirect reduction of the intracanal fragment, while requiring fixation and fusion of the fewest segments. Besides, pedicle instruments are installed through a posterior approach, which is familiar to most orthopedic surgeons. However, a relative high incidence of implant failure and correction loss has been noted in previous follow‐up studies 4 , 5 .
During this procedure, posterolateral grafting after instrumented reduction and fixation has generally been deemed indispensable, and some authors also advocate transpedicular intracorporeal grafting to prevent implant failure 5 , 6 , 7 . However, as comparable results have been reported after short‐segment fixation with and without fusion, the latter has obvious advantages in elimination of donor site complications, and reduction of intraoperative blood loss and operation time 8 , 9 .
Accordingly, in our practice posterolateral bone grafting has not been included as part of this procedure for some time; therefore neither autologous iliac bone nor another substitute has been used for grafting. In patients undergoing laminectomy, only limited bone from the laminectomy was grafted to the lateral side of the articular process, and no grafting was attempted in patients without decompression. A retrospective 5 to 13 years follow‐up was analyzed to evaluate the long‐term results of this procedure.
Materials and methods
Patients
From February 1987 to June 1995, 136 patients were treated with short‐segment pedicle instrumentation for thoracic or lumbar fractures in our department. Eighty‐nine patients with a burst fracture, (according to the Denis classification 10 ), of a single thoracolumbar or lumbar vertebra were included in this retrospective follow‐up study. Patients with severe intrusion into the spinal canal (more than 40% at T12 or above, 50% at L1 and 60% at L2 or below) and neurological compromise, and those with more than 60% vertebral collapse, were treated with anterior surgery and excluded from this study. At final follow‐up, two patients had died of reasons unrelated to their surgery and 19 patients had dropped out, leaving 68 patients available for evaluation (76.4% follow‐up rate). This included 52 males and 16 females with an average age of 39.1 years at admission (range, 21–59 years). The fractured levels were T11 (n= 3), T12 (n= 14), L1 (n= 26), L2 (n= 15), L3 (n= 9) and L4 (n= 1), and the fracture types were Denis A (n= 26), B (n= 39) and C (n= 3). Preoperative neurological compromise was present in 36 patients with Frankel A (n= 5), B (n= 6), C (n= 8) and D (n= 17). Fifteen of them complained of dysuria, and were given intravenous corticosteroid. Preoperative radiographs and computerized tomography (CT) scans were taken in all patients.
Surgical treatment
All patients were operated on under general anesthesia within 10 days of injury. Standard short‐segment transpedicular fixation with one level above and one level below the fractured vertebra was performed through a routine posterior midline approach. Two types of short‐segment pedicle implants were used for reduction and fixation, namely posterior short‐segment fixation (PSSF) in 27 and screw‐rod angle pedicle fixation (APF) in 41 patients 11 , 12 . Both systems were modified from the Dick type of pedicle fixation, and were made in China with stainless steel 316. The special design of the angle pedicle screw provided powerful restoration of normal lordosis.
Laminectomy was performed in 36 patients with neurological compromise. The lateral part of the facet was preserved if possible, and laceration of the dural sac was sutured if present. Two rods were installed to connect the pedicle screws, then an instrumented reduction force was applied for lordosis and distraction, and the vertebral body height and segmental lordosis were restored and checked with intraoperative fluoroscopy. No cross‐link was used, as sufficient rigidity was provided by the instrumentation as proved by biomechanical testing. In 36 patients undergoing laminectomy, the bone removed during laminectomy was placed on the lateral side of the articular process, while no grafting was attempted in the other 32 patients. Neither autologous iliac graft nor other graft material was used.
A lumbar corset was recommended during out of bed activities for three months. Revision surgery was proposed to remove the implants within one year of operation.
Follow‐up evaluation
Sixty‐eight patients were followed for more than 5 years (range, 5–13 years; average, 8 years). Clinical evaluation was undertaken in the Outpatients Department. Anterior‐posterior (AP) and lateral radiographs centered on the fractured vertebra were taken before and after surgery, before implant removal and at final follow‐up. At final follow‐up, voluntary CT scan examination was advised, and 18 patients agreed to it.
On lateral plain radiograph, measurements made included the anterior, posterior and middle height of the fractured vertebral body, the anterior and posterior height of the disc spaces adjacent to the fractured vertebra, the sagittal angulation of the fractured vertebra and adjacent disc spaces, and the Cobb angle (angle between the superior endplate one level above the fracture and the inferior endplate one level below the fracture, lordosis was deemed as positive, kyphosis as negative). The height of the adjacent vertebra below the fracture was measured as a reference. Reduction was calculated as the difference between pre‐ and post‐ operation in height and lordosis. Correction loss was calculated as the difference in height and lordosis between immediately postoperative and just prior to implant removal, and the difference between immediately postoperative and at final follow‐up, respectively. The shortest distance between the upper and lower screw tips was measured on lateral radiograph just prior to implant removal and immediately postoperatively, and any shortening of this distance was deemed as deformation of the implant.
The discs adjacent to the fractured vertebra were assessed and compared between preoperative and at final follow‐up according to the Mimura method with AP and lateral radiographs (Table 1) 13 .
Table 1.
Radiographic grading of discs according to Mimura et al 13
| Disc height (% of adjacent discs) | Osteophyte formation (sum of points on 8 edges: <3 mm 1 pt., >3 mm 2 pts. | Endplate sclerosis |
|---|---|---|
| 0 = normal | 0 = 0 point | 0 = none |
| 1 = mild (>75%) | 1 = 1–4 points | 1 = either endplate |
| 2 = moderate (>50%) | 2 = 5–8 points | 2 = both endplates |
| 3 = severe (>25%) | 3 = 9–12 points | |
| 4 = very severe (<25%) | 4 = 13–16 points |
1, 0 to 1.5 points; 2, 2 to 3.5 points; 3, 4 to 6 points; 4, score of 6.5 or greater.
Results
Long‐term clinical results
Of the 31 patients with preoperative incomplete paralysis, 28 patients (90.3%) experienced improvement of at least 1 Frankel grade, while one patient with Frankel B and two patients with Frankel D remained at the same grade. All five patients with Frankel A remained at the same grade. Of the 15 patients with preoperative dysuria, 7 patients recovered sphincter function and 3 of them experienced partial improvement, while the other 5 patients with Frankel A experienced no obvious recovery.
Back pain was assessed according to the Denis evaluation scale (Table 2). 14 Forty‐one patients (60.3%) were rated as P1, 24 patients (35.3%) as P2 and 3 patients (4.4%) as P3. Twenty‐nine patients (42.6%) returned to their previous occupation or were engaged in heavy physical work, 32 patients (47.1%) changed their work, and seven patients (10.3%) could not work but had adequate function for daily activities.
Table 2.
Evaluation scale of back pain according to Denis 10
| Grade | Criteria |
|---|---|
| P1 | No pain |
| P2 | Occasional, minimal pain; no need for medication |
| P3 | Moderate pain, occasional medication, no interruption of work or activities of daily living |
| P4 | Moderate to severe pain, occasional absence from work, significant in activities of daily living |
| P5 | Constant severe pain, chronic medication |
Implant failure
Screw breakage occurred in seven patients. For the other 61 patients, the shortest distance between the upper and lower screw tips shortened by 2.5 mm on average (range, 0–6.5 mm) between immediately postoperative and just prior to implant removal.
Sixty patients underwent revision surgery to remove their implants at an average of 13.2 months (range, 8–24 months) after operation. Among them, the screws had loosened in one patient, bent in two (Fig. 1), and broken in five patients (Fig. 2). Screw breakage occurred at one lower screw in two patients, two lower screws in one patient, one upper and one lower screw in one patient, and one upper and two lower screws in one patient.
Figure 1.
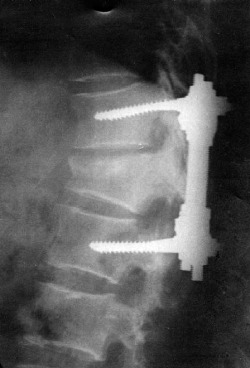
A 50‐year‐old male who had a T12 burst fracture treated with PSSF, 6 months postoperative radiograph showing bent pedicle screws.
Figure 2.
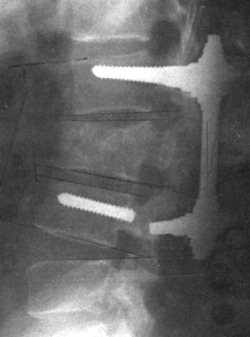
A 45‐year‐old male who had a L2 burst fracture treated with APF, note the broken lower pedicle screw.
Eight patients were unwilling to undergo revision surgery. Among them, the nut loosened in one patient at 8 years (Fig. 3), a screw broke in two patients at 5 and 6 years (Fig. 4) and local foreign body reaction occurred in two patients at 6 and 8 years, respectively. All these five patients underwent revision surgery with implant removal and had good results. The other three patients refused revision surgery: one had mild back pain at 8 years, and two had no discomfort 9 and 11 years after operation.
Figure 3.

A 48‐year‐old male who had a L1 burst fracture treated with PSSF. Radiograph at 8 years after surgery showing loose nuts.
Figure 4.
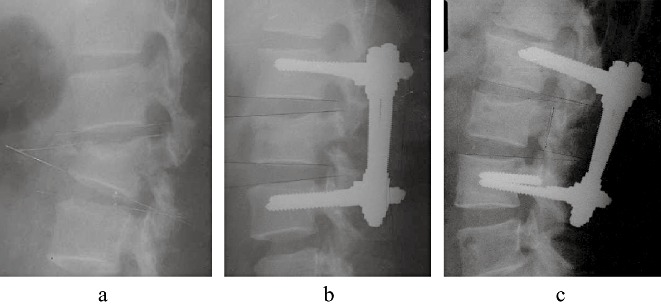
A 48‐year‐old male who had a L2 burst fracture treated with APF. The implant had not been removed at 6 years follow‐up, he had low back pain and a broken screw, as well as a degenerated disc adjacent to the fixation level. The implant was removed by revision surgery with good response. (a) Preoperative radiograph; (b) Postoperative radiograph; (c) Radiograph at 6 years after surgery, note the broken lower pedicle screw, and degeneration of the upper disc adjacent to the fixation level.
Of the 27 patients with PSSF fixation, implant failure included a loose nut, a loose screw and screw breakage, each in one patient, and a bent screw in two patients. Of the 41 patients with APF fixation, implant failure included screw breakage in six patients (14.6%). Thus a total of 11 patients (16.2%) had implant failure; including a loose nut and a loose screw, each in one patient, a bent screw in two patients, and screw breakages in seven patients. The screw breakages occurred at the entry site; six broken screws remained in four patients because of difficulties during removal. No adverse response was noted among these patients.
Reduction and correction loss
The height of the fractured vertebral body had clearly improved by final follow‐up compared to preoperatively: the anterior vertebral body height averaged 16.4 mm preoperatively, and 25.8 mm at final follow‐up, with an average reduction of 9.4 mm (30.5% relative to the referent vertebra below it). Loss of correction of the anterior and middle vertebral body heights at final follow‐up averaged 0.6 and 1.8 mm (1.9% and 6.0% relative to the referent vertebra below it), respectively (Table 3).
Table 3.
Reduction and correction loss in the fractured vertebral body and adjacent discs (mean ± SD)
| Index | Preoperative | Reduction | Loss before implant removal | Loss at final follow‐up | Final follow‐up |
|---|---|---|---|---|---|
| Anterior up disc height (mm) | 6.0 ± 2.4 | 3.1 ± 2.5 | 4.3 ± 4.3 | 6.1 ± 3.7 | 2.9 ± 2.1 |
| Anterior vertebra height (mm) | 16.4 ± 4.7 | 9.9 ± 6.1 | 0.4 ± 1.5 | 0.6 ± 1.1 | 25.8 ± 5.5 |
| Anterior below disc height (mm) | 9.8 ± 3.5 | 1.5 ± 1.7 | 3.2 ± 2.7 | 5.1 ± 3.9 | 6.2 ± 4.1 |
| Middle vertebra height (mm) | 19.1 ± 5.5 | 6.2 ± 5.7 | 1.7 ± 3.1 | 1.8 ± 3.1 | 23.1 ± 5.6 |
| Posterior up disc height (mm) | 3.2 ± 1.9 | 0.7 ± 2.2 | 1.4 ± 1.8 | 1.9 ± 2.1 | 1.9 ± 1.7 |
| Posterior vertebra height (mm) | 34.1 ± 2.4 | 0.7 ± 2.7 | −0.1 ± 1.1 | −0.4 ± 1.1 | 35.1 ± 1.7 |
| Posterior below disc height (mm) | 4.4 ± 2.6 | 0.9 ± 1.8 | 1.2 ± 1.5 | 1.2 ± 2.3 | 4.1 ± 2.0 |
| Lordosis in up disc (degree) | 3.7 ± 3.4 | 3.4 ± 4.4 | 4.4 ± 4.9 | 6.1 ± 3.4 | 1.0 ± 2.7 |
| Lordosis in vertebra (degree) | −22.3 ± 10.2 | 13.3 ± 9.2 | 0.4 ± 3.8 | 1.6 ± 3.8 | −10.6 ± 6.23 |
| Lordosis in lower disc (degree) | 6.9 ± 4.1 | 1.2 ± 4.7 | 2.7 ± 3.9 | 4.4 ± 3.8 | 3.7 ± 3.9 |
The Cobb angle averaged −11.7° preoperatively; 6.2° postoperatively with an average reduction of 17.9°, and −5.9° at final follow‐up with an average correction loss of 12.0°, leaving a final average reduction of 5.8°.
Reduction and correction losses were assessed at the fractured vertebral body and adjacent disc spaces (Table 3). Reduction during operation occurred mainly at the fractured vertebral body. However, correction loss during follow‐up occurred mainly at the adjacent disc spaces, especially the superior adjacent disc. Indeed, correction loss occurred prior to implant removal, accompanied by implant deformation.
Correlation between correction loss, reduction and collapse
Correction losses in anterior and middle vertebral body height at final follow‐up were positively correlated to the extent of preoperative vertebral body collapse (r= 0.28, 0.28, P < 0.05, respectively), and reduction (r= 0.32, 0.29, P < 0.05, respectively). Collapses of the anterior and middle vertebral body at final follow‐up were positively correlated to the extent of preoperative collapse (r= 0.38, 0.34, P < 0.05, respectively), and negatively correlated to reduction (r=−0.64, −0.33, P < 0.05, respectively).
Deformation of the fractured vertebral body
At final follow‐up, collapse and correction loss of the vertebral body were more severe in the middle part (Table 3). On radiograph, obvious concavity of the superior part of the vertebral body was found in 52 (76.5%) patients, and the deformity known as ‘codfish vertebra’ was found in 21 (30.9%) of them. In five patients, the upper adjacent vertebral body had settled into the concavity of the fractured vertebral body (Fig. 5).
Figure 5.

A 51‐year‐old female who had a L2 burst fracture treated with APF. Radiograph at 6 months after implant removal showing a ‘codfish vertebra’ type of deformity of the superior part of the vertebral body.
Among the 18 patients examined with CT scans, an obvious gap in the vertebral body was found in 16 (88.9%) patients, all such gaps communicated with the upper adjacent disc space (Fig. 6).
Figure 6.

A 31‐year‐old male who had a L1 burst fracture fixed with APF. CT scan at 5 years after implant removal showing an obvious gap, which communicates with the upper disc space, in the vertebral body.
Changes in adjacent discs
The disc spaces above and below the fractured vertebra had narrowed significantly by final follow‐up. Spontaneous fusion occurred at the upper disc space in 27 patients and at the lower disc space in 14 (Fig. 7). According to the Minura classification, the upper and lower adjacent discs had ‘degenerated’ significantly by final follow‐up compared to preoperatively (χ2 test, upper adjacent discs: χ2= 67.10, ν= 3, P < 0.01; lower adjacent discs: χ2= 119.36, ν= 3, P < 0.01, respectively, Table 4).
Figure 7.

A 59‐year‐old male who had a L2 burst fracture treated with PSSF. The implant had not been removed at 11 years follow‐up. Despite severe degeneration of adjacent discs seen on radiograph, he had no discomfort with good function.
Table 4.
Comparison of degeneration of discs adjacent to vertebral body between preoperatively and at final follow‐up
| Mimura Grade | Upper adjacent disc | Lower adjacent disc | ||
|---|---|---|---|---|
| Preoperative (68 cases) | Final follow‐up (62 cases) | Preoperative (68 cases) | Final follow‐up (62 cases) | |
| 1 | 28 | 45 | ||
| 2 | 40 | 23 | 3 | |
| 3 | 16 | 37 | ||
| 4 | 46 | 22 | ||
χ2 test, upper adjacent discs: χ2= 67.10, ν= 2, P < 0.01; lower adjacent discs: χ2= 119.36, ν= 2, P < 0.01.
Degeneration of the disc adjacent to the instrumented segments was found in one patient, in whom the implant was not removed until 6 years after surgery (Fig. 4).
Correlation between long‐term clinical results and radiological findings
Local kyphosis of more than 20° existed in five patients: one patient underwent revision surgery with implant removal 5 months after surgery because of a loose screw, and a 30° kyphosis was recorded (Fig. 8). Four patients with PSSF had insufficient reduction; 21°, 22°, 25° and 27° kyphoses were recorded respectively. Four of the five patients had back pain (two with Denis P3, and two with P2). Patients with more than 20° local kyphosis were found to have more back pain (χ2 test, χ2= 16.98, ν= 2, P < 0.01, Table 5); however, no significant correlation was found between ‘degeneration’ of adjacent discs and clinical results (P > 0.05).
Figure 8.
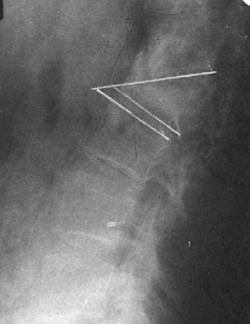
A 47‐year‐old male who had a L2 burst fracture treated with PSSF. The implant had to be removed 6 months after surgery because of loose screws. Radiograph showing that the upper vertebral body has sunk into the fractured body, and a local kyphosis of 30° has occurred. He had low back pain but refused revision operation.
Table 5.
Comparison of back pain between patients with and without more than 20° kyphosis
| Patients | Denis P1 | Denis P2 | Denis P3 |
|---|---|---|---|
| With >20° kyphosis | 40 | 22 | 1 |
| Without >20° kyphosis | 1 | 2 | 2 |
| Total | 41 | 24 | 3 |
χ2 test, χ2= 16.98, ν= 2, P < 0.01.
Discussion
Clinical results
Short‐segment pedicle instrumentations provide successful reduction for thoracolumbar and lumbar burst fractures, with restoration of vertebral body height and physical lordosis. Despite correction loss, at final follow‐up vertebral body height and spinal alignment were still significantly improved compared to pre‐operatively. Partial indirect reduction of intracanal fragments can be completed with ligamentotaxis. Posterior surgery is also convenient for the treatment of posterior element injuries, such as fractured lamina or facet protruding into the canal and lancination of the dural theca. However, neurological recovery was poor in patients with complete paraplegia or conus medullaris syndrome. Sphincter dysfunction remained in 8 of the 15 patients with preoperative dysuria, including all 5 patients with complete paralysis. Residual back pain was reported in 27 (39.7%) patients, and local kyphosis of more than 20° was associated with back pain.
Injured vertebrae
During burst fracture, the nucleus pulposus and fractured endplates are intruded into the fractured vertebral body, resulting in collapse of the cancellous framework of the vertebral body. 1 , 10 During posterior instrumented reduction, the annulus fibrosus of the collapsed disc is distracted, and then the fractured vertebral body wall reduced by the annulus fibrosus attached at the periphery of the endplate, but the fragmented nucleus, endplates and collapsed cancellous framework are not sufficiently reduced, due to the annulus fibrosus not being sufficiently attached at the center of the endplate. Some authors have described ‘eggshell’ deformity after posterior ligamentotaxis reduction, the gap in the vertebral body having gradually filled with fibrous tissue instead of bone fusion in the long‐term 1 .
In our long‐term follow‐up, correction loss and collapse of the vertebral body were most severe in the middle part, and obvious concavity at the superior part of the body was found in 52 (76.5%) patients, including the deformity of ‘codfish vertebra’ in 21 (30.9%) patients. An obvious gap in the vertebral body was found in 88.9% patients examined with CT scans, and this gap communicated with the upper adjacent disc space in all patients. Due to collapse of the central part of fractured vertebral body after reduction, we speculate that the resultant deformity may be more like a ‘cup’ than an ‘eggshell’, with the fragmented nucleus and endplates remaining in the bottom of the ‘cup’ (Fig. 9).
Figure 9.
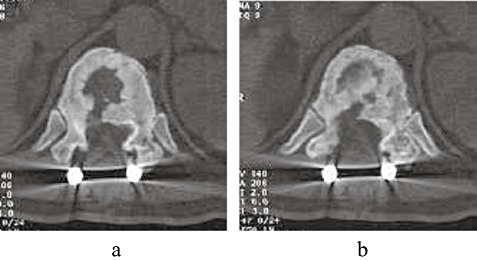
A 36‐year‐old male who had a T12 burst fracture treated with APF. Postoperative CT scans showing collapse of the central part of the fractured vertebral body after reduction, with the fragmented nucleus and endplates remaining in the bottom of a ‘cup’ instead of an ‘eggshell’. (a) Presumed deformity of ‘cup’; (b) Fragments of endplate and nucleus in the ‘cup’.
The more severe the preoperative collapse of the fractured vertebral body is, the more obvious the correction loss that is found on follow‐up. Although correction loss was positively correlated to reduction, collapse at final follow‐up was negatively correlated to reduction; that is, after sufficient reduction, relatively minor collapse occurs.
Discs adjacent to fractured vertebral body
When the nucleus pulposus and fractured endplate intrude into a burst vertebral body, the adjacent discs lose their integrity, and this can not be sufficiently recovered with posterior instrumented reduction. Adjacent discs are usually fully distracted through ligamentotaxis, but remain incapable of load conduction. Without load sharing at the anterior column, the pedicle screw implants are exposed to a high cantilever bending load. After full distraction, the spinal column can not accommodate previously tolerated loads, so deformation or failure of pedicle instruments may occur with long‐term cycling of axial loads. Indeed, the disc spaces narrow even before implant removal, accompanied by implant deformation, and narrowed even more obviously after implant removal. At long‐term follow‐up, in our study the majority of correction loss resulted from narrowing or collapse of adjacent disc spaces, which is consistent with previous reports 15 .
Due to fracture and collapse of the endplate and cancellous framework of the vertebral body, the nucleus pulposus is redistributed and partially settles in the collapsed vertebral body. Correction loss and collapse continue until the load can be transferred from the instruments to the spinal column. Since the superior endplate is often more severely injured during burst fracture, the upper adjacent disc was found to be more obviously narrowed at follow‐up in our study. However, no correlation was found between narrowing or ‘degeneration’ of adjacent discs and back pain, this may be explained by the relative stability of these disc spaces. Degeneration of the disc adjacent to the instrumented segments was found in only one patient whose implant was not removed at the optimal time.
Causes of implant failure and correction loss
Despite satisfactory restoration of vertebral body height and spinal alignment as seen on postoperative radiograph, the integrity of the burst vertebral body and its adjacent discs do not recover fully. Nor does their load sharing ability, thus the pedicle screws must bear most of the axial load in a cantilever bending mode. As high as 9%–54% incidence of implant failure and 3°–12 ° of correction loss is reported in the literature concerning pedicle instrumentation for thoracic and lumbar fractures 16 . At our long‐term follow‐up, implant failure had occurred in 16.2% of patients with an average correction loss of 12°. Multiple factors may contribute to this high incidence.
Firstly, standard posterolateral grafting was not performed in our patients, 36 patients received limited grafting with decompressed bone at the lateral side of the facet, and the other 32 patients did not receive any grafting. Credible posterolateral fusion was not found in our patients during follow‐up, resulting in long‐term cycling of axial loads on the pedicle instruments. With deformation or failure of the implant, correction loss was inevitable.
Secondly, the pedicle instruments used in our patients were fabricated with stainless steel, which has more rigidity and less ductility than titanium alloy, thus they had a limited capacity to adjust to deformation. Revision surgery was proposed to remove these steel implants within one year after surgery; however, some patients were unwilling to undergo revision surgery. This may have increased the incidence of implant failure and other adverse responses, such as late foreign body reactions in two of our patients.
Thirdly, a postoperative brace was not used strictly by our patients. Most of them used a soft short lumbar corset, which is inferior to a thoracolumbar brace for protection.
Fourthly, as the pedicle screws of short‐segment instrumentation are exposed to large cantilever bending loads, supplemental offset laminar hooks and three or four segment fixation have been proposed to distribute the corrective forces more widely, but these were not attempted in our patients 17 , 18 , 19 .
Another deficiency may relate to the extensive controversy surrounding the choice of anterior or posterior surgery for thoracolumbar and lumbar burst fractures 19 , 20 , 21 . Load classification has been proposed to evaluate the integrity and load sharing ability of the fractured vertebral body, and anterior surgery has been suggested for those with more comminuted vertebrae and limited load‐sharing ability 16 . This classification was not adopted in our patients.
Although transpedicular intracorporeal grafting has not been sufficiently proved to be effective in the prevention of implant failure and correction loss, balloon vertebroplasty has been used recently, in combination with short‐segment pedicle instrumentation, to restore the collapsed central endplate, as well as the anterior column load‐sharing ability. 22 , 23 However, insufficiency of the injured adjacent disc constitutes the main source of correction loss and implant failure according to follow‐up findings. Although balloon vertebroplasty may be helpful in restoring disc configuration in some cases, its effectiveness remains to be proven.
Despite deficiencies in this retrospective study, the long‐term findings enable us to have some insight into the long‐term results of pedicle instrumentation for thoracolumbar and lumbar burst fractures. The relatively high incidence of implant failure and loss of correction may be caused by various factors, and more adequate fusion is recommended.
Disclosure
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work. No benefits of any type have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1. Weidenbaux M, Farcy JPC. Surgical management of thoracic and lumbar burst fractures In: Bridwell KH, Dewald RL, eds. The Text Book of Spinal Surgery, 2nd edn. Philadelphia: Lippincott Raven, 1997; 1839–1880. [Google Scholar]
- 2. Dickman CA, Yahiro MA, Lu HT, et al. Surgical treatment alternatives for fixation of unstable fractures of the thoracic and lumbar spine. A meta‐analysis. Spine, 1994, 19 (20 Suppl.): 2266–2273. [DOI] [PubMed] [Google Scholar]
- 3. Katonis PG, Kontakis GM, Loupasis GA, et al. Treatment of unstable thoracolumbar and lumbar spine injuries using Cotrel‐Dubousset instrumentation. Spine, 1999, 24: 2352–2357. [DOI] [PubMed] [Google Scholar]
- 4. Mclain RF, Sparling E, Benson DR. Early failure of short‐segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am, 1993, 75: 162–167. [DOI] [PubMed] [Google Scholar]
- 5. Knop C, Fabian HF, Bastian L, et al. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine, 2001, 26: 88–99. [DOI] [PubMed] [Google Scholar]
- 6. Alanay A, Acaroglu E, Yazici M, et al. Short‐segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure? Spine, 2001, 26: 213–217. [DOI] [PubMed] [Google Scholar]
- 7. Leferink VJ, Zimmerman KW, Veldhuis EF, et al. Thoracolumbar spinal fractures: radiological results of transpedicular fixation combined with transpedicular cancellous bone graft and posterior fusion in 183 patients. Eur Spine J, 2001, 10: 517–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sanderson PL, Fraser RD, Hall DJ, et al. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J, 1999, 8: 495–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang ST, Ma HL, Liu CL, et al. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine, 2006, 31: 2646–2652. [DOI] [PubMed] [Google Scholar]
- 10. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine, 1983, 8: 817–831. [DOI] [PubMed] [Google Scholar]
- 11. Tang TS, Qiu Y, Zhu GL, et al. The treatment of thoracolumbar and lumbar fractures with posterior short‐segment fixation (PSSF) (Chin). Zhonghua Wai Ke Za Zhi, 1989, 27: 272–275. [PubMed] [Google Scholar]
- 12. Yang HL, Tang TS, Zhu GL, et al. The screw‐rod angle pedicle fixation (APF) for the treatment of thoracic and lumbar fractures (Chin). Zhonghua Gu Ke Za Zhi, 1995, 15: 570–572. [Google Scholar]
- 13. Mimura M, Panjabi M, Oxland TR, et al. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine, 1994, 19: 1371–1380. [DOI] [PubMed] [Google Scholar]
- 14. Denis F, Armstrong GW, Searls K, et al. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res, 1984, 189: 142–149. [PubMed] [Google Scholar]
- 15. Muller U, Berlemann U, Sledge J, et al. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusion. Eur Spine J, 1999, 8: 284–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Parker JW, Lane JR, Karaikovic EE, et al. Successful short‐segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2‐year series. Spine, 2000, 25: 1157–1170. [DOI] [PubMed] [Google Scholar]
- 17. McLain RF. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine, 2006, 31 (11 Suppl.): 70–79. [DOI] [PubMed] [Google Scholar]
- 18. Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: short‐segment pedicle fixation versus long‐segment instrumentation. J Spinal Disord Tech, 2005, 18: 485–488. [DOI] [PubMed] [Google Scholar]
- 19. Sasso RC, Renkens K, Hanson D, et al. Unstable thoracolumbar burst fractures: anterior‐only versus short‐segment posterior fixation. J Spinal Disord Tech, 2006, 19: 242–248. [DOI] [PubMed] [Google Scholar]
- 20. Been HD, Bouma GJ. Comparison of two types of surgery for thoraco‐lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir (Wien), 1999, 141: 349–357. [DOI] [PubMed] [Google Scholar]
- 21. Verlaan JJ, Diekerhof CH, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine, 2004, 29: 803–814. [DOI] [PubMed] [Google Scholar]
- 22. Verlaan JJ, Van De Kraats EB, Oner FC, et al. The reduction of endplate fractures during balloon vertebroplasty: a detailed radiological analysis of the treatment of burst fractures using pedicle screws, balloon vertebroplasty, and calcium phosphate cement. Spine, 2005, 30: 1840–1845. [DOI] [PubMed] [Google Scholar]
- 23. Oner FC, Verlaan JJ, Verbout AJ, et al. Cement augmentation techniques in traumatic thoracolumbar spine fractures. Spine, 2006, 31 (11 Suppl.): 89–95. [DOI] [PubMed] [Google Scholar]


