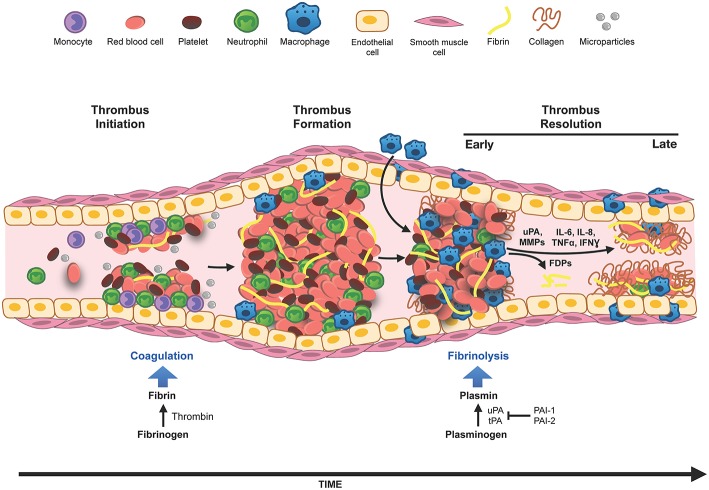
Figure 1.
Innate immune cells in DVT. Venous thrombosis can be initiated by venous stasis, increased blood hypercoagulability or endothelial damage. Innate immune cells, neutrophils, and monocytes, bind to the activated vascular endothelium and along with platelets, initiate thrombus formation and fibrin deposition. The thrombus grows by deposition of more fibrin, accumulation of red blood cells and immune cells. Thrombus infiltrating neutrophils and macrophages (differentiated from monocytes) modulate generation of plasmin and matrix metalloproteinases (MMPs), and thus set the stage for fibrinolysis and the collagen remodeling required for the resolution of the thrombus. In the early phase of thrombus resolution, fibrinolysis occurs at a high rate generating fibrin degradation products (FDPs), intrathrombus collagen fibrils start to appear, and thrombus-associated immune cells are induced to produce inflammatory cytokines and various proteases. As the thrombus matures, the rate of fibrinolysis slows down, intrathrombus collagen deposition increases, matrix remodeling via macrophage secreted MMPs occurs and eventually blood flow through the thrombus is restored. Resolution of inflammation and acceleration of this process is believed to be beneficial for restoring vein wall patency and reducing the pathology associated with PTS.