Abstract
This systematic review of overlapping meta‐analyses was conducted to propose a principle to make decisions for comparing clinical safety and efficacy of surgical and non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus. Three electronic databases (PubMed, EMBASE, and the Cochrane Library) were systematically searched to retrieve available published systematic reviews and meta‐analyses comparing surgical versus non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus. Ten meta‐analyses were identified for this investigation. Based on the application of selection with the Jadad algorithm, a meta‐analysis including 6 randomized clinical trials was selected for this systematic review, which demonstrated the best available evidence that no statistically significant differences were found in the Constant score, health‐related quality of life, and mortality between surgical and non‐surgical treatments for displaced 3‐part and 4‐part fractures of the proximal humerus; however, surgical treatment was associated with a significant increase in the incidence of reoperation. This systematic review of overlapping meta‐analyses reveals that although surgical treatment is more advantageous than and superior to non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus, the former leads to a higher incidence of postoperative complications.
Keywords: Fractures of the proximal humerus, Overlapping meta‐analysis, Systematic review
Introduction
Proximal humeral fractures are very common and potentially disabling injuries, which mostly occur in the elderly. The global incidence of fractures is 4%–9%1, 2, 3, 4, 5, and is up to 66 per 10 000 per year6, 7, 8. Proximal humeral fractures have become the third most common fracture after hip and wrist fractures, rapidly increasing in frequency as the population ages, and the global annual incidence has risen over the past few decades. Fragile bones and risk of falling are considered the two predominant risk factors for proximal fractures of the humerus.
In general, interventions for proximal humeral fractures are classified as surgical and non‐surgical. Most minimally displaced or non‐displaced proximal humeral fractures can be treated with non‐surgical methods. Displaced 3‐part and 4‐part fractures, accounting for approximately 12.6% of all proximal humeral fractures, are among the most challenging fractures, and may seriously affect quality of life and result in additional complications9.
Both operative and non‐operative interventions are used to treat these complicated fractures. A broad spectrum of surgical methods is available, such as open reduction and internal fixation (ORIF) with Kirschner wire fixation, screw fixation, plate fixation, and hemiarthroplasty. ORIF has become increasingly popular for these fractures as a result of technical advances in locking plate fixation10. A study published in 2011 reported that the rates of operative treatment and ORIF for these fractures increased significantly, by 25.6% and 28.5%, respectively, between 1999 and 2005 in the United States11.
Numerous randomized clinical trials (RCT) or quasi‐RCT comparing surgical with non‐surgical treatment have been published for displaced 3‐part and 4‐part fractures of the proximal humerus, but the studies have yielded discordant findings. Because of this discrepancy, multiple systematic reviews and meta‐analyses have been published to evaluate surgical versus non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus12, 13, 14, 15, 16, 17, 18, 19, 20, 21; however, surgeons are not in agreement regarding the optimal interventions for these fractures. Several studies have shown that surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus is associated with a significant increase in the incidence of complications when compared with non‐surgical intervention12, 13, 14, 15, while other studies suggest that there are no significant differences between these two methods16, 17, 18, 19, 20. These controversial results from numerous meta‐analyses pose a dilemma for decision‐makers in the clinic.
Multiple systematic reviews of overlapping meta‐analyses have been published regarding orthopaedic diseases, including distal radial fractures22 and osteoporotic vertebral compression fractures23, which have been remarkably useful for decision‐makers to choose the best treatment strategy by estimating the overlapping meta‐analyses with the controversial findings involving the same topic in the clinic.
Potential redundancy was defined as overlap in terms of comparisons of interventions, type of populations, and outcomes between meta‐analyses. There had to be at least one overlapping analysis (same comparison, type of population/indication, and outcome) for them to be considered as overlapping. Three quality tools for the assessment of the overlapping meta‐analyses, Oxford Levels of Evidence, Assessment of Multiple Systematic Reviews Instrument, and Jadad algorithm, were adopted to assess the methodological quality for each included study to select the currently best available evidence.
In addition, there are no systematic reviews of overlapping meta‐analyses conducted to compare the clinical safety and efficacy of surgical and non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus. Therefore, the aim of this study was to propose a principle to offer intervention recommendations for displaced 3‐part and 4‐part fractures of the proximal humerus based on the currently best available evidence.
Materials and Methods
This systematic review of overlapping meta‐analyses was conducted following the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA)24. Because the systematic review was based on the published literature, ethical approval and informed consent of patients were not required.
Inclusion and Exclusion Criteria
Inclusion of a systematic review or meta‐analysis had to meet the following four inclusion criteria: (i) patients with displaced 3‐part and 4‐part fractures of the proximal humerus; (ii) intervention including surgical and non‐surgical treatment; (iii) comparing surgical and non‐surgical treatment of patients with displaced 3‐part and 4‐part fractures of the proximal humerus; and (iv) studies assessing at least one quantitative indicator (disabilities of the arm, shoulder and hand [DASH], Constant score, American Shoulder and Elbow Surgeons [ASES] score, visual analogue scale [VAS], simple shoulder test [SST], and complications [avascular necrosis, impingement and stiffness, and axillary nerve lesions]).
The excluded criteria were as follows: (i) review only providing descriptive viewpoints without quantitative calculation on the outcomes of interest; or (ii) meeting abstracts and correspondence were excluded because insufficient detailed data and assessment of methodological quality were presented.
Search Strategy
A computerized search of three electronic medical databases (PubMed, Embase, and Cochrane Library) was performed comprehensively until 30 December 2018 with no restrictions on language. The search strategy was the use of mesh terms: (i) “Humerus [MeSH]” or “Humeral Fractures [MeSH]” AND “Systematic Review [MeSH]” or “Meta‐Analysis [MeSH].” Subsequently, relevant reference lists of included meta‐analyses were also manually retrieved to identify any additional systematic reviews or meta‐analyses.
Selection Process
Two investigators independently and in duplicate conducted the selection process. We first excluded explicit publications by screening titles and abstracts. Then, all potentially feasible publications were retrieved and we downloaded full texts using the eligibility criteria. All discrepancies were resolved by discussion and consensus of two investigators (Fan‐xiao Liu and Hong‐lei Jia).
Data Extraction
All quality information and data, including the first author's name, year of publication, search database, search date, primary study design, number of included RCT or quasi‐RCT, level of evidence, and outcomes were independently and carefully extracted from each original publication into a standardized Excel file by two investigators (Fan‐xiao Liu and Hong‐lei Jia) and checked by a third investigator (Dong‐sheng Zhou). All disagreement was resolved by discussion and consensus of three investigators (Fan‐xiao Liu, Hong‐lei Jia, and Dong‐sheng Zhou).
Assessment of Methodological Quality
The methodological quality of the included meta‐analyses was evaluated independently by two investigators (Fan‐xiao Liu and Hong‐lei Jia) according to the Assessment of Multiple Systematic Reviews (AMSTAR) Instrument25, 26, 27 and the Oxford Levels of Evidence28, 29. The AMSTAR Instrument is composed of 11 items and is a valuable measurement tool with good reliability and validity for evaluating the methodological quality of systematic reviews or meta‐analyses25, 26, 27. In addition, the Oxford Levels of Evidence is a hierarchy of the likely best evidence, which was designed and used as a shortcut for busy clinicians, researchers, or patients to find the presumptive best evidence28, 29. The Oxford Levels of Evidence provides the most reliable answers for treatment benefit and harm in systematic reviews of randomized control trials. The consistency of each item from the two methods was reviewed and discussed for consensus.
Heterogeneity Assessment
The heterogeneities of mean differences and dichotomous variables across studies were assessed using the I 2 statistic, a quantitative measure which describes the percentage of total variation due to heterogeneity. A higher I 2 indicates higher heterogeneity. According to the Cochrane Handbook, for an I 2 ≤ 50%, heterogeneity across studies was acceptable in a systematic review or meta‐analysis30. Two investigators (Fan‐xiao Liu and Hong‐lei Jia) evaluated whether the original literature presented the results of sensitivity analyses, subgroup analyses, and publication bias for assessing the stability of pooled estimations to explore possible sources of heterogeneity.
Application of Jadad Decision Algorithm
The Jadad decision algorithm, reported first by Jadad et al., is a methodology for providing best treatment recommendations to identify discordant meta‐analyses31. In the present study, multiple sources of discordance of systematic reviews or meta‐analyses included different clinical questions, inclusion and exclusion criteria, search strategies, selection processes, information extraction, quality assessments, and data synthesis analyses. Three authors reached a consensus to choose publications presenting the best currently available evidence using the algorithm.
Results
Study Selection
In brief, a total of 202 titles and abstracts were retrieved through the primary search in three electronic databases and references of relevant articles. After excluding titles and abstracts, 24 studies were identified and downloaded as full‐text articles assessed for eligibility. Subsequently, 4 publications were excluded because the publications were not meta‐analyses or included pooled data, and 3 other publications were excluded because the publications included non‐RCT as an integral part of the study. Finally, 10 meta‐analyses published between 2013 and 2017 met the inclusion criteria and were included in our investigation12, 13, 14, 15, 16, 17, 18, 19, 20, 21. The search process and exclusion reasons are described in detail in Fig. 1.
Figure 1.
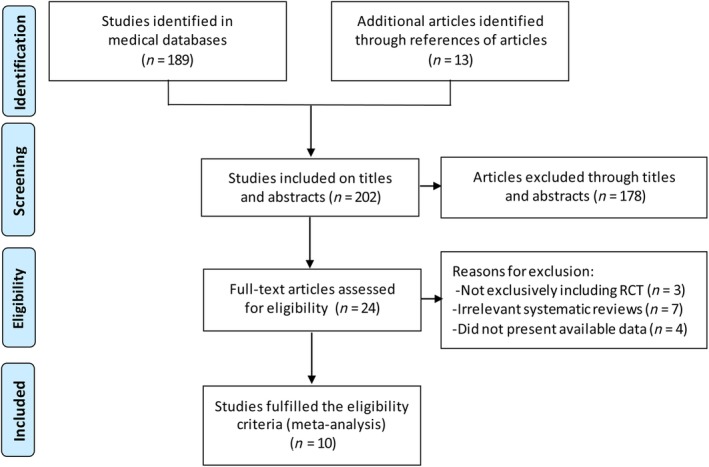
Flow chart of inclusion and exclusion for included meta‐analyses. RCT, randomized clinical trial.
Main Characteristics
All included meta‐analyses were published in English, except the study by Li et al.20. Among the 10 meta‐analyses12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 9 publications12, 13, 14, 15, 16, 17, 19, 20, 21 search the databases with no language restrictions; the remaining 1 publication18 searched with the restriction of English. The sample size of primary RCT in meta‐analyses ranged from 3 to 7. A comprehensive and careful description of the main characteristics of each meta‐analysis is shown in Table 1. Every primary RCT of each included meta‐analysis is listed in Table 2.
Table 1.
General description of the characteristics of each meta‐analysis
| Study, year | Journal of publication | Date of last literature search | Language of search | Date of publication | Number of included RCT | Number of quasi‐RCT |
|---|---|---|---|---|---|---|
| Handoll et al. (2013)12 | The Cochrane Library | January 2012 | No restrictions | 18 April 2012 | 6 | 18 |
| Li et al. (2013)16 | Plos one | October 2012 | No restrictions | 16 September 2013 | 3 | 0 |
| Mao et al. (2014)17 | ORTHOPEDICS | March 2013 | No restrictions | 14 May 2014 | 6 | 0 |
| Jia et al. (2014)14 | ORTHOPEDICS | November 2012 | No restrictions | 6 November 2014 | 7 | 0 |
| Fu et al. (2014)13 | International Journal of Clinical and Experimental Medicine | June 2013 | No restrictions | 30 December 2014 | 6 | 0 |
| Sun et al. (2015)15 | Int J Clin Exp Med | August 2013 | No restrictions | 30 May 2015 | 3 | 3 |
| Mao et al. (2015)18 | Journal of Investigative Surgery | 31 October 2013 | English | August 2015 | 5 | 0 |
| Rabi et al. (2015)19 | World Journal of Orthopedics | 20 Feb, 2014 | No restrictions | 18 November 2015 | 6 | 0 |
| Li et al. (2016)20 | Journal of Zhengjiang University (MedicalSciences) | Jul, 2016 | No restrictions | 14 November 2016 | 6 | 0 |
| Du et al. (2017)21 | International Journal of Surgery | 31 Jul, 2017 | No restrictions | 7 Sep, 2017 | 7 | 0 |
RCT, randomized controlled trials.
Table 2.
Primary RCT included in meta‐analyses
| Study, years | Stableforth et al. 1984 | Kristiansen et al. 1988 | Zyto et al. 1997 | Fjalestad et al. 2010 | Olerud et al. 2011 | Olerud et al. 2011* | Boons et al. 2012 | Fjalestad et al. 2012 |
|---|---|---|---|---|---|---|---|---|
| Handoll et al. (2013)12 | √ | √ | √ | √ | √ | √ | ||
| Li et al. (2013)16 | √ | √ | √ | |||||
| Mao et al. (2014)17 | √ | √ | √ | √ | √ | √ | √ | |
| Jia et al. (2014)14 | √ | √ | √ | √ | √ | √ | √ | |
| Fu et al. (2014)13 | √ | √ | √ | √ | √ | √ | ||
| Sun et al. (2015)15 | √ | √ | √ | |||||
| Mao et al. (2015)18 | √ | √ | √ | √ | √ | |||
| Rabi et al. (2015)19 | √ | √ | √ | √ | √ | √ | ||
| Li et al. (2016)20 | √ | √ | √ | √ | √ | √ | ||
| Du et al. (2017)21 | √ | √ | √ | √ |
RCT, randomized controlled trails.
stands for different studies.
Search Methodology
All 10 meta‐analyses12, 13, 14, 15, 16, 17, 18, 19, 20, 21 were conducted with a comprehensive search for original studies in PubMed and Cochrane Library. Of the 10 meta‐analyses12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 912, 13, 14, 15, 17, 18, 19, 20, 21 searched Embase. Studies inconsistently searched Google Scholar, Cinahl Datebases, China National Knowledge Internet (CNKI), and China Biology Medicine disc (CBM). The details of databases applied by literature searches of each included meta‐analysis are presented in Table 3.
Table 3.
Databases used by each meta‐analysis in their study searches
| Study, year | PubMed | Embase | Cochrane Library | Google Scholar | CINAHL | CNKI | CBM | CMCC | Others |
|---|---|---|---|---|---|---|---|---|---|
| Handoll et al. (2013)12 | √ | √ | √ | √ | √ | ||||
| Li et al. (2013)16 | √ | √ | √ | ||||||
| Mao et al. (2014)17 | √ | √ | √ | √ | |||||
| Jia et al. (2014)14 | √ | √ | √ | √ | √ | √ | √ | √ | |
| Fu et al. (2014)13 | √ | √ | √ | √ | |||||
| Sun et al. (2015)15 | √ | √ | √ | √ | √ | ||||
| Mao et al. (2015)18 | √ | √ | √ | √ | √ | ||||
| Rabi et al. (2015)19 | √ | √ | √ | √ | √ | ||||
| Li et al. (2016)20 | √ | √ | √ | √ | √ | √ | |||
| Du et al. (2017)21 | √ | √ | √ | √ |
Methodological Quality
All 10 meta‐analyses included RCT or quasi‐RCT provided Level II or III evidence. Among the 10 meta‐analyses, 612, 13, 15, 17, 18, 21 declared that the meta‐analysis adopted the Cochrane Handbook as the quality tool in the research process, 414, 16, 19, 21 followed PRISMA, 712, 15, 16, 17, 18, 19, 20 performed pool analyses using RevMan, and only 213, 14 used STATA software for pooled data. Detailed methodologic information is presented in Table 4. The AMSTAR scores of the 10 included publications ranged from 8 to 11, with a median and mean of 9. A total of 5 meta‐analyses13, 14, 17, 18, 21 had scores of 9, 315, 16, 20 had scores of 8, 119 had a score of 10, and 1 had a score of 1112. One meta‐analysis19 met 10 of 11 items of the AMSTAR criteria with more and higher quality publications. The AMSTAR outcomes for each question from each included meta‐analysis are shown in Table 5.
Table 4.
Methodological information for each included meta‐analysis
| Authors, year | Included study design | Level of evidence | Software | Assessment of study quality | Sensitivity analysis | Publication bias | PRISMA |
|---|---|---|---|---|---|---|---|
| Handoll et al. (2013)12 | RCT | Level II | RevMan | Cochrane Handbook | Yes | Yes | No |
| Li et al. (2013)16 | RCT | Level II | RevMan version 5.0 | Jadad score | Yes | Yes | Yes |
| Mao et al. (2014)17 | RCT | Level II | RevMan version 5.1 | Cochrane Handbook | No | No | No |
| Jia et al. (2014)14 | RCT | Level II | STATA version 11.0 | Jadad score | Yes | No | Yes |
| Fu et al. (2014)13 | RCT | Level II | STATA version 12.0 | PEDro scale | Yes | Yes | No |
| Sun et al. (2015)15 | RCT or quasi‐RCT | Level III | RevMan version 5.0 | Cochrane Handbook | No | Yes | No |
| Mao et al. (2015)18 | RCT | Level II | RevMan version 5.1 | Cochrane Handbook | Yes | Yes | No |
| Rabi et al. (2015)19 | RCT | Level II | RevMan version 5.2 | Cohen's kappastatistic | Yes | Yes | Yes |
| Li et al. (2016)20 | RCT | Level II | RevMan version 5.3 | Jadad score | No | Yes | No |
| Du et al. (2017)21 | RCT | Level II | R i386 3.3.2 | Cochrane Handbook | Yes | Yes | Yes |
RCT, randomized controlled trials.
Table 5.
AMSTAR criteria for each included meta‐analysis
| Included studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Handoll et al. (2013)12 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Li et al. (2013)16 | N | Y | N | Y | N | Y | Y | Y | Y | Y | Y | 8 |
| Mao et al. (2014)17 | N | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | 9 |
| Jia et al. (2014)14 | N | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | 9 |
| Fu et al. (2014)13 | N | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 9 |
| Sun et al. (2015)15 | N | Y | N | Y | N | Y | Y | Y | Y | Y | Y | 8 |
| Mao et al. (2015)18 | N | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 9 |
| Rabi et al. (2015)19 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 10 |
| Li et al. (2016)20 | N | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 8 |
| Du et al. (2017)21 | N | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 9 |
1: Was an a priori design provided?; 2: Was there duplicate study selection and data extraction?; 3: Was a comprehensive literature search performed?; 4: Was the status of publication (ie, grey literature) used as an inclusion criterion?; 5: Was a list of studies (included and excluded) provided?; 6: Were the characteristics of the included studies provided?; 7: Was the scientific quality of the included studies assessed and documented?; 8: Was the scientific quality of the included studies used appropriately in formulating conclusions?; 9: Were the methods used to combine the findings of studies appropriate?; 10: Was the likelihood of publication bias assessed?; 11: Was the conflict of interest stated?
Heterogeneity Assessment
Of the 10 meta‐analyses, 8 used the funnel plot and Egger's test to identify publication bias12, 13, 15, 16, 18, 19, 20, 21. All the meta‐analyses used the I 2 value as a statistical measure to evaluate heterogeneity across studies. The I 2 value for each result of 10 meta‐analyses is demonstrated in Table 6. Heterogeneities (I 2 < 50%) of the majority variables in 10 meta‐analyses were tolerant. In addition, 7 meta‐analyses12, 13, 14, 16, 18, 19, 21 performed sensitivity analyses to test whether the results would qualitatively change if a different assumption was used.
Table 6.
I 2 statistic value of each variable at different follow up in each meta‐analysis
| Outcomes | Handoll et al. (2013)12 | Li et al. (2013)16 | Mao et al. (2014)17 | Jia et al. (2014)14 | Fu et al. (2014)13 | Sun et al. (2015)15 | Mao et al. (2015)18 | Rabi et al. (2015)19 | Li et al. (2016)20 | Du et al. (2017)21 |
|---|---|---|---|---|---|---|---|---|---|---|
| Constant score | 0% | 0% | 0% | 0% | 42% | 0% | ‐ | |||
| Constant score at 4 months | 60% | |||||||||
| Constant score at 6 months | — | |||||||||
| Constant score at 12 months | 0% | 0% | — | 0% | 24% | |||||
| Constant score at 24 months | 0% | 0% | — | |||||||
| Constant score at 50 months | — | — | ||||||||
| DASH | 0% | |||||||||
| DASH at 4 months | 0% | |||||||||
| DASH at 12 months | 0% | 0% | — | |||||||
| DASH at 24 months | 0% | 0% | — | |||||||
| ASES score | — | |||||||||
| ASES at 6 months | — | — | ||||||||
| ASES at 12 months | — | — | ||||||||
| SST at 3 months | — | |||||||||
| SST at 12 months | — | |||||||||
| VAS score | 0% | |||||||||
| Functional outcome | 0% | 0% | ||||||||
| Poor or unsatisfactory function | — | |||||||||
| ROM | — | — | ||||||||
| Quality of life | — | 3.1% | 0% | |||||||
| EQ‐5D | 0% | 0% | ||||||||
| EQ‐5D at 4/6 months | 48%/10% | 0%/− | ||||||||
| EQ‐5D at 12/24 months | 0%/0% | 0%/0% | 0%/0% | |||||||
| 15D | 0% | |||||||||
| 15D at 3/6/12 months | 0%/0%/0% | — | — | |||||||
| Activities of daily living | — | |||||||||
| Total complications | 85% | 23% | 8% | |||||||
| Additional surgery | 0% | 0% | 0% | 0% | ||||||
| Additional surgery at 12 months | 0% | 0% | ||||||||
| Additional surgery at 24 months | 0% | 0% | ||||||||
| Fixation failure resulting in an operation | — | |||||||||
| Axillary nerve lessions | 0% | — | ||||||||
| AVN | 0% | 0% | 41.9% | — | 0% | 0% | ||||
| Bone resorption | — | 60% | — | |||||||
| Hematoma | — | |||||||||
| Implant penetration | 0% | 0% | — | |||||||
| Impingement and stiffness | — | — | ||||||||
| Infection | 4 | 0% | — | 0% | ||||||
| Mortality | 0% | 0% | 0% | |||||||
| Nonunion | 0% | 0% | 0% | — | 0% | 0% | ||||
| Number of QALY at 1 year | 0% | |||||||||
| Osteoarthritis | 42% | 13% | 52% | — | 0% | 36% | 27% | |||
| Pain and impairment | — | — | ||||||||
| Pulmonary embolism | — | |||||||||
| Redisplacement of fracture | 0% | 0% | — | |||||||
| Refracture | — |
15D, 15 Dimensions; ASES, American Shoulder and Elbow Surgeons; AVN, Avascular Necrosis; DASH, disabilities of the arm, shoulder and hand; ROM; Range of Motion; SST, Simple Shoulder Test; VAS, Visual Analogue Scale.
Results of Jadad Decision Algorithm
We adopted the Jadad decision algorithm as a measure to identify a meta‐analysis providing the best available evidence. Given that each included publication selecting the same topic closest to the problem to be solved did not enroll the same original RCT based on similar search strategies and selection criteria, the Jadad algorithm suggested that a high‐quality meta‐analysis with the best available evidence could be selected based on publication status and methodology quality of primary trials, whether or not language restrictions and data analysis for individual patients exist. The outcomes of each included meta‐analysis are presented in Fig. 2. Eventually, a meta‐analysis19 including 6 RCT was selected as a high‐quality report (Fig. 3). Based on the present systematic review of overlapping meta‐analyses that compared surgical with non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus, the best available evidence indicated that surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus is more advantageous than and superior to non‐surgical treatment, and should be considered an effective option for the treatment of patients with displaced 3‐part and 4‐part fractures of the proximal humerus.
Figure 2.
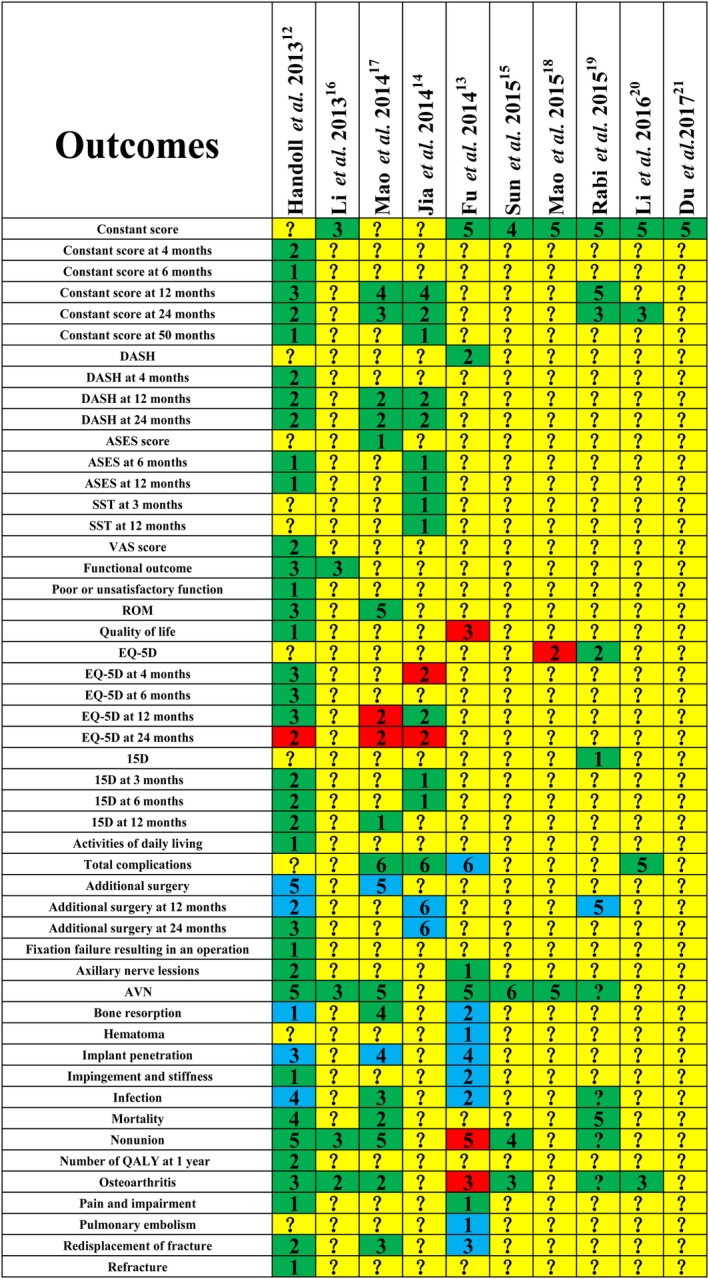
Outcomes of each included meta‐analysis. Red means favoring surgery group; green means no difference; yellow means not reporting, and blue means favoring conservative therapy group. Arabic numerals mean the number of included randomized controlled trials. ASES, American Shoulder and Elbow Surgeons; AVN, avascular necrosis; DASH, disabilities of the arm, shoulder and hand; ROM, range of motion; SST, simple shoulder test; VAS, visual analogue scale; 15D, 15 dimensions.
Figure 3.
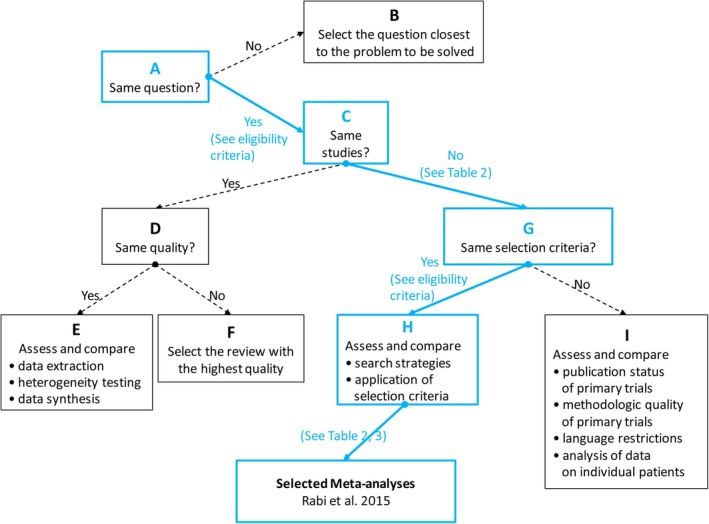
Flow chart of Jadad decision algorithm.
Discussion
The treatments for displaced 3‐part and 4‐part fractures of the proximal humerus remain a hot topic. A retrospective cohort study involving 113 patients with an average follow‐up time of 26.2 months revealed that surgical treatment did not show obvious advantages over non‐surgical treatment for complex fractures of the proximal humerus32.
Results of the Original Randomized Clinical Trials
One RCT33 involving 50 patients demonstrated that the non‐surgical treatment is accordant with the shoulder replacement for the displaced four‐part fractures in Constant–Murley and SST scores at 3‐month and 12‐month follow‐up, but the nonoperatively treated patients will feel more pain at 3‐month follow‐up. A similar result was achieved in another RCT where no evidence of a difference was presented between surgical and non‐surgical treatment in functional outcome at 1‐year follow‐up of displaced proximal humeral fractures in elderly patients34. Olerud et al. performed one RCT involving 55 patients, demonstrating a significant advantage in quality of life in favor of hemiarthroplasty, as compared to non‐surgical treatment in elderly patients with a displaced 4‐part fracture of the proximal humerus, and the main advantage of hemiarthroplasty appeared to be less pain while there were no differences in range of motion (ROM).
Results on the Meta‐Analysis Including Randomized Clinical Trials
As is well‐known, meta‐analyses including RCT or quasi‐RCT, which provide the highest level of evidence, are conducive to making more reasonable clinical decisions for clinicians, patients, and decision‐makers; however, numerous meta‐analyses published focusing on common topics have been conducted to estimate intervention methods, but the conclusions are discrepant. Such inconsistent findings puzzle decision‐makers in the clinic, who make clinical choices among alternative interventions based on best available evidence. Fortunately, multiple authors had performed numerous systematic reviews or meta‐analyses to evaluate the effectiveness and safety of surgical and non‐surgical treatment for displaced proximal humeral fractures. A network meta‐analysis including 7 RCT suggested that reverse shoulder arthroplasty was a beneficial choice for the treatment of the displaced 3‐part or 4‐part fractures with more favorable clinical outcomes and reduction of reoperation rates21. Two meta‐analyses demonstrated that compared to nonsurgical treatment, surgery did not improve the constant score. In this investigation, all included meta‐analyses demonstrated that surgical and non‐surgical interventions can improve the preoperative clinical status, but the relative effects between these two interventions are still discordant16, 20. These meta‐analyses comprehensively performed literature searches of similar procedures, but the included original articles and their conclusions were presented differently, and did not provide similar conclusions for treating displaced 3‐part and 4‐part fractures of the proximal humerus.
Every Variable of Interest after the Jadad Decision Algorithm
A guide to interpreting discordant systematic reviews by Jadad et al. was designed to make a decision algorithm in the clinic to choose the highest level of evidence from currently discordant systematic reviews or meta‐analyses31. We analyzed the possible sources of inconsistency among the included meta‐analyses by assessing the clinical topic, study selection and inclusion, data extraction, study quality, heterogeneity of combined studies, publication bias, sensitivity, and data synthesis. According to the search strategies, the process of screening and application of selection with the Jadad algorithm, 1 meta‐analysis with 6 RCT was selected in this systematic review of overlapping meta‐analyses19. The current study demonstrated that surgical treatment is superior to conservative treatment with respect to EQ‐5D; however, the Constant score, DASH, ASES score, SST, ROM, 15D, and total complications (avascular necrosis, bone resorption, infections, mortality, and non‐union in the surgical group) did not yield a clinically important difference. There was no difference between surgical and conservative interventions with respect to these variables. Finally, complication rates are of great importance. Infection is a common complication after surgical treatment. No difference between the two methods existed with respect to other complications in the two selected meta‐analyses; however, the difference did not have statistical significance, and, thus, warrants further investigation. For fractures that do not achieve satisfactory function, reduction, or prognosis with non‐operative treatment, surgery is necessary. Therefore, although our study demonstrated that surgical treatment was consistent with non‐surgical treatment in many aspects, the indications and complications of each technique may have differences. The optimum treatment strategy should be determined by the characteristics of fractures (age, open or closed, non‐displaced, or displaced) and the experience of the surgeons.
The Analyzing Advantages of Overlapping Meta‐Analyses
There are some particular advantages relating to the analysis in this systematic review of overlapping meta‐analyses: (i) the optimal search strategies and the retrieval process of screening on published data were used to obtain more reliable results and minimize the possibility of publication bias;(ii) each meta‐analysis has good homogeneity and steady data; (iii) three methods, the Jadad Decision Algorithm, the Oxford Levels of Evidence, and AMSTAR, were used to maintain the quality; and (iv) each included meta‐analysis was evaluated using the whole retrieval progress, every included original study, and statistical methods.
Some limitations in this investigation merit consideration. First, this was a systematic review of published overlapping meta‐analyses, and we could only analyze issues on the meta‐analysis level, instead of the patient or trial level. Second, although we included the meta‐analyses exclusively pooling RCT to ensure the quality of our investigation, several meta‐analyses included and analyzed lower‐quality RCT. Third, to acquire the highest level of evidence, only meta‐analyses comprising RCT were included in this study.
Conclusion
This systematic review of overlapping meta‐analyses reveals that although surgical treatment is more advantageous and superior to non‐surgical treatment for displaced 3‐part and 4‐part fractures of the proximal humerus, the former leads to higher incidence of postoperative complications.
Acknowledgments
This study was supported by the China Scholarship Council (CSC), which funded the author (Fanxiao Liu, No. 201808080126) and the Shandong Key R&D Program, which funded the author (Baisheng Fu, No. 2017GSF18112).
Disclosure: The authors declare that they have no competing interests.
References
- 1. Baron JA, Karagas M, Barrett J, et al Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology, 1996, 7: 612–618. [DOI] [PubMed] [Google Scholar]
- 2. Court‐Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury, 2006, 37: 691–697. [DOI] [PubMed] [Google Scholar]
- 3. Horak J, Nilsson BE. Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat Res, 1975, 112: 250‐253. [PubMed] [Google Scholar]
- 4. Iyengar JJ, Devcic Z, Sproul RC, Feeley BT. Nonoperative treatment of proximal humerus fractures: a systematic review. J Orthop Trauma, 2011, 25: 612–617. [DOI] [PubMed] [Google Scholar]
- 5. Lanting B, MacDermid J, Drosdowech D, Faber KJ. Proximal humeral fractures: a systematic review of treatment modalities. J Shoulder Elbow Surg, 2008, 17: 42–54. [DOI] [PubMed] [Google Scholar]
- 6. Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M, Vuori I. Increasing number and incidence of osteoporotic fractures of the proximal humerus in elderly people. BMJ, 1996, 313: 1051–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M, Vuori I. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970‐1998 and alarming projections for the new millennium. Acta Orthop Scand, 2000, 71: 465–470. [DOI] [PubMed] [Google Scholar]
- 8. Roux A, Decroocq L, EI Batti S, et al Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res, 2012, 98: 715–719. [DOI] [PubMed] [Google Scholar]
- 9. Court‐Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand, 2001, 72: 365–371. [DOI] [PubMed] [Google Scholar]
- 10. Agudelo J, Schurmann M, Stahel P, et al Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma, 2007, 21: 676–681. [DOI] [PubMed] [Google Scholar]
- 11. Bell JE, Leung BC, Spratt KF, Koval KJ, et al Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am, 2011, 93: 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Handoll HH, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev, 2012, 12: CD000434. [DOI] [PubMed] [Google Scholar]
- 13. Fu T, Xia C, Li Z, Wu H. Surgical versus conservative treatment for displaced proximal humeral fractures in elderly patients: a meta‐analysis. Int J Clin Exp Med, 2014, 7: 4607–4615. [PMC free article] [PubMed] [Google Scholar]
- 14. Jia Z, Li W, Qin Y, et al Operative versus nonoperative treatment for complex proximal humeral fractures: a meta‐analysis of randomized controlled trials. Orthopedics, 2014, 37: e543–e551. [DOI] [PubMed] [Google Scholar]
- 15. Sun Y, Li L, Dai J, Wang T. Treatment of complex proximal humeral fracture: plate and tension band fixation versus conservative therapy. Int J Clin Exp Med, 2015, 8: 7143–7151. [PMC free article] [PubMed] [Google Scholar]
- 16. Li Y, Zhao L, Zhu L, Li J, Chen A. Internal fixation versus nonoperative treatment for displaced 3‐part or 4‐part proximal humeral fractures in elderly patients: a meta‐analysis of randomized controlled trials. PloS One, 2013, 8: e75464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mao Z, Zhang L, Zhang L, et al Operative versus nonoperative treatment in complex proximal humeral fractures. Orthopedics, 2014, 37: e410–e419. [DOI] [PubMed] [Google Scholar]
- 18. Mao F, Zhang DH, Peng XC, Liao Y. Comparison of surgical versus non‐surgical treatment of displaced 3‐ and 4‐part fractures of the proximal humerus: a meta‐analysis. J Invest Surg, 2015, 28: 215–224. [DOI] [PubMed] [Google Scholar]
- 19. Rabi S, Evaniew N, Sprague SA, Bhandari M, Slobogean GP. Operative vs non‐operative management of displaced proximal humeral fractures in the elderly: a systematic review and meta‐analysis of randomized controlled trials. World J Orthop, 2015, 6: 838–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li W, Ding G, Liu J, Shi J, Zhang C, Gao Q. [Operative versus non‐operative treatment for three‐ or four‐part proximal humeral fractures in elderly patients: a meta‐analysis of randomized controlled trials]. Zhejiang Da Xue Xue Bao Yi Xue Ban, 2016, 45: 641–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Du S, Ye J, Chen H, Li X, Lin Q. Interventions for treating 3‐ or 4‐part proximal humeral fractures in elderly patient: a network meta‐analysis of randomized controlled trials. Int J Surg, 2017, 48: 240–246. [DOI] [PubMed] [Google Scholar]
- 22. Zhang Q, Liu F, Xiao Z, et al Internal versus external fixation for the treatment of distal radial fractures: a systematic review of overlapping meta‐analyses. Medicine (Baltimore), 2016, 95: e2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tan G, Li F, Zhou D, Cai X, Huang Y, Liu F. Unilateral versus bilateral percutaneous balloon kyphoplasty for osteoporotic vertebral compression fractures: a systematic review of overlapping meta‐analyses. Medicine (Baltimore), 2018, 97: e11968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Panic N, Leoncini E, de Belvis G, Ricciardi W, Boccia S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta‐analysis (PRISMA) statement on the quality of published systematic review and meta‐analyses. PloS One, 2013, 8: e83138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shea BJ, Hamel C, Wells GA, et al AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol, 2009, 62: 1013–1020. [DOI] [PubMed] [Google Scholar]
- 26. Shea BJ, Grimshaw JM, Wells GA, et al Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol, 2007, 7: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shea BJ, Bouter LM, Peterson J, et al External validation of a measurement tool to assess systematic reviews (AMSTAR). PloS One, 2007, 2: e1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Slobogean G, Bhandari M. Introducing levels of evidence to the Journal of Orthopaedic Trauma: implementation and future directions. J Orthop Trauma, 2012, 26: 127–128. [DOI] [PubMed] [Google Scholar]
- 29. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am, 2003, 85: 1–3. [PubMed] [Google Scholar]
- 30. Higgins JP, Green S. Cochrane handbook for systematic reviews of Interventions 2011. Available from: https://handbook-5-1.cochrane.org (accessed 15 April 2019).
- 31. Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ, 1997, 156: 1411–1416. [PMC free article] [PubMed] [Google Scholar]
- 32. Tamimi I, Montesa G, Collado F, et al Displaced proximal humeral fractures: when is surgery necessary?. Injury, 2015, 46: 1921–1929. [DOI] [PubMed] [Google Scholar]
- 33. Boons HW, Goosen JH, van Grinsven S, van Susante JL, van Loon CJ. Hemiarthroplasty for humeral four‐part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop Relat Res, 2012, 470: 3483–3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma, 2012, 26: 98–106. [DOI] [PubMed] [Google Scholar]


