Figure 1.
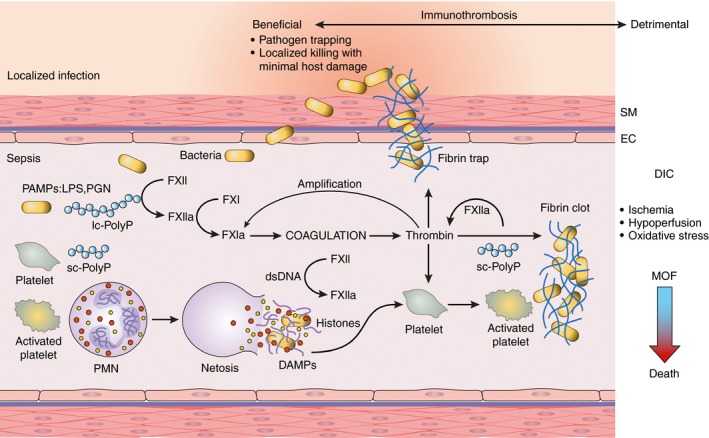
Bacteria‐induced contact activation leading to immunothrombosis and DIC. The coagulation factor XII (FXII) is activated by live bacteria and bacterial wall–derived pathogen‐associated molecular patterns (PAMPS), such as lipopolysaccharides (LPS) for gram‐negative or peptidoglycan (PGN) for gram‐positive bacteria or bacteria‐produced long‐chain polyphosphates (lc‐PolyP). Activation of FXII leads to thrombin generation, platelet activation, and fibrin formation, which in concert trap and contain pathogens. Activated platelets promote neutrophils to release their nuclear contents to form extracellular traps (netosis) as part of the routes of pathogen clearance; NETs are also potent platelet activators and cytotoxic to the host cells. Histones and double‐stranded DNA (dsDNA) act as damage‐associated pattern molecules (DAMPs) that together with platelet‐derived short‐chain polyphosphates (sc‐polyPs) contribute to contact activation via direct and indirect mechanisms. Failing the redundant pathways of pathogen clearance offered by the immune and coagulation systems, immunothrombosis can result in widespread microvascular thrombosis termed disseminated intravascular coagulation (DIC) followed by consumptive coagulopathy and bleeding. Thrombosis within the microvasculature of vital organs leads to ischemia, hypoperfusion, and oxidative stress, thus impairing organ function and leading to multiple organ failure (MOF). When more than two organs fail, death is the most likely outcome
