Abstract
This paper presents a highly challenging technique involving posterior double vertebral column resections (VCRs) and satellite rods placement. This was a young adult case with severe angular thoracolumbar kyphosis of 101 degrees, secondary to anterior segmentation failure from T11 to L1. There were hemivertebrae at T11 and T12, and a wedged vertebra at L1. He received double VCRs at T12 and T11 and instrumented fusion from T6 to L4 via a posterior only approach. Autologous grafts and a cage were placed between the bony surfaces of the osteotomy gap. Once closure of osteotomy was achieved, bilateral permanent CoCr rods were placed with addition of satellite rods. Postoperative X‐ray demonstrated marked correction of kyphosis. On the 10th days after surgery, the patient was able to walk without assistance. In conclusion, double VCRs are effective to correct severe angular kyphosis, and addition of satellite rods may be imperative to enhance instrumentation strength and thus prevent correction loss.
Keywords: Vertebral column resection, Satellite rod, congenital kyphosis, Three‐column osteotomy
Introduction
Posterior vertebral column resection (VCR) is the optimal procedure for correction of thoracolumbar angular kyphosis because it ensures maximal excision of deformity1, 2, 3, 4, 5, 6, 7. However, because VCR interrupts the original continuity of the spine column, it renders the whole spine at risk of high instability; thus, neurological complications can and do occur8, 9, 10, 11, 12, 13. Although the cephalad and caudal segments are connected via bilateral rods after reduction at the osteotomy gap, there is still a risk of pseudarthrosis. Several studies have reported a relatively high rate of rod breakage because of pseudarthrosis during postoperative follow‐up14, 15, 16, 17, 18. Pseudarthrosis may result from an anterior support defect at the osteotomy gap because of incomplete bone‐on‐bone closing, incomplete removal of the disc, insufficient support by the anterior column, or dislocation between the osteotomized ends before establishment of solid fusion. Clinically, revision surgery involving addition of multiple rods across the site of a pseudarthrosis and connection of those rods to the original rods has been shown to more strongly stabilize the instrumentation system, and thus to facilitate subsequent solid fusion.
Hence, enhancement of instrumentation strength is a strong priority when performing primary surgery entailing VCR to correct thoracolumbar kyphosis. A satellite rod technique may be an optimal means of achieving this19, 20. Such a technique has the following advantages. First, the satellite rods share the stress at the osteotomy site. Secondly, they more strongly stabilize the whole instrumentation system. Thirdly, these adjunctive implants help to better maintain balance in the coronal and sagittal planes. And lastly, from the perspective of efficiency, it is relatively easy and not time‐consuming to add satellite rods medially or laterally to the main corrective rods. Hence, in our clinical practice we have routinely employed this technique around VCR sites, our aim being to achieve increased stability and prevent implant failure19.
Herein, we present the case of a young man with severe angular thoracolumbar kyphosis who we successfully treated with double VCRs at T11 and T12 combined with bilateral satellite rod placement (Fig. 1).
Figure 1.
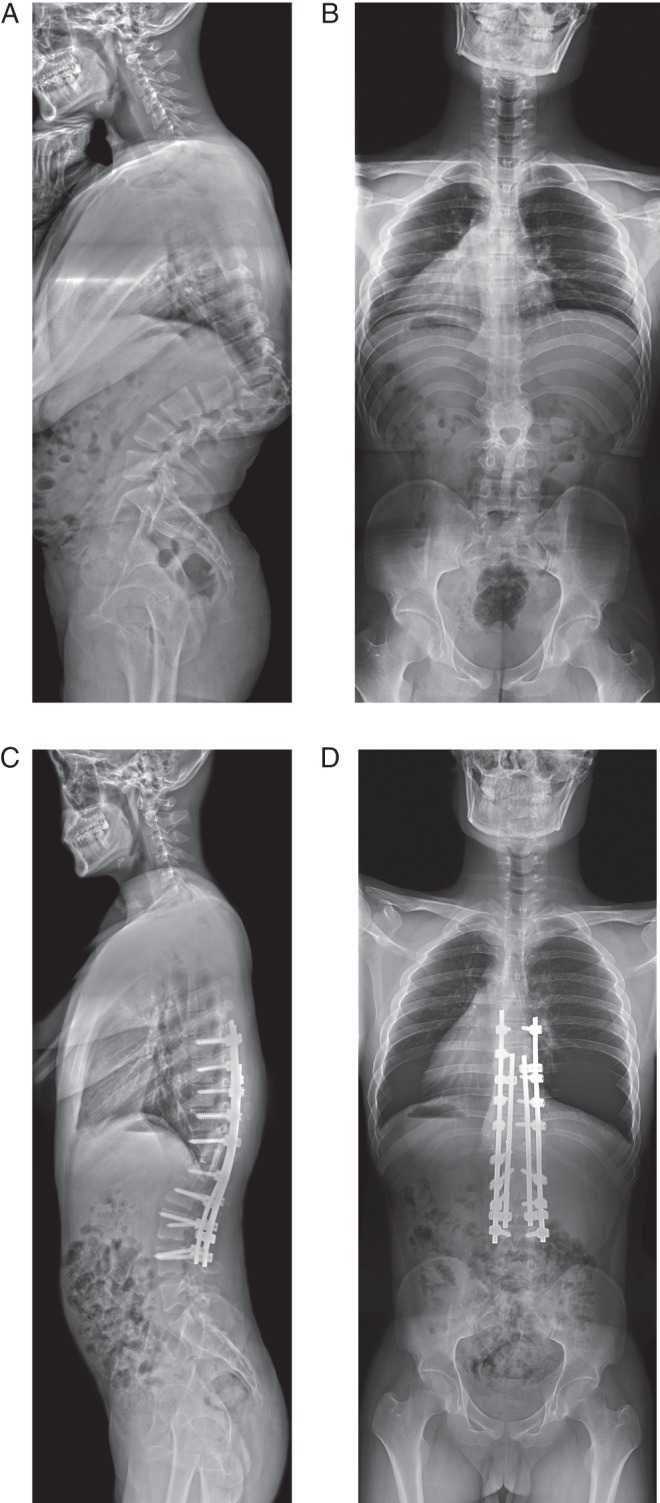
Radiographs of a 21‐year‐old man with marked kyphosis secondary to thoracolumbar anomalies. (A) There are hemivertebrae at T11 and T12, and a wedged vertebra at L1. They converge anteriorly, thus separating the posterior column. (B) A transverse plane of a vertebra (L2) is clearly visible in this standing posteroanterior film. After double VCRs at T11 and T12 and use of satellite rods, (C) kyphosis was satisfactorily corrected and (D) balance well maintained.
Case Presentation and Surgical Procedure
Patient
A 21‐year‐old man presented with a humped back that he had had for 4 years. He had no weakness, numbness or pain in the lower extremities. Upon physical examination, a symmetrical kyphosis and shortened trunk was noted. No sensory loss or abnormalities in muscle power or one were detected and he was able to walk without assistance.
Radiological Assessment
Standing lateral X‐ray films revealed marked kyphosis with a Cobb angle of 101° caused by anterior segmentation failure in the thoracolumbar region (T11 to L1). The apex of the kyphosis was located at T12, T11 and T12 both being hemivertebrae that converged with L1 at the anterior column. Interestingly, a transverse plane of a vertebra (L2), which was detected only on CT scan images, was clearly visible in a standing posteroanterior film.
A CT scan showed the three vertebrae from T11 to L1 were underdeveloped in terms of size and had converged anteriorly, thus being separated in the posterior column. There were hemivertebrae at T11 and T12, and a wedged vertebra at L1. No anomalies were found in the cephalad or caudal segments.
MR images demonstrated that the spinal cord was closely adjacent to the apex of the kyphosis and that there was segmentation failure at the anterior, but not the posterior, column from T11 to L1. There was no evidence of Chiari malformation, syringomyelia, split cord, or tethered cord.
Surgical Procedure
Preoperative discussion resulted in formulation of a plan to perform double VCRs at T11 and T12 to correct the severe kyphosis. The most sagittal stable vertebra (L4) was set as the lowest instrumented vertebra and T6 as the upper instrumented vertebra. The patient was placed in a prone position after induction of general anesthesia. The subsequent surgery was monitored with spinal cord monitoring (somatosensory and motor evoked potentials). After thorough dissection, pedicle screws were placed at the levels planned preoperatively using the freehand technique. A power‐driven device was used to assist rapid and accurate placement of the pedicle screws.
Osteotomy with VCR was started at the T12 level with a bilateral costotransversectomy of 2 cm of the rib. Following subperiosteal dissection of the rib, dissection was performed around the lateral aspect of the pedicles onto the anterolateral aspect of the vertebral body. During dissection, a custom‐made elevator was used, taking great care to avoid any injury to the visceral organs or anterior vasculature.
Next, a wide laminectomy was performed from T10 to T12. As is typical with these procedures, the entire laminae of the two levels to be resected (T11 and T12) and the laminae caudal to the inferior pole of the pedicles above (T10), and cephalad to the superior pole of the pedicles below (L1), were all removed.
Vertebral resection was begun by gaining access to the body through the pedicle entrance on the left side with the aid of a high‐speed burr. The cancellous bone of the vertebral body was curetted out and saved for grafting. Discectomies both above and below the corpectomy were carefully performed while avoiding violation to the endplates. Temporary stabilization was achieved with a unilateral rod fixed both above and below the osteotomy area prior to initiation of the subsequent procedures, this being extremely important to prevent dislocation of the vertebral column around the osteotomy level. Next, osteotomy was performed on the other side. The bony aspect anterior to the dural sac was resected with a high‐speed burr followed by a specialized elevator. Upon completion of T12 VCR, the osteotomy gap was temporarily closed with a temporary rod, after which osteotomy was begun at T11 in the same way.
When both vertebrae had been completely resected, closure of the osteotomy gap was attempted. At this point, it is important to ensure that all neural tissue is free of distraction or compression. The osteotomy gap was closed with compression forces, which were slowly applied to the implants bilaterally to avoid subluxation and/or dural impingement, careful and repeated dural palpation and visual inspection being performed to assess any such impingement. During the closure procedure, autologous grafts and a poly(ether‐ether‐ketone) cage were placed between the bony surfaces of the superior endplate of L1 and the inferior endplate of T10 as required. Once closure of the osteotomy area had been achieved, bilateral permanent rods made of CoCr were placed with appropriate correction maneuvers. To more strongly stabilize the instrumentation, satellite CoCr rods were implanted bilaterally and connected to the main corrective rods via dual‐head connectors on both sides.
The outcome of correction and the implants on both sides were checked by intraoperative radiographs and a circumferential check of the exposed dura performed to confirm the absence of impingement. Autologous bone graft obtained from the osteotomies was placed over the instrumented levels after posterior decortication. Both somatosensory evoked potentials and motor evoked potentials were continuously monitored throughout the procedure. A wake‐up test was performed to ensure there were no neurological complications.
The patient was instructed to sit 6 days after surgery and was discharged on the 10th postoperative day, when he was able to walk without assistance.
Discussion
The goal of treating kyphosis is to reestablish the sagittal profile through osteotomy procedures1, 2, 3, 4, 5, 6, 7. When treating severe congenital angular kyphosis, it is essential to excise the apex of the kyphosis with VCR and to provide sufficient anterior support. VCR enables maximal kyphosis correction upon complete removal of the deformed vertebra or vertebrae as well as bone‐on‐bone contact upon closure of osteotomy1, 2, 3, 4, 5. The two major complications of VCR surgeries are massive blood loss and neurological deficits2, 8, 10, 18, 21. VCR must therefore be performed prudently in the few cases that cannot be effectively treated by other methods. Rarely, VCR needs to be performed at two levels to correct a deformity.
In the current case, VCRs were performed at two adjacent levels to fully excise the anomalies and correct the kyphotic deformity of 101°. The double VCRs forcibly broke the severely kyphotic spine and achieved a new, balanced one. From a technical view of point, the extent of resection, namely how much to resect, is of critical importance. In the present case, the vertebral columns were fully excised from the lower endplate of T10 to the superior endplate of L1. Basically, the double VCRs started with the distal vertebra, followed by the proximal one. Upon completion of VCR at the first level, it was necessary to perform temporary closure before continuing to gradually correct the deformity. Moreover, a temporary rod across the VCR site was repeatedly engaged to stabilize the whole spine, the stability of which had been destroyed by the VCR. Use of a temporary rod at the osteotomy site is crucially important in prevention of intervertebral dislocation, which frequently leads to injury to the neural tissue or vasculature.
Although VCR surgery results in dramatic correction of kyphosis, mid‐ to long‐term follow‐up studies have reported an unacceptably high rate of rod breakage postoperatively14, 15, 16, 17, 18. The reasons for such rod breakage may include the relatively greater instability after VCR and relatively weaker strength of the instrumentations. Some surgeons attempt to revise this by connecting multiple rods to the broken rods. This practice can serve as a reminder to employ additional rods as well as the main corrective rods during primary VCR surgery for severe kyphosis. In recent years, we have routinely employed satellite rods across the osteotomy area in patients with severe spinal deformity undergoing three‐column osteotomies19, 20. As shown in a previous study, use of additional rods across three‐column osteotomy sites provides greater stability and a lower incidence of implant failure and symptomatic pseudarthrosis than with the conventional use of two rods22. These authors strongly recommend using a multi‐rod construct to stabilize three‐column osteotomies, including VCR22. In multi‐rod constructs, rods placed parallel laterally or medially to the main corrective rods serve as satellite rods and share the load at the osteotomy site19, 20, 22. In the current case, the thoracolumbar region was highly unstable after the double VCRs had been performed. Closure of the osteotomy was combined with gradual compression using CoCr rods to provide maximal correction and followed by addition of bilateral satellite rods to enhance the fixation strength. Powerful stability was then achieved, reducing stress in the implants and decreasing the risk of correction loss.
In conclusion, double VCRs were effective in the current case. We consider addition of satellite rods imperative to enhance instrumentation strength and thus prevent correction loss.
Supporting information
Video S1 supportingInformation
Acknowledgments
We thank Mr. Zhen‐yin Zhou and Song Li for their assistance in recording and editing the video.
Disclosure: This work was supported by the National Natural Science Foundation of China (Grant No. 81301603).
References
- 1. Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976), 2002, 27: 2374–2382. [DOI] [PubMed] [Google Scholar]
- 2. Li J, Lv GH, Wang XB, Wang B, Lu C. Delayed paraplegia following correction of severe thoracolumbar kyphotic deformity by posterior vertebral column resection. Orthop Surg, 2010, 2: 71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hamzaoglu A, Alanay A, Ozturk C, Sarier M, Karadereler S, Ganiyusufoglu K. Posterior vertebral column resection in severe spinal deformities: a total of 102 cases. Spine (Phila Pa 1976), 2011, 36: E340–E344. [DOI] [PubMed] [Google Scholar]
- 4. Lenke LG, O'Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM. Posterior vertebral column resection for severe pediatric deformity: minimum two‐year follow‐up of thirty‐five consecutive patients. Spine (Phila Pa 1976), 2009, 34: 2213–2221. [DOI] [PubMed] [Google Scholar]
- 5. Wang Y, Zhang Y, Zhang X, et al. Posterior‐only multilevel modified vertebral column resection for extremely severe Pott's kyphotic deformity. Eur Spine J, 2009, 18: 1436–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Helenius I, Serlo J, Pajulo O. The incidence and outcomes of vertebral column resection in paediatric patients: a population‐based, multicentre, follow‐up study. J Bone Joint Surg Br, 2012, 94: 950–955. [DOI] [PubMed] [Google Scholar]
- 7. Liu Z, Qiu Y, Zhu ZZ, et al. Pedicle subtraction osteotomy for correction of severe thoracolumbar kyphosis in ankylosing spondylitis. Orthop Surg, 2014, 6: 257–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Qiu Y, Wang S, Wang B, Yu Y, Zhu F, Zhu Z. Incidence and risk factors of neurological deficits of surgical correction for scoliosis. Analysis of 1373 cases at one Chinese institution. Spine (Phila Pa 1976), 2008, 33: 519–526. [DOI] [PubMed] [Google Scholar]
- 9. Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res, 2010, 468: 687–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lenke LG, Newton PO, Sucato DJ, et al. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine (Phila Pa 1976), 2013, 38: 119–132. [DOI] [PubMed] [Google Scholar]
- 11. Kelly MP, Lenke LG, Shaffrey CI, et al. Evaluation of complications and neurological deficits with three‐column spine reconstructions for complex spinal deformity: a retrospective Scoli‐RISK‐1 study. Neurosurg Focus, 2014, 36: E17, doi: 10.3171/2014.2.FOCUS1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Papadopoulos EC, Boachie‐Adjei O, Hess WF, et al. Early outcomes and complications of posterior vertebral column resection. Spine J, 2015, 15: 983–991. [DOI] [PubMed] [Google Scholar]
- 13. Ayhan S, Aykac B, Yuksel S, et al. Safety and efficacy of osteotomies in adult spinal deformity: what happens in the first year? Eur Spine J, 2015. [Epub ahead of print] doi: 10.1007/s00586-015-3981-3. [DOI] [PubMed] [Google Scholar]
- 14. Smith JS, Shaffrey E, Klineberg E, et al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine, 2014, 21: 994–1003. [DOI] [PubMed] [Google Scholar]
- 15. Smith JS, Shaffrey CI, Ames CP, et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery, 2012, 71: 862–867. [DOI] [PubMed] [Google Scholar]
- 16. Akazawa T, Kotani T, Sakuma T, Nemoto T, Minami S. Rod fracture after long construct fusion for spinal deformity: clinical and radiographic risk factors. J Orthop Sci, 2013, 18: 926–931. [DOI] [PubMed] [Google Scholar]
- 17. Wang F, Qiu Y, Qian B, et al. Risk factors for rod fracture in patients with severe kyphoscoliosis following posterior vertebral column resection. Zhonghua Gu Ke Za Zhi, 2012, 32: 946–950 (in Chinese). [Google Scholar]
- 18. Auerbach JD, Lenke LG, Bridwell KH, et al. Major complications and comparison between 3‐column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976), 2012, 37: 1198–1210. [DOI] [PubMed] [Google Scholar]
- 19. Liu Z, Qiu Y, Shi B, et al. Using satellite rod around the osteotomy area in patients with severe spinal deformity undergoing three‐column osteotomy. Zhonghua Gu Ke Za Zhi, 2015, 35: 349–356 (in Chinese). [Google Scholar]
- 20. Newton PO, Bastrom TP, Emans JB, et al. Antifibrinolytic agents reduce blood loss during pediatric vertebral column resection procedures. Spine (Phila Pa 1976), 2012, 37: E1459–E1463. [DOI] [PubMed] [Google Scholar]
- 21. Liu Z, Qiu Y, Yan H, et al. S2 alar‐iliac fixation: a powerful procedure for the treatment of kyphoscoliosis. Orthop Surg, 2016, 8: 81–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2‐rod constructs to multiple‐rod constructs for fixation across 3‐column spinal osteotomies. Spine (Phila Pa 1976), 2014, 39: 1899–1904. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1 supportingInformation


