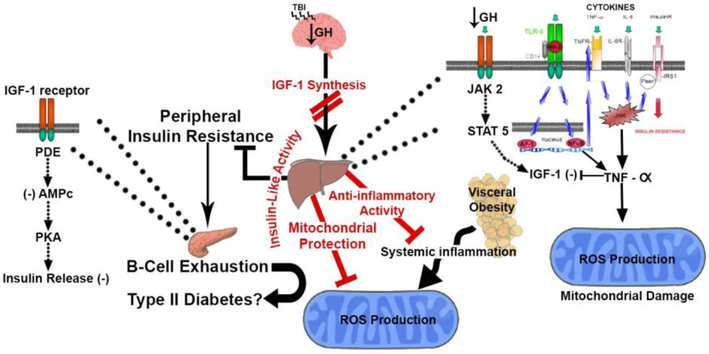
Figure 2.
Proposed mechanism by which TBI alters hypothalamic-pituitary growth hormone (GH) Axis. TBI-induced chronic growth hormone deficiency (GHD) is characterized by metabolic abnormalities associated with decreased IGF-1 synthesis. The presence of low plasma GH decreases the hepatic IGF-1 synthesis via dysregulation of the GH receptor, JAK2 and STAT5 pathways. Early hepatic inflammation after TBI also activates the hepatic toll like receptors (TLR-4) that leads to nuclear translocation of the transcription factor NF-κB, TNF-αreceptor upregulation and TNF-α increase. This systemic inflammation could induce insulin resistance by stimulating cytokines receptors and JNK pathway that leads to serine/threonine phosphorylation of IRS1, TNF-α and mitochondrial ROS production. It is recognized that the growth hormone GH/IGF system is involved in metabolism manifestations. In turn, TBI-induced GH/IGF-1 deficiency may be associated with visceral obesity that leads to systemic inflammation and ROS production. Low plasma IGF-1 induces β-cell exhaustion and consequently peripheral insulin resistance by dysregulation of the IGF-1 receptor, PDE and PKA pathway.