Abstract
This study uses the Florida State Ambulatory Surgery and State Inpatient Databases to assess the trends in knee arthroscopy use among patients with osteoarthritis, meniscal tears, and knee pain.
Multiple clinical trials have shown that knee arthroscopy, compared with medical management, does not result in clinically significant benefits for patients with osteoarthritis, meniscal tears, and knee pain.1,2 It is unclear whether these trials have affected clinical practice. Reimbursement incentives favor surgery, and surgeons’ and patients’ beliefs may not reflect the evidence.3 In this article, I document the trends in the use of knee arthroscopy in Florida from January 1, 2002, to December 31, 2015.
Methods
I evaluated trends in outpatient arthroscopic knee procedures among patients aged 18 years or older using the Florida State Ambulatory Surgery and State Inpatient Databases for 2000 to 2015. The all-payer data included 100% of ambulatory and inpatient surgical procedures in the state. I selected Florida because of the availability of data for that state and because it has a large, diverse population. Following a previous study,4 I measured receipt of arthroscopic knee surgery using Current Procedural Terminology codes and International Classification of Diseases, Ninth Revision and Tenth Revision procedure codes to identify arthroscopic knee operations.
In addition, I identified trends in the use of total knee arthroplasties to gauge the possible substitution between knee arthroplasty and arthroscopy. I separately examined the trends in arthroscopic knee procedures by age group.
I report the surgical rate per 100 000 population aged 18 years or older, standardized by age and sex to the 2002 Florida population, using the direct method. I evaluated the significance of trends using least squares regression with a time trend variable. The study was exempt from institutional review board review under federal regulation 45 CFR §46.101 because the data were previously collected and deidentified.
Results
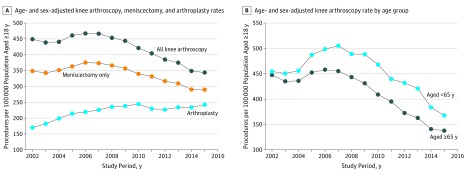
In total, 868 482 arthroscopic knee procedures were performed in Florida between 2002 and 2015. Of the 868 482 procedures, 704 563 (81.1%) were meniscectomies. The knee arthroscopy rate declined over the study period, from 449 procedures per 100 000 population aged 18 years or older in 2002 to 345 in 2015 (change, 23%; P < .001) (Figure, A). The meniscectomy rate declined from 349 in 2002 to 291 in 2015 (change, 17%; P = .002), and the adjusted knee arthroplasty rate increased from 170 in 2002 to 244 in 2015 (change, 44%; P < .001).
Figure. Knee Arthroscopy and Arthroplasty Procedures in Florida From 2002 to 2015.
Data are from the Florida State Ambulatory Surgery and State Inpatient Databases for 2002 to 2015.
The adjusted knee arthroscopy rate in the population aged 18 to 64 years declined from 447 in 2002 to 339 in 2015 (change, −24%; P < .001). The rate in the population aged 65 years or older declined from 454 in 2002 to 368 in 2015 (change, −19%; P = .01) (Figure, B).
Discussion
Knee arthroscopy rates in Florida declined by 23% between 2002 and 2015. The decline in arthroscopy rates was especially pronounced after 2008. The trial by Kirkley et al5 was published in 2008, which was the second major trial that failed to detect a difference between arthroscopy and medical management in the treatment of osteoarthritis of the knee. The knee arthroplasty rate increased, but most of the increase preceded the decline in arthroscopy rates.
Between 1999 and 2014, the prevalence of osteoarthritis in the US adult population more than doubled from 6.6% to 14.3%.6 Trends in per capita knee surgical procedures, which are not adjusted for the increase in the prevalence of osteoarthritis, likely understate the degree to which use of arthroscopic surgery as a treatment for knee pain has declined.
Some private insurers have started to require physicians to obtain authorization before an arthroscopic knee procedure. The fee-for-service Medicare program does not require prior authorization. Private insurers covered 72% of knee arthroscopies in patients younger than 65 years, and Medicare covered 83% of these procedures in patients aged 65 years or older. I could not observe the impact of prior authorization requirements directly, but trends in arthroscopy rates in these age groups were similar, indicating that the requirements may not be a major factor behind the decline in rates.
The results suggest that the accumulating evidence on the lack of benefit associated with knee arthroscopy, compared with medical management, has altered treatment decisions. Despite the lower use rates, knee arthroscopy is still a common procedure. There may be additional opportunities to reduce the use of knee arthroscopy without adversely affecting patient outcomes.
References
- 1.Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014;186(14):1057-1064. doi: 10.1503/cmaj.140433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ. 2015;350:h2747. doi: 10.1136/bmj.h2747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barlow T, Plant CE. Why we still perform arthroscopy in knee osteoarthritis: a multi-methods study. BMC Musculoskelet Disord. 2015;16:85. doi: 10.1186/s12891-015-0537-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard D, Brophy R, Howell S. Evidence of no benefit from knee surgery for osteoarthritis led to coverage changes and is linked to decline in procedures. Health Aff (Millwood). 2012;31(10):2242-2249. doi: 10.1377/hlthaff.2012.0644 [DOI] [PubMed] [Google Scholar]
- 5.Kirkley A, Birmingham TB, Litchfield RB, et al. . A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359(11):1097-1107. doi: 10.1056/NEJMoa0708333 [DOI] [PubMed] [Google Scholar]
- 6.Park J, Mendy A, Vieira ER. Various types of arthritis in the United States: prevalence and age-related trends from 1999 to 2014. Am J Public Health. 2018;108(2):256-258. doi: 10.2105/AJPH.2017.304179 [DOI] [PMC free article] [PubMed] [Google Scholar]