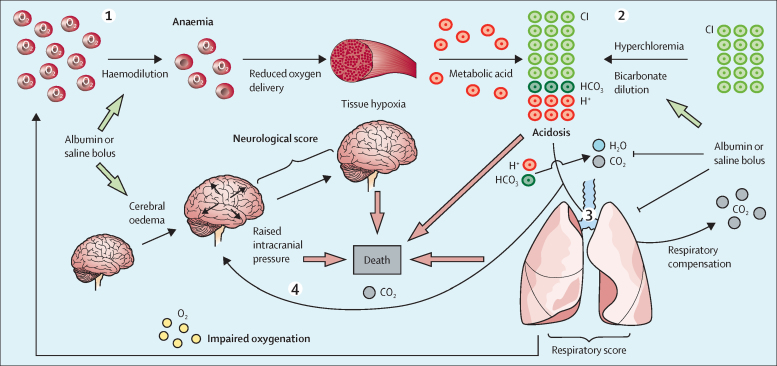
Figure 5.
Proposed physiological model of the adverse effects of fluid bolus
Bolus fluid reduces haemoglobin concentration, resulting in decreased tissue oxygenation, increasing anaerobic metabolism, and metabolic acidosis. According to the Stewart model, maintenance of normal plasma pH is controlled by (1) the strong ion difference (charge difference between strong cations (Na+, K+, Ca2+, and Mg2+), and strong anions (Cl– and lactate–); (2) pCO2 and (3) charge from weak acids (phosphate, albumin).28, 29 Bolus of normal saline or 5% albumin (which have similar electrolyte content) caused hyperchloraemia and dilution of bicarbonate, resulting in a reduction in the strong ion difference. Hyperchloraemic acidosis increases the need for respiratory compensation through increased carbon dioxide excretion to maintain pH. Worsening of respiratory function due to bolus results in hypoxia (as evidenced by low oxygen saturation and increased respiratory score). This outcome, together with an inability to increase respiratory rate, impairs excretion of carbon dioxide (not shown in our study). Increasing carbon dioxide causes cerebral vasodilation, resulting in increased intracranial pressure. Fluid bolus might also directly cause cerebral oedema. The combination of adverse effects on haemoglobin concentration, acidosis, and respiratory and neurological function induced by modest albumin or saline fluid boluses might overwhelm compensatory mechanisms in the most severely ill patients, resulting in increased mortality.