Abstract
We describe a 10 year old boy who presented with acute onset rapidly progressing encephalopathy. MRI revealed bilateral insular cortex and basifrontal involvement suggesting Herpes encephalitis.He was treated with acyclovir and his symptoms improved. Six months after the first hospitalization he reported back with two episodes of partial seizures. He was started on Valproate. A week after starting valproate he was readmitted with hyperammonemic encephalpathy, on further investigations Citrullinemia Type 1 was diagnosed. This case highlights a metabolic disorder which radiologically mimics herpes encephalitis. The management of the disorder differs remarkably from herpes encephalitis and hence its recognition and suspicion based on radiology is critical.
KEYWORDS: Citrullinemia, herpes encephalitis, hyperammonemia
CASE REPORT
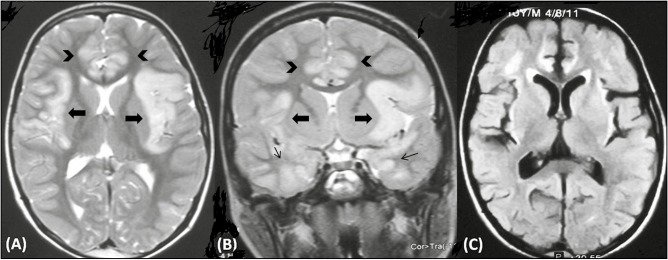
A 10-year-old boy was first admitted with a history of acute-onset, rapidly progressive, altered consciousness of 2-day duration. He had become totally unresponsive by the time of hospitalization. There was no history of fever, rash, trauma, or seizures. On examination, there were no focal deficits. His cerebrospinal fluid (CSF) examination was unremarkable. On the basis of the MRI of the brain [Figure 1A and B], a diagnosis of herpes encephalitis was suspected and treatment with acyclovir initiated. Though his herpes simplex virus (HSV) polymerase chain reaction (PCR) in CSF was negative, he was given a 2-week course of intravenous acyclovir. He made a gradual recovery of consciousness in hospital and was interactive at the time of discharge. However, he continued to have behavioral problems after discharge. He was noticed by parents and teachers to have become stubborn, hyperactive, inattentive, and aggressive. His school performance too was poor compared to the premorbid level. Six months after the first hospitalization, he reported back with two episodes of partial seizures. Valproate was initiated at a dose of 10mg/kg. One week later, he presented with acute-onset rapidly progressive altered consciousness with abnormal behavior and hallucinations. There was no history of fever or seizures. CSF was unremarkable and negative for HSV by PCR. MRI revealed residual changes and no new areas of involvement [Figure 1C]. Blood ammonia was 260 mmol/L (normal < 35), and urine gas chromatography and mass spectrometry revealed elevated orotic acid. Blood spot tandem mass spectrometry, plasma, and urine amino acid analysis revealed a markedly elevated citrulline level. Genetic analysis revealed a homozygous missense variation in exon 11 of the ASS1 gene (chr9:133355791; C > T). His initial diagnosis of herpes encephalitis [Figure 1] was revised to late-onset citrullinemia type I. There was a gradual improvement in consciousness and behavior with sodium benzoate, arginine, and protein restriction. At 45-month follow-up, he was attending school, had no significant behavioral problems, and had normal ammonia levels.
Figure 1.
Axial (A) and coronal (B) T2-weighted MRI showing swollen, hyperintense, insular cortices (thick black arrows), cingulate gyri (black arrowheads), and basal temporal cortices (thin black arrows). Follow-up axial fluid-attenuated inversion recovery MRI at 6 months showing resolution of old changes with residual mild cortical atrophy, ex vacuo ventricular dilatation, and curvilinear hyperintense signal changes in subcortical white matter of insular and frontal cortex (C)
DISCUSSION
Citrullinemia type I (MIM # 215700) is a rare, autosomal recessive, urea cycle disorder caused by deficiency of argininosuccinate synthase. The late-onset citrullinemia is usually less severe and has varied clinical presentations. Children may present with growth failure, poor appetite, behavioral abnormalities, poor coordination, sleep disorders, cyclical vomiting, ataxia, stroke-like episodes, and acute encephalopathy precipitated by infections, catabolic states, and medications.[1] In the child we report, the first episode of encephalopathy was unprovoked but the second was provoked by valproate.
MRI findings in citrullinemia are varied; common radiological findings are diffuse gray matter and white matter hyperintensities in cingulate, perirolandic, parietal, temporo-insular cortex with involvement of basal ganglia. The MRI findings being similar to herpes encephalitis resulted in a misdiagnosis in the child we report. It is postulated that elevated ammonia in urea cycle disorders gets converted to glutamine and the resultant osmotic effects are believed to cause astrocyte swelling and subsequent brain edema.[2] Similar to the areas involved in herpes encephalitis, it has been suggested that insular cortex, cingulate gyrus, and temporal lobes may be particularly vulnerable to hyperammonemic brain injury.[3] In addition, the curvilinear hyperintensities in subcortical white matter seen on follow-up of this child have also been suggested to be a clue to an underlying proximal urea cycle disorder.[4]
In conclusion, a consideration for inherited disorder of urea cycle should be kept in children with acute encephalopathy with normal CSF and imaging changes such as herpes encephalitis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Smith W, Kishnani PS, Lee B, Singh RH, Rhead WJ, Sniderman King L, et al. Urea cycle disorders: Clinical presentation outside the newborn period. Crit Care Clin. 2005;21:S9–17. doi: 10.1016/j.ccc.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Butterworth RF. Pathophysiology of brain dysfunction in hyperammonemic syndromes: The many faces of glutamine. Mol Genet Metab. 2014;113:113–7. doi: 10.1016/j.ymgme.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Baganz MD, Dross PE. Valproic acid-induced hyperammonemic encephalopathy: MR appearance. AJNR Am J Neuroradiol. 1994;15:1779–81. [PMC free article] [PubMed] [Google Scholar]
- 4.Nunley S, Ghosh D. Teaching neuroimages: MRI findings in carbamoyl phosphate synthetase 1 deficiency. Neurology. 2015;84:e138–9. doi: 10.1212/WNL.0000000000001546. [DOI] [PubMed] [Google Scholar]