Abstract
Background
Treadmill training augmented with visual images projected on the belt's surface can help improve walking adaptability. Moreover, patient-tailored automatization and standardization can increase the feasibility of walking-adaptability therapy. We developed C-Gait, a treadmill protocol consisting of a baseline walking-adaptability assessment involving 7 putatively distinct walking-adaptability tasks and a decision algorithm, to automatically update training content and execution parameters to a patients’ performance and perceived challenge.
Objectives
The main objective was to examine the feasibility, acceptability, and clinical potential of C-Gait training. The secondary objective was to evaluate the validity of the baseline assessment.
Design
This was a longitudinal proof-of-concept study with pretraining, posttraining, and retention tests encompassing baseline assessment and walking-related clinical measures.
Methods
Twenty-four healthy adults, 12 healthy older persons, and 28 patients with gait and/or balance deficits performed the baseline assessment; the gait deficit group received 10 C-Gait training sessions over a 5-week period. Baseline assessment scores and walking-related clinical measures served as outcome measures.
Results
C-Gait training exhibited significant progression in training content and execution, with considerable between-patient variation and minimal overruling by therapists. C-Gait training was well accepted and led to improvements in walking adaptability and general walking ability, which persisted after training cessation. Baseline assessment scores differed over groups and difficulty levels, had no-to-moderate correlations with walking-related clinical measures, and had limited correlations among walking-adaptability tasks.
Limitations
C-Gait was evaluated in a small yet diverse cohort. More encompassing studies are required to further establish its apparent merits. The validity of treadmill-based walking-adaptability assessment against an overground standard remains to be established.
Conclusions
C-Gait offers automatized, standardized, and patient-tailored walking-adaptability training that is feasible and well accepted, with good potential for improving task-specific and generic measures of walking.
Older persons can suffer from walking problems, which can increase their fall risk. To promote safe community ambulation and to prevent falls, the ability to adapt walking to environmental challenges and hazards might have to be taught through training.1–5 Recently, novel training devices and interventions have been developed for this purpose, among which is C-Mill training. The C-Mill (Motek, Amsterdam/Culemborg, the Netherlands) is an instrumented treadmill that can project visual images (or objects) on its walking surface. When walking on the treadmill, the patient can be instructed to hit (goal-directed stepping) or avoid (obstacle avoidance) projected visual objects. In this manner, both repetitive stepping and walking adaptability can be practiced using the C-Mill, which has led to the development of novel training paradigms.6–12 Furthermore, the C-Mill is equipped with a large embedded force platform to quantify center-of-pressure movements, which can be used for real-time performance feedback to the patient, as well as for adapting walking speed and the presentation of visual objects to the patient's performance.13–15 C-Mill training allows therapists to flexibly attune the training to the specific abilities and needs of individuals. Specifically, therapists can modify training content (ie, type and duration of particular walking-adaptability tasks) and execution parameters (ie, belt speed, difficulty level, handrail use) to prevent demotivation during training, as might be induced by offering training content that is either too challenging or too easy, according to the motivational flow model.16 However, at present, no objective guidelines exist regarding the design of treadmill-based gait training programs or how to adapt them to individual needs and treatment goals. These aspects are currently left to the therapist supervising the training, who must be well versed in operating the C-Mill. This requirement can limit the practical potential of C-Mill training, combined with the fact that operating the C-Mill can divert the therapist's attention from monitoring, instructing, and assisting the patient.
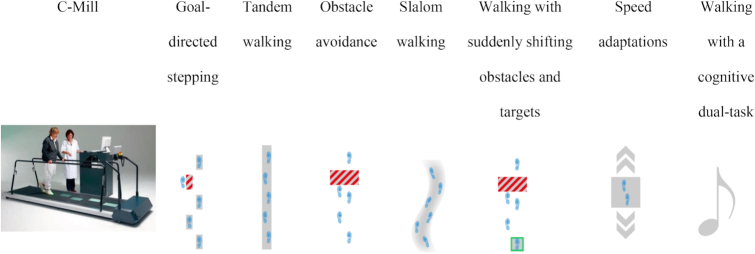
To address these problems, we developed an automatized and standardized patient-tailored C-Mill training protocol, called “C-Gait.” C-Gait consists of: (1) a standardized assessment of the baseline performance on 7 supposedly distinct walking-adaptability tasks (ie, goal-directed stepping, tandem walking, obstacle avoidance, slalom walking, adaptation to suddenly shifting obstacles and targets, adaptation to speed changes, and dual-task walking), addressing some of the previously defined walking-adaptability domains;17 and (2) a training protocol based on a decision algorithm that determines training content and execution parameters for each training session according to the patient's performance and perceived challenge during the preceding session. Although this training protocol is automatically generated and tailored to individual competencies, it can be overruled if deemed necessary by the therapist.
The main objective of the present proof-of-concept study was to examine the feasibility, acceptability, and clinical potential of C-Gait training in patients with gait and/or balance deficits. Feasibility was evaluated in terms of progress and between-patient variation in training content and execution parameters, patients’ performance and perceived challenge, and the degree of overruling by therapists. We expected the automated training protocol to be progressive in terms of belt speed, difficulty level, and handrail use, with considerable between-patient variation in training content and execution parameters, but an overall high (but not perfect) performance and moderately perceived challenge, and minimal overruling by therapists, indicating feasible individual therapy that is neither too easy nor too challenging.16 Acceptability of C-Gait training was assessed after completing the C-Gait training protocol with a questionnaire. Finally, the clinical potential of C-Gait training was evaluated by comparing baseline assessment scores and walking-related clinical measures between pretraining, posttraining, and retention tests.
A secondary objective was to evaluate the face validity of the baseline assessment by comparing C-Gait outcome measures (belt speed and composite score representing participants’ performance over standardized difficulty levels) across groups varying in walking ability (healthy adults, healthy older persons, and patients with gait and/or balance deficits) as well as overall task performance between 2 difficulty levels. If the baseline assessment taps into walking adaptability, then its outcome measures are expected to differ among participant groups as a function of expected walking adaptability and varying difficulty levels. Item validity was evaluated by correlating performance across the 7 walking-adaptability tasks encompassing the baseline assessment; these should be limited if the tasks in question represent separate aspects of walking adaptability. Finally, we correlated the aforementioned composite score with walking-related clinical measures of patients with gait and/or balance deficits. Considering the strong focus on walking adaptability rather than general walking ability, we expected no or only moderate correlations between the baseline composite score and walking-related clinical measures.
Methods
Participants
Twenty-four healthy adults (HA), 12 healthy older persons without gait and/or balance deficits (HE), and 28 patients with gait and/or balance deficits (GD) were included, all of whom had no previous experience with the C-Mill. The GD group was recruited from 2 physical therapist practices (Amstelland in Amstelveen and Boot & Broersen in Lisse, the Netherlands) and 1 rehabilitation center (Revant Lindenhof in Goes, the Netherlands). Inclusion criteria for the GD group were: (1) age at least 65 years and Short Physical Performance Battery (SPPB) score not exceeding 9 points or first-ever stroke at least 3 months ago; (2) a Functional Ambulation Categories (FAC) score of at least 3 points; and (3) a high risk of falling based on fear of falling and/or falling history as indicated by the physical therapist. Exclusion criteria were interfering treatments that could influence the effects of C-Gait training. All participants had to be able to understand and execute simple instructions and have no contraindication to physical training or severe uncorrected visual deficits. Eligible participants were informed about the study, both verbally and in writing, and provided informed consent. The study protocol was approved by the Medical Ethical Reviewing Committee of VU University Medical Centre (Amsterdam, the Netherlands; protocol number 2015/057).
Study Design
All three groups (HA, HE, GD) performed the C-Gait baseline assessment to evaluate its face validity in terms of between-group differences, and for the GD group walking-related clinical measures were also assessed to determine their relation with the C-Gait assessment. After these pretraining tests (T1), the GD group received 5 weeks of C-Gait training. Posttraining tests (T2, within 1 week after the last training) and retention tests (T3, 6 weeks after the last training) included reassessment of the C-Gait baseline assessment and walking-related clinical measures. All measurements and training sessions were part of a regular physical therapy treatment regimen. All involved therapists were trained in using the C-Gait protocol.
C-Gait Baseline Assessment
A 20-minute C-Gait baseline assessment of walking adaptability was performed using the 7 different tasks mentioned above and depicted in Figure 1 and the Video (available at https://academic.oup.com/ptj).17 All but the cognitive dual-task, which consisted of an auditory Stroop task, were assessed at a lower and higher level of difficulty (eAppendix 1, available at https://academic.oup.com/ptj) to determine participants’ first C-Gait training in terms of content and execution parameters. C-Gait baseline assessment was performed at a comfortable walking speed, which was determined for each participant by slowly increasing the belt speed in steps of 0.1 km/h until the participant reported it as comfortable. Subsequently, belt speed was increased by 0.5 km/h followed by a stepwise decrease (0.1 km/h) until the participant reported it as comfortable again. These 2 indications of comfortable walking speed were then averaged and taken to represent the participant's comfortable belt speed.
Figure 1.
The C-Mill and the 7 C-Gait walking-adaptability tasks.
C-Gait Training
C-Gait training follows a decision algorithm–based training protocol based on expert advice and literature (eAppendix 1, available at https://academic.oup.com/ptj). Training content and execution parameters of the first training session were automatically generated based on performance during the baseline assessment. Each subsequent training session was automatically generated according to the performance and perceived challenge of the previous training. Training content is an adjustable parameter automatically modified from session to session based on the patient's performance; the poorer the task performance, the longer will be the relative training duration of that particular task in the next training session. Adjustable training execution parameters in the current proof-of-concept study were the difficulty level of walking-adaptability tasks and belt speed, which were automatically increased in odd and even training sessions, respectively, depending on the participant's performance in the preceding training session. Stepwise increments in difficulty level and belt speed were kept relatively small (ie, 1 level and 10%, respectively), ensuring that the training remained safe and tolerable. The third adjustable execution parameter was handrail use (0 to 1 to 2 hands; never, rarely, sometimes, often, or always, as documented for each walking-adaptability task for each training session); participants were automatically advised to reduce handrail use when belt speed or difficulty level was increased. When the highest level for a task was reached, participants were additionally challenged to reduce handrail use, to perform the task at an even higher walking speed (+10%), and/or to perform the auditory Stroop task concurrently. After completing a particular task during the training, participants were asked to rate how challenging the task was: “hard” (1 point), “neutral” (2 points), or “easy” (3 points). When the answer deviated from the actual performance for 3 consecutive training sessions, the protocol was adjusted accordingly. eAppendix 1 (available at https://academic.oup.com/ptj) details the performance cutoff of each task used to adjust training content and execution parameters, along with other decision algorithm elements.
C-Gait training was provided twice a week, and every training session lasted about 30 minutes, of which ∼20 minutes were spent on actual treadmill walking. All assessment and training sessions were supervised by a trained physical therapist. At the start of each training session, the automatically generated training protocol was provided as advice to the therapist, who could overrule the training protocol by manually adjusting the proposed training content and training execution parameters per task when deemed appropriate or necessary; the degree of overruling by physical therapists was recorded.
Outcome Measures
Outcome measures of the C-Gait baseline assessment comprised its belt speed and the composite score, performance per walking-adaptability task, and overall performance averaged over the 7 walking-adaptability tasks, as detailed here. Task performance of slalom walking, tandem walking, speed adaptations, goal-directed stepping, obstacle avoidance, and walking with suddenly shifting obstacles and targets was defined as the percentage of correctly performed steps relative to the projected visual objects (based on center-of-pressure at mid-stance; eAppendix 1, available at https://academic.oup.com/ptj). Cognitive dual-task performance during walking was quantified as the percentage of correct answers. The composite score of the baseline assessment was an average score based on average performance over the 6 walking-adaptability tasks at the higher level of difficulty and the performance of the cognitive dual-task, thereby combining different aspects of walking adaptability. The composite score of the baseline assessment ranged from 0 (poor performance) to 8 (excellent performance), as detailed in eAppendix 1 (available at https://academic.oup.com/ptj).
Walking-related clinical measures included the 10-Meter Walking Test (10MWT), Timed “Up & Go” Test (TUG), Activities-specific Balance Confidence Scale (ABC), and the SPPB. The 10MWT and TUG were performed 3 times at comfortable walking speed; subsequently, the average times to perform the whole 10MWT and TUG, respectively, were calculated.18,19 The ABC was assessed to determine balance confidence and had a possible range from 0% to 100%.20,21 The SPPB involved standing balance, timed 4-m walk, and 5 sit-to-stands, with the sum of the 3 components comprising the SPPB score (0–12 points).22
Statistical Evaluation of the Validity of the Baseline Assessment
The face validity of the baseline assessment was evaluated by: (1) comparing the belt speed and composite score between groups (HA, HE, and GD) using 1-way analyses of variance (ANOVAs), and (2) comparing overall performance (excluding the cognitive dual-task) between difficulty levels using a group (HA, HE, GD) by level (lower and higher difficulty level) repeated-measures ANOVA. Post hoc analyses of main effects and interactions used independent t tests (group effects) and paired-samples t tests (level effects). Degrees of freedom were adjusted if the assumption of sphericity (following the Mauchly test, using the Greenhouse-Geisser correction) or the assumption of equal variances (following the Levene test) were violated. The item validity was evaluated by correlating the performances on the walking-adaptability tasks at the higher difficulty level with each other, using nonparametric Spearman correlation coefficients (rs) and Cronbach  . C-Gait outcome measures were correlated with the walking-related clinical measures of the GD group using nonparametric Spearman correlation coefficients to determine their relation.
. C-Gait outcome measures were correlated with the walking-related clinical measures of the GD group using nonparametric Spearman correlation coefficients to determine their relation.
Examination of the Feasibility, Acceptability, and Clinical Potential of C-Gait Training
The feasibility of C-Gait training was assessed in terms of progress and between-participant variation in training content and execution parameters as well as in participants’ performance and perceived challenge and the degree of therapists’ overruling of the advised C-Gait training protocol. The progress in belt speed, difficulty level, perceived challenge (all averaged over the tasks), and overall performance was visualized over the 10 training sessions for all participants with 2 representative cases highlighted. These progressions were analyzed using repeated-measures ANOVAs with the within-subject factor “training” (10 levels) or with nonparametric Friedman ANOVAs followed by paired-samples t tests or Wilcoxon signed rank tests as post hoc tests. Between-participant variation in terms of content (relative duration) was illustrated by 2 representative cases, whereas for handrail use (number of hands used, averaged over the tasks) the percentage of participants using the handrails during the first and last training session was given and the difference between those training sessions was analyzed using a Wilcoxon signed rank test. The degree of overruling by therapists on the advised C-Gait training protocol was presented using the percentage disagreement between advised and performed training content and execution parameters.
The acceptability of C-Gait training was assessed in terms of participants’ experience after C-Gait training using a custom-made evaluation questionnaire with 1 to 10 rating scales and multiple-choice questions (eAppendix 2, available at https://academic.oup.com/ptj). The number of participants per score and the number of participants experiencing improvement(s) and/or discomfort(s) after training were reported.
The clinical potential of C-Gait training was evaluated by subjecting C-Gait outcome measures and walking-related clinical measures to repeated-measures ANOVAs with “time” as within-subject factor (3 levels: pretraining, posttraining, retention) and paired-samples t tests as post hoc tests. For all analyses the criterion P < .05 was adopted for significant effects. ANOVAs are presented as F, Wilcoxon signed rank tests are reported in Z, and ttests are reported in t. Effect sizes are presented as partial  for ANOVA or Cohen d for the other tests.
for ANOVA or Cohen d for the other tests.
Role of Funding Source
This study was funded by an “MKB-innovatie stimulering” grant of the Netherlands Enterprise Agency (RVO.nl). The funding source had no influence on the design of the study or the analysis or interpretation of the data.
Results
In total, 22 HA, 12 HE, and 28 GD participants completed the baseline assessment; 2 participants of the HA group were excluded because of incomplete data. Twenty-six GD participants completed the 5-week C-Gait protocol—taking at least 6 (n = 1), 7 (n = 1), 9 (n = 2), or 10 (n = 22) out of 10 training sessions—and posttraining tests; 2 GD participants (7%) dropped out after T1 due to interfering personal obligations and perceived stress with participation. Twenty-three of these participants completed the retention tests; 3 participants (12%) were unable to complete the retention tests due to illness or interfering personal obligations. Participants’ characteristics are provided in the Table.
Table.
Participant Characteristicsa
| Characteristic | HA (n = 22) | HE (n = 12) | GD (n = 28) |
|---|---|---|---|
| Menb, n (%) | 9 (41) | 8 (67) | 14 (50) |
| Age, y | 29.14 (11.69) | 70.25 (5.23) | 69.96 (11.40) |
| Height, m | 1.76 (0.08) | 1.76 (0.08) | 1.71 (0.08) |
| Body mass, kg | 71.55 (9.24) | 84.83 (14.26) | 76.83 (11.48) |
| Diagnosisc (stroke/elderly with gait and/or balance deficits), n | NA | NA | 6/22 |
| Time since diagnosis, mod | NA | NA | 12 (0–492) |
| FACd | NA | NA | 5 (4–5) |
| Walking aid indoorsb, n (%) | NA | NA | 4 (14) |
| Walking aid outdoorsb, n (%) | NA | NA | 10 (36) |
| Fear of fallingd | NA | NA | 5 (1–9) |
All values are reported as mean (SD) unless otherwise indicated. FAC = Functional Ambulation Categories; GD = patients with gait and/or balance deficits; HA = adults who were healthy; HE = older persons who were healthy; NA = not applicable.
Reported as number (percentage) of participants.
Reported as number of participants with stroke/number of elderly participants with gait and/or balance deficits.
Reported as median (minimum–maximum).
Validity of C-Gait Baseline Assessment
Between-group differences in C-Gait outcome measures (face validity)
As expected, the C-Gait belt speed and composite score varied significantly over groups (F2,59 = 6.10; P < .01;  = 0.17; and (F2,59 = 16.80; P < .01;
= 0.17; and (F2,59 = 16.80; P < .01;  = 0.36, respectively), with significantly lower belt speeds and composite scores for GD (0.68 ± 0.16 m/s and 6.64 ± 0.68, respectively) than the HA group (0.85 ± 0.14 m/s; t48 = 3.96; P < .01; d = 1.13; and 7.46 ± 0.18; t31.75 = 6.07; P < .01; d = 1.65, respectively). Moreover, the composite score was significantly higher for the HE (6.98 ± 0.33) than for the GD group (t37.30 = 2.11; P < .05; d = 1.83) but significantly lower than for the HA group (t32 = 5.51; P < .01; d = 1.83). No significant difference in belt speed was found between those groups (GD vs HE: 0.76 ± 0.24 m/s; t15.20 = 0.99; P = .34; d = 0.46; and HA vs HE: t15.29 = 1.26; P = .23; d = 0.46).
= 0.36, respectively), with significantly lower belt speeds and composite scores for GD (0.68 ± 0.16 m/s and 6.64 ± 0.68, respectively) than the HA group (0.85 ± 0.14 m/s; t48 = 3.96; P < .01; d = 1.13; and 7.46 ± 0.18; t31.75 = 6.07; P < .01; d = 1.65, respectively). Moreover, the composite score was significantly higher for the HE (6.98 ± 0.33) than for the GD group (t37.30 = 2.11; P < .05; d = 1.83) but significantly lower than for the HA group (t32 = 5.51; P < .01; d = 1.83). No significant difference in belt speed was found between those groups (GD vs HE: 0.76 ± 0.24 m/s; t15.20 = 0.99; P = .34; d = 0.46; and HA vs HE: t15.29 = 1.26; P = .23; d = 0.46).
Between-level and between-group differences in overall performance (face validity)
Overall performance varied significantly between the 2 difficulty levels (F1,59 = 49.46; P < .01;  = 0.46), with lower performance for the higher difficulty level (lower = 87.92 ± 8.04%; higher = 84.37 ± 7.68%). In line with the between-group differences for the composite scores, performance also varied significantly over groups (F2,59 = 13.50; P < .01;
= 0.46), with lower performance for the higher difficulty level (lower = 87.92 ± 8.04%; higher = 84.37 ± 7.68%). In line with the between-group differences for the composite scores, performance also varied significantly over groups (F2,59 = 13.50; P < .01;  = 0.31), with significantly lower performances for GD (86.15 ± 7.34%) and HE (89.72 ± 4.26%) groups than for the HA group (94.16 ± 1.86%) (t31.31) = 5.55; P < .01; d = 1.50; and t32 = 4.25; P < .01; d = 1.35, respectively). Overall performance did not differ between GD and HE groups (t38 = 1.57; P = .13; d = 0.59). There was no significant interaction between group and difficulty level (F2,59 = 0.87; P = .42;
= 0.31), with significantly lower performances for GD (86.15 ± 7.34%) and HE (89.72 ± 4.26%) groups than for the HA group (94.16 ± 1.86%) (t31.31) = 5.55; P < .01; d = 1.50; and t32 = 4.25; P < .01; d = 1.35, respectively). Overall performance did not differ between GD and HE groups (t38 = 1.57; P = .13; d = 0.59). There was no significant interaction between group and difficulty level (F2,59 = 0.87; P = .42;  = 0.03).
= 0.03).
Correlations among walking-adaptability tasks (item validity)
Performances of only 4 out of the 21 possible pairs of walking-adaptability tasks were significantly correlated: (1) goal-directed stepping and walking with suddenly shifting obstacles and targets (rs = 0.56; P < .01); (2) tandem walking and obstacle avoidance (rs = 0.46; P < .05); (3) speed adaptations and walking with a cognitive dual-task (rs = 0.43; P < .05); and (4) tandem walking and walking with suddenly shifting obstacles and targets (rs = 0.52; P < .01). This limited number of significant low to moderate correlations suggests that most of these tasks indeed capture distinctive aspects of walking adaptability; this suggestion is corroborated by an overall Cronbach α of 0.71, with removal of any task yielding lower  values.
values.
Correlation between C-Gait baseline assessment and walking-related clinical measures
Belt speed correlated significantly with 10MWT (rs = −0.72; P < .001), TUG (rs = −0.57; P < .01), and SPPB (rs = 0.50; P < .01) but not with the ABC (rs = 0.26; P = .20). The composite score, in contrast, only correlated significantly with TUG (rs = −0.48; P < .05) and not with other walking-related clinical measures (10MWT: rs = −0.29; P = .14; SPPB: rs = 0.10; P = .63; ABC: rs = 0.03; P = .88), suggesting that it addresses a distinctive construct that is not or only moderately targeted by standard clinical measures.
Feasibility of C-Gait Training
Training progress
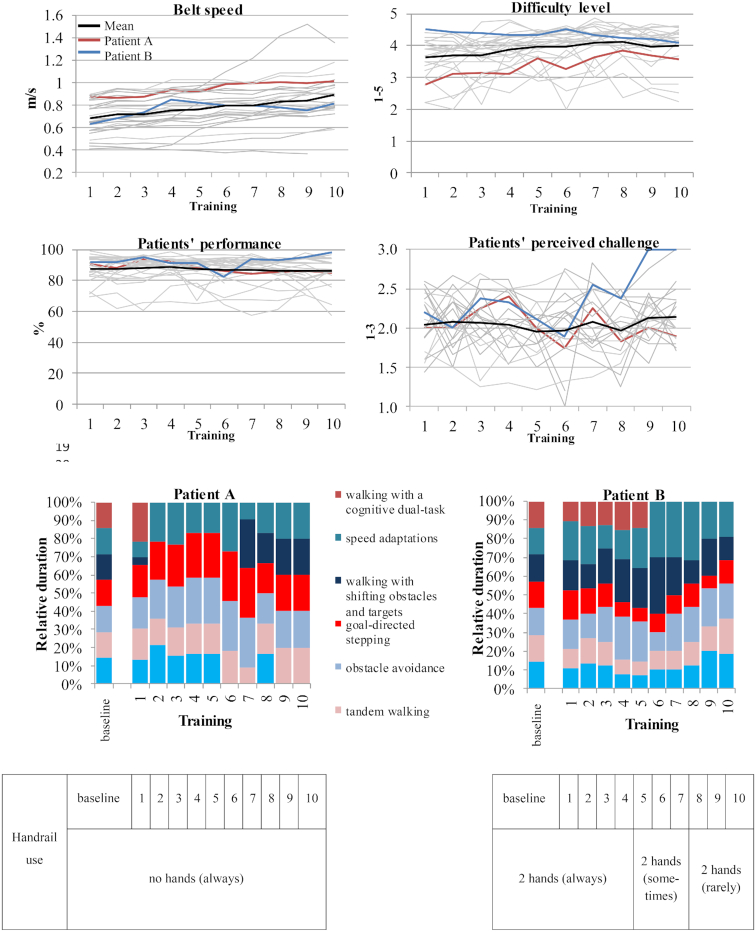
Figure 2 shows the progress in belt speed, difficulty level, participants’ performance, and perceived challenge over the 10 training sessions for all GD participants. Belt speed increased significantly over sessions (F1.53,32.12 = 21.35; P < .01;  = 0.50), with significant post hoc differences between all odd sessions and the consecutive even sessions (t21 > 2.08; P < .05; r > 0.41), consistent with the algorithm's speed adjustments in even sessions. The difficulty level also increased significantly over sessions (
= 0.50), with significant post hoc differences between all odd sessions and the consecutive even sessions (t21 > 2.08; P < .05; r > 0.41), consistent with the algorithm's speed adjustments in even sessions. The difficulty level also increased significantly over sessions ( 222 = 36.51; P < .01), with post hoc tests revealing significant or trend differences between consecutive sessions 1 and 2 (Z22 = 1.95; P = .051; r = 0.42), 3 and 4 (Z22 = 2.17; P < .05; r = 0.46), 4 and 5 (Z22 = 1.81; P = .071; r = 0.39), and sessions 8 and 9 (Z22 = 1.77; P = .076; r = 0.38). Participants’ performance and perceived challenge did not vary systematically over sessions (F4.52,94.81 = 1.21; P = .29;
222 = 36.51; P < .01), with post hoc tests revealing significant or trend differences between consecutive sessions 1 and 2 (Z22 = 1.95; P = .051; r = 0.42), 3 and 4 (Z22 = 2.17; P < .05; r = 0.46), 4 and 5 (Z22 = 1.81; P = .071; r = 0.39), and sessions 8 and 9 (Z22 = 1.77; P = .076; r = 0.38). Participants’ performance and perceived challenge did not vary systematically over sessions (F4.52,94.81 = 1.21; P = .29;  = 0.05;and
= 0.05;and  22 = 13.94; P = .13, respectively). Throughout all training sessions overall performance remained high (mean performance was 87.23%) and participants perceived training sessions as neutrally challenging (mean challenge was 2.05, neither too easy nor too difficult). Handrail use decreased from 61% (session 1) to 14% (session 10) of the participants using both hands for support, whereas the percentage of participants using no handrail increased from 11% (session 1) to 36% (session 10) (Z22 = 3.26; P < .01; r = 0.70).
22 = 13.94; P = .13, respectively). Throughout all training sessions overall performance remained high (mean performance was 87.23%) and participants perceived training sessions as neutrally challenging (mean challenge was 2.05, neither too easy nor too difficult). Handrail use decreased from 61% (session 1) to 14% (session 10) of the participants using both hands for support, whereas the percentage of participants using no handrail increased from 11% (session 1) to 36% (session 10) (Z22 = 3.26; P < .01; r = 0.70).
Figure 2.
Feasibility results: progress and between-patient variation in training content and execution parameters, performance, and perceived challenge over the 10 training sessions for the gait and/or balance deficits (GD) group (top 4 panels) and 2 representative cases (Participant A and Participant B) highlighted (lower 4 panels).
As is evident from Figure 2, between-participant variation in belt speed and difficulty level was large (ranging, respectively, from 0.37 to 1.52 m/s and from 2.0 to 4.9). We highlighted progression profiles in training execution parameters for 2 representative cases. Participant A started C-Gait training with a relatively high belt speed, relatively lower difficulty level but without handrail use. Over the sessions, both speed and difficulty levels increased. In contrast, participant B had a relatively low belt speed, high difficulty level, and used handrails with both hands. Over sessions, speed increased, difficulty level remained high, and handrail use was reduced. Finally, training content progressed differently for participants A and B, as visualized by the different changes in relative training duration of the 7 walking-adaptability tasks, which again underscores that the tasks address distinct walking-adaptability aspects. Together, these observations testify to the feasibility of the patient-tailored element of C-Gait training.
Therapists’ overruling
Overruling by therapists of the advised training in clinical practice was minimal: the automatically proposed difficulty level was adjusted in 4.10% of all occasions, belt speed was adjusted in 5.48%, and content was adjusted in 5.48%.
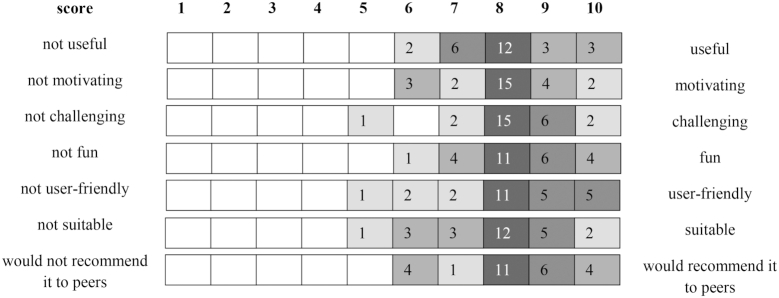
Acceptability of C-Gait Training
Participants scored C-Gait as useful, motivating, challenging, fun, user-friendly, and suitable and would recommend it to peers (Fig. 3). Participants described an increase in physical fitness (n = 19), safety of walking (n = 17), walking speed (n = 14), and confidence during walking indoors, outdoors on smooth surfaces, and outdoors on irregular surfaces and/or in crowded environments (n = 20). Participants reported only mild discomfort during and after training sessions, without exhibiting any serious adverse events related to the training. Discomfort during (once: n = 2; frequently: n = 5) and after (once: n = 2; frequently: n = 6) training sessions mainly comprised muscle soreness, fatigue, and shortness of breath.
Figure 3.
Acceptability results: patients’ experience (n = 26) after C-Gait training assessed with a custom-made questionnaire, presented as the number of patients (n) per score for 7 items.
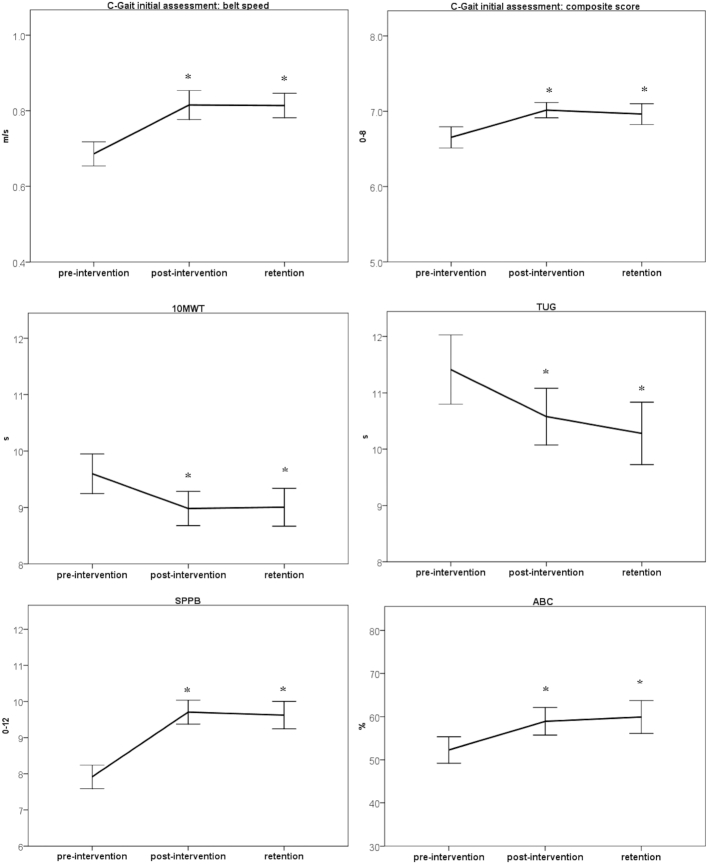
Clinical Potential of C-Gait Training
The C-Gait belt speed and composite score, 10MWT, TUG, and SPPB improved over time (all F1.53,33.75 > 5.22; P < .01;  > 0.19), with significant posttraining improvement (all T2 vs T1 t22 > 2.26; P < .05; r > 0.43; and all T3 vs T1 t22 > 2.22; P < .05; r > 0.43) and retention after 6 weeks (all T3 vs T2 t22 < 1.40; P > .18; r < 0.29). For the ABC we missed data for 1 participant; however, we saw similar results for this clinical measure, namely, a significant improvement over time (F2,42 = 6.98; P < .01;
> 0.19), with significant posttraining improvement (all T2 vs T1 t22 > 2.26; P < .05; r > 0.43; and all T3 vs T1 t22 > 2.22; P < .05; r > 0.43) and retention after 6 weeks (all T3 vs T2 t22 < 1.40; P > .18; r < 0.29). For the ABC we missed data for 1 participant; however, we saw similar results for this clinical measure, namely, a significant improvement over time (F2,42 = 6.98; P < .01;  = 0.25), with significant posttraining improvement (T2 vs T1 t21 = 3.52; P < .01; r = 0.61; and T3 vs T1 t21 = 2.96; P < .05; r = 0.54) and retention after 6 weeks (T3 vs T2 t21 = 0.47; P = .65; r = 0.10) (Fig. 4).
= 0.25), with significant posttraining improvement (T2 vs T1 t21 = 3.52; P < .01; r = 0.61; and T3 vs T1 t21 = 2.96; P < .05; r = 0.54) and retention after 6 weeks (T3 vs T2 t21 = 0.47; P = .65; r = 0.10) (Fig. 4).
Figure 4.
Clinical potential: effect of C-Gait training on C-Gait baseline assessment scores (belt speed and composite score) and walking-related clinical measures—10-Meter Walking Test (10MWT), Timed “Up & Go” Test (TUG), Activities-specific Balance Confidence Scale (ABC), and Short Physical Performance Battery (SPPB). Error bars represent the standard error, and asterisks represent significant differences (P < .05) compared with the pretraining tests.
Discussion
We developed C-Gait, a protocol for baseline assessment of walking adaptability and a decision algorithm, that adaptively and progressively updates training content and execution parameters to patients’ performance and experienced challenge. In this proof-of-concept study, we examined the feasibility, acceptability, and clinical potential of the C-Gait training protocol (main objective) and evaluated the validity of its baseline assessment (secondary objective). Face validity of the baseline assessment was evidenced by significant between-group (C-Gait outcome measures and overall performance) and between-level (overall task performance) differences in expected directions. Item validity was evidenced by limited correlations among the 7 walking-adaptability tasks, suggesting that they represented largely distinctive walking-adaptability aspects. Finally, no to moderate correlations between the composite score and walking-related clinical measures were found, suggesting added value. Considering that the baseline assessment focuses strongly on walking adaptability rather than walking ability in general, the added value most plausibly pertains to walking adaptability, although in the absence of a gold standard for (overground) walking adaptability17 this is difficult to prove.
Regarding our main objective, C-Gait training proved feasible, and exhibited significant progression and considerable between-participant variation in terms of training content and execution parameters, high overall task performance, and minimal overruling of the proposed training by therapists in clinical practice. Acceptance by therapists and confidence in a given therapy are prerequisites for automatized and standardized forms of therapy. Automatization enhanced the feasibility of C-Gait training by enabling therapists to supervise patients instead of operating technology; operational duties could be further reduced by recording handrail use with a force sensor.23 Standardization was successful in providing progressive (ie, significant changes in belt speed, difficulty level, and handrail use over training sessions) and participant-tailored (ie, large between-participant variation in training content and execution parameters) training, testifying to C-Gait's feasibility for patients who vary widely in terms of self-selected walking speed, handrail use, and walking adaptability. C-Gait training was well accepted by participants with gait and/or balance deficits. Participants rated the progressive training as moderately challenging while maintaining high but suboptimal levels of task performance, suggesting that the training was indeed challenging but not too easy or too difficult, which is important for motivational flow.16
Last but not least, C-Gait training has good clinical potential, as evidenced by significant task-specific (C-Gait outcome measures) and generic (walking-related clinical measures) improvements from pretraining to posttraining, which all persisted 6 weeks later (retention); observed gains in 10MWT and SPPB were substantially greater than their known clinically meaningful changes of 0.05 m/s and 1.0 point, respectively.24 Future studies are warranted to further establish the apparent merits of automatized, standardized, and patient-tailored progressive walking-adaptability training compared with conventional gait training or conventional C-Mill training.8,10 Such studies, with more participants, therapists, and care centers, now seem feasible owing to C-Gait's automatized and standardized assessment and training, which could help in determining which patients would benefit most from treadmill-based walking-adaptability training. This seems timely considering that conventional C-Mill walking-adaptability training showed clinical potential for groups with similar levels of walking ability as our GD group.6,9,25 However, based on the current evidence, C-Mill training does not seem more effective than other interventions in groups with greater walking ability (and cognitive) limitations,10 although 2 conventional C-Mill therapy trials are still running.11,12 The developed patient-tailored C-Gait walking-adaptability assessment and training protocol could facilitate identification of responders and nonresponders to walking-adaptability training by collecting and combining standardized baseline and training data suitable for database research. Validation of the treadmill-based baseline assessment of walking-adaptability aspects could be required against an overground standard, which now seems possible with the Interactive Walkway.26
Conclusion
C-Gait provides a feasible and well-accepted protocol for automatized, standardized, patient-tailored and progressive training, with good potential for improving both task-specific and generic measures of walking, paving the way for assessing and training large and diverse groups of patients with walking-adaptability limitations.
Supplementary Material
Author Contributions and Acknowledgments
Concept/idea/research design: C. Timmermans, M. Roerdink, T.W.J. Janssen, P.J. Beek, C.G.M. Meskers
Writing: C. Timmermans, M. Roerdink, T.W.J. Janssen, P.J. Beek, C.G.M. Meskers
Data collection: C. Timmermans
Data analysis: C. Timmermans, M. Roerdink
Project management: C. Timmermans, C.G.M. Meskers
Fund procurement: P.J. Beek, C.G.M. Meskers
Consultation (including review of manuscript before submitting): M. Roerdink
All collaborators within the “Mkb-innovatie stimulering” grant of the Netherlands Enterprise Agency (RVO.nl) are gratefully acknowledged. Jaap Versloot, Jasper de Beus, and Peter Martens of Motek, Amsterdam, contributed to the design and development of the C-Gait software for the C-Mill. The participating therapists of the involved physical therapist practices (Amstelland in Amstelveen, and Boot & Broersen in Lisse, the Netherlands) and rehabilitation centre (Revant Lindenhof in Goes, the Netherlands), in particular Guido van Werven and Jasper Sint, are acknowledged for their contribution to the measurements and training sessions.
Ethics Approval
The study protocol was approved by the Medical Ethical Reviewing Committee of VU University Medical Centre (Amsterdam, the Netherlands; protocol number 2015/057).
Funding
This study was funded by an “MKB-innovatie stimulering” grant of the Netherlands Enterprise Agency (RVO.nl).
Disclosures
The authors completed the ICJME Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. Berg WP, Alessio HM, Mills MM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26:261–268. [DOI] [PubMed] [Google Scholar]
- 2. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. [DOI] [PubMed] [Google Scholar]
- 3. Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age Ageing. 1981;10:141–146. [DOI] [PubMed] [Google Scholar]
- 4. Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990;19:136–141. [DOI] [PubMed] [Google Scholar]
- 5. Said CM, Goldie PA, Patla AE, Sparrow WA, Martin KE. Obstacle crossing in subjects with stroke. Arch Phys Med Rehabil. 1999;80:1054–1059. [DOI] [PubMed] [Google Scholar]
- 6. Heeren A, Van Ooijen MW, Geurts ACH et al.. Step by step: a pilot study on the effectiveness of gait adaptability training in the chronic phase after stroke using a treadmill with visual context. J Rehabil Med. 2013;45:616–622. [DOI] [PubMed] [Google Scholar]
- 7. Fonteyn EM, Heeren A, Engels JJ, Boer JJ, van de Warrenburg BP, Weerdesteyn V. Gait adaptability training improves obstacle avoidance and dynamic stability in patients with cerebellar degeneration. Gait Posture. 2014;40:247–251. [DOI] [PubMed] [Google Scholar]
- 8. Hollands KL, Pelton TA, Wimperis A et al.. Feasibility and preliminary efficacy of visual cue training to improve adaptability of walking after stroke: multi-centre, single-blind randomised control pilot trial. PLoS One. 2015;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Van Ooijen MW, Heeren A, Smulders K et al.. Improved gait adjustments after gait adaptability training are associated with reduced attentional demands in persons with stroke. Exp Brain Res. 2015;233:1007–1018. [DOI] [PubMed] [Google Scholar]
- 10. Van Ooijen MW, Roerdink M, Trekop M, Janssen TW, Beek PJ. The efficacy of treadmill training with and without projected visual context for improving walking ability and reducing fall incidence and fear of falling in older adults with fall-related hip fracture: a randomized controlled trial. BMC Geriatr. 2016;16:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Timmermans C, Roerdink M, Van Ooijen MW, Meskers CG, Janssen TWJ, Beek PJ. Walking adaptability therapy after stroke: study protocol for a randomized controlled trial. Trials. 2016;17:425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rossano C, Terrier P. Visually-guided gait training in paretic patients during the first rehabilitation phase: study protocol for a randomized controlled trial. Trials. 2016;17:523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roerdink M, Coolen BH, Lamoth CJ, Beek PL. Online gait event detection using a large force platform embedded in a treadmill. J Biomech. 2008;41:2628–2632. [DOI] [PubMed] [Google Scholar]
- 14. Roerdink M, Beek PJ. Device for displaying target indications for foot movements to persons with a walking disorder. US patent 2009246746-A1. October 1, 2009. European patent 2106779-A1. October 7, 2009. Japanese patent 2009240775-A. October 22, 2009. Dutch patent 1035236-C2. October 1, 2009.
- 15. Houdijk H, Van Ooijen MW, Kraal JJ et al.. Assessing gait adaptability in people with a unilateral amputation on an instrumented treadmill with a projected visual context. Phys Ther. 2012;92:1453–1460. [DOI] [PubMed] [Google Scholar]
- 16. Nakamura J, Csikszentmihalyi M. The concept of flow. In: Snyder C, Lopez SJ, eds. Oxford Handbook of Positive Psychology. Oxford University Press; 2009:89–105. [Google Scholar]
- 17. Balasubramanian CK, Clark DJ, Fox EJ. Walking adaptability after stroke and its assessment in clinical settings. Stroke Res Treatment. 2014;2014:591013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired: reliability and meaningfulness. Phys Ther. 1984;64:35–40. [DOI] [PubMed] [Google Scholar]
- 19. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med, 1995;332:556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Botner EM, Miller WC, Eng JJ. Measurement properties of the Activities-specific Balance Confidence Scale among individuals with stroke. Disabil Rehabil. 2005;27:56–163. [DOI] [PubMed] [Google Scholar]
- 21. Ylva N, Anette F. Psychometric properties of the Activities-Specific Balance Confidence Scale in persons 0-14 days and 3 months post stroke. Disabil Rehabil. 2012;34:1186–1191. [DOI] [PubMed] [Google Scholar]
- 22. Vasunilashorn S, Coppin AK, Patel KV et al.. Use of the short physical performance battery score to predict loss of ability to walk 400 meters: analyses from the InCHIANTI study. J Gerontol. 2009;2:223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. IJmker T, Lamoth CJ, Houdijk H et al.. Effects of handrail hold and light touch on energetics, step parameters, and neuromuscular activity during walking after stroke. J Neuroeng Rehabil. 2015;12:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749. [DOI] [PubMed] [Google Scholar]
- 25. Hollands KL, Pelton TA, van der Veen S, Alharbi S, Hollands MA. A novel and simple test of gait adaptability predicts gold standard measures of functional mobility in stroke survivors. Gait Posture. 2016;3:170–175. [DOI] [PubMed] [Google Scholar]
- 26. Geerse DJ, Coolen BH, Roerdink M. Kinematic validation of a Multi-Kinect v2 instrumented 10-meter walkway for quantitative gait assessments. PLoS One. 2015;13:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Van Ooijen-Kerste MW, Houdijk JHP, Janssen TWJ, Roerdink M. C-Mill training voor het oefenen van functionele loopvaardigheid. Nederlands Tijdschrift voor Revalidatiegeneeskunde. 2015;5:231–233. [Google Scholar]
- 28. Van Ooijen MW, Roerdink M, Trekop M, Visschedijk J, Janssen TWJ, Beek PJ. Functional gait rehabilitation in elderly people following a fall-related hip fracture using a treadmill with visual context: design of a randomized controlled trial. BMC Geriatr. 2013;13:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011;377:1693–1702. [DOI] [PubMed] [Google Scholar]
- 30. Beek PJ, Roerdink M. Evolving insights into motor learning and their implications for neurorehabilitation. In: Selzer M, Clarke S, Cohen L, Kwakkel G, Miller R, eds. Textbook of Neural Repair and Rehabilitation. Cambridge: Cambridge University Press; 2014:95–104. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.