Figure 3.
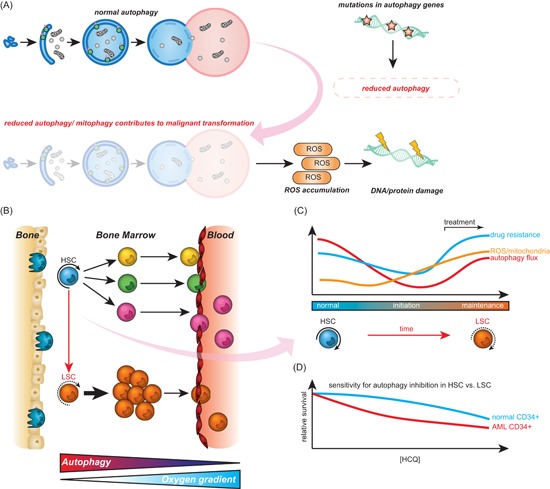
Autophagy during malignant transformation and cancer maintenance. A, Different pro‐oncogenic events such as mutation or monoallelic deletion of autophagy‐related genes can cause reduced autophagy activity. Reduced levels of autophagy/mitophagy can contribute to malignant transformation due to elevated levels of reactive oxygen species (ROS). B, Hematopoietic stem cells (HSCs) reside in specific bone marrow niches with low oxygen content and are characterized by high autophagy activity. During differentiation, the autophagy flux declines and mature cells leave the bone marrow (BM) environment and enter the blood‐stream. In leukemia, HSCs have acquired mutations which results in a block in differentiation and consequently accumulation of immature blasts in BM and peripheral blood of patients. C, Hypothetical model for changes in autophagy and ROS in HSCs during transformation. Normal HSCs have high autophagy flux, low mitochondrial activity, and ROS levels. During cancer initiation, autophagy is repressed (although not completely inhibited), causing accumulation of mitochondria and ROS, which in turn contributes to malignant transformation. During cancer maintenance, cancer cells re‐establish functional autophagy promoting tumor growth and survival. In addition, in response to drug treatment, autophagy is activated and acts as a survival mechanism for cancer cells. D, Both normal BM‐derived CD34+ and acute myeloid leukemia (AML) CD34+ cells need a certain level of autophagy to survive. Therefore, there is only a small therapeutic window of autophagy inhibition with autophagy inhibitors like hydroxychloroquine. LSC, leukemic stem cells [Color figure can be viewed at wileyonlinelibrary.com]
