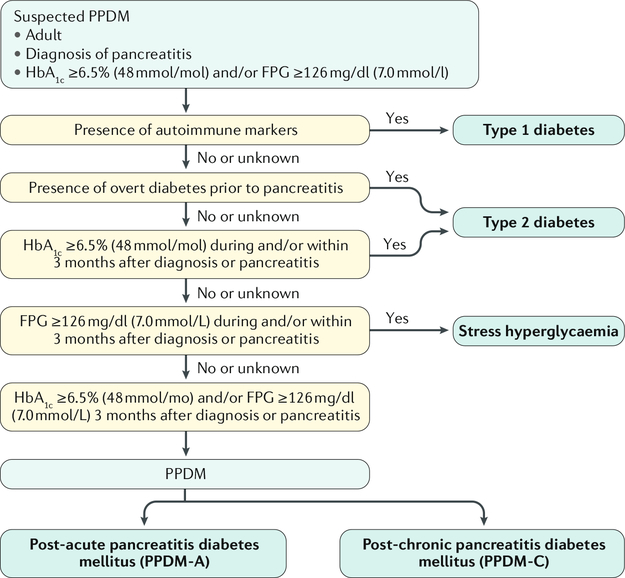
Fig. 3 |. Diagnostic algorithm to identify individuals with PPDM.
Post-pancreatitis diabetes mellitus (PPDM) should be suspected in all adults with a history of pancreatitis who meet the diagnostic criteria for diabetes by the American Diabetes Association. Confirmed type 1 diabetes, or type 2 diabetes prior to first attack of pancreatitis, or stress hyperglycaemia during (or within 3 months after) pancreatitis rules out the diagnosis of PPDM. The 3-month threshold is applied because glycated haemoglobin (HbAlc) level reflects average plasma glucose over the previous 8–12 weeks. The term ‘New-onset diabetes after pancreatitis’ (NODAP) is reserved for individuals with PPDM who had documented normal glucose homeostasis at baseline (as evidenced by available HbAlc and/or fasting plasma glucose (FPG) data). The algorithm has been devised by the authors. The glycated haemoglobin HbAlc test should be performed using a method that is certified by the National Glycohaemoglobin Standardization Program (NGSP) and standardized or traceable to the Diabetes Control and Complications Trial (DCCT) reference assay. Fasting is defined as no caloric intake for at least 8 h. Autoimmune markers include islet cell autoantibodies and autoantibodies to glutamic acid decarboxylase, insulin, the tyrosine phosphatases IA-2 and IA-2b and zinc transporter antigen. The oral glucose tolerance test can also be used to diagnose diabetes, if it is deemed practical and time-efficient in a given hospital.