Abstract
Background
For subjects with out-of-hospital cardiac arrest (OHCA), bag-valve mask (BVM), endotracheal intubation (ETI), and laryngeal mask airway (LMA) are the most common methods of ventilatory support; however, the best choice remains controversial.
Methods
A comprehensive search of online databases was performed. A traditional meta-analysis was performed to determine the risk ratio of BVM vs. LMA and ETI vs. LMA. Indirect treatment comparisons (ITCs) were conducted to compare BVM and ETI.
Results
A total of 13 full-text articles reporting the efficacy of BVM, ETI, and LMA were considered in this analysis. BVM and LMA had the same effect regarding return of spontaneous circulation (ROSC) (23% vs. 24%; RR =0.84), survival rate at admission (19% vs. 21%; RR =0.82) or discharge (6% vs. 4%; RR =0.61). ETI was superior to LMA in terms of ROSC (48% vs. 23%; RR =0.72) and survival rate at both admission (27% vs. 19%; RR =0.85) and discharge (12% vs. 4%; RR =0.90). BVM was inferior to ETI in terms of ROSC (24% vs. 48%; RR =0.86), survival to admission rate (21% vs. 27%; RR =1.037), and survival to discharge rate (6% vs. 12%; RR =1.476).
Conclusions
ETI should be considered for airway management as early as possible, which can improve the subject’s success rate of recovery and survival to admission rate. In future, large-scale, multi-center, randomized controlled studies should be conducted to evaluate the exact efficacy of BVM, ETI, and LMA for the first aid of subjects with OHCA.
Keywords: Bag-valve mask (BVM), endotracheal intubation (ETI), laryngeal mask, out-of-hospital cardiac arrest subjects (OHCA subjects)
Introduction
According to current rescue strategies for subjects with out-of-hospital cardiac arrest (OHCA), immediate cardiopulmonary resuscitation (CPR) significantly improves survival. Effective ventilation is an important component in survival and is associated with return of spontaneous circulation (ROSC) and neurological recovery (1). However, the most optimal method for effective ventilation is still under debate (2).
Traditionally, bag-valve mask (BVM) is often preferred to quickly establish ventilation and gain valuable time for successful recovery of spontaneous circulation, in the meanwhile, BVM is simple and practical to perform. However, it has some shortcomings, including leakage and gas pressure on the stomach, leading to increased risk of regurgitation and pulmonary aspiration (3).
Endotracheal intubation (ETI) is considered to be the optimal method for airway management by some studies because it provides better airway control and protection against upper airway obstruction compared with BVM. It also would decrease risk of gastric aspiration and control of carbon dioxide removal. However, incorrect placement of endotracheal tube and unnecessary interruption of chest compression are associated with prolonged operation and are major drawbacks of pre-hospital ETI (4).
Laryngeal mask airway (LMA) is an alternative airway adjunct that maintains respiratory ventilation, which may enable rapid and effective airway control in comparison with BVM when used by inexperienced personnel (5). Moreover, ventilation by LMA may be particularly advantageous for subjects with facial dysmorphia and obesity (6).
Many studies have observed the characteristics of these three methods of ventilation, but the conclusion regarding which one should be considered the priority remains unclear (7,8). In this study, we aimed to comprehensively evaluate the efficacy of BVM, ETI, and LMA in rescuing adult cardiac arrest by performing a meta-analysis and indirect comparison of these three methods of ventilation.
Methods
Literature search and selection
A systematic and comprehensive literature search of online databases, including PubMed (National Library of Medicine, Bethesda, MD, USA), Web of Science (Thompson Scientific, Philadelphia, PA, USA), Embase, and Cochrane library, was performed to identify the comparative studies published before July 31, 2018. Several search terms and related variants were used, including “cardiopulmonary resuscitation”, “bag-valve mask”, “endotracheal intubation”, “laryngeal mask air way”, and their related words according to “MeSH terms”. The therapeutic effects (ROSC, survival to admission, survival to discharge) of these three methods on subjects with OHCA were examined.
All search results were evaluated according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement by two independent researchers (Z Yang and J Li) (9). The screening accuracy rate of two independent researchers were evaluated by exact Fisher’s test. The selection of original studies was based on the process of viewing titles, abstracts, and full-text papers. The inclusion criteria were as follows: (I) studies focused on adult subjects with OHCA; (II) comparative studies examining the effect between any two of these methods: BVM, ETI, and LMA; and (III) comparative studies that reported at least one outcome of interest (ROSC, survival to admission, survival to discharge). Non-comparative studies, review articles, abstracts, case reports, editorials, expert opinions, commentary articles, not published in English and letters were excluded.
Data extraction and quality assessment
Data were extracted independently by two investigators (Z Yang and J Li), and conflicts were adjudicated by a third investigator (H Liang). Information on all available variables from the selected studies was extracted. ROSC, survival to admission and survival to discharge were used to evaluate the outcomes. Quality of each clinical trial was assessed using the Newcastle-Ottawa Scale (for cohort study) (10) and Cochrane collaboration’s tool (for randomised controlled trial) for assessing risk of bias (11). Quality assessment was conducted using the Cochrane risk of bias assessment tool. Risk of bias assessment for included studies in meta-analysis was classified as “high”, “low” or “unclear”.
Statistical analysis
After studies screening, there were only comparison studies between LMA vs. BVM and LMA vs. ETI, thus indirect treatment comparisons (ITCs) were used to indirectly compare BVM and ETI, which methodology was mentioned before (12). In short, the log risk ratio (log RR) of the adjusted indirect comparison for arm A vs. B was estimated by logRRAB=logRRAC−logRRBC, and its standard error for logRR was (13):
A traditional meta-analysis was performed to determine the RR of outcomes with its 95% confidence interval (CI) for LMA vs. BVM and LMA vs. ETI. ITCs were then conducted to compare BVM and ETI using ITC computer program (Canadian Agency for Drugs and Technologies in Health, Toronto, Canada). Single arm meta-analysis was conducted to calculate the pooled rate of each outcome.
Chi-square test and I2 statistic were used to examine heterogeneity among the effect estimates (14). Statistical heterogeneity among studies was defined as I2 statistic >50%. The fixed effects model was preferred over the random effects model when there was no statistically significant heterogeneity and vice versa when there was significant heterogeneity. Publication bias was detected using funnel plots and Egger’s and Begger’s tests (15). A two-sided P<0.05 was considered statistically significant. Statistical analysis was performed using STATA 12.0 (Stata Corporation, College Station, TX, USA).
Results
Study selection and quality assessment
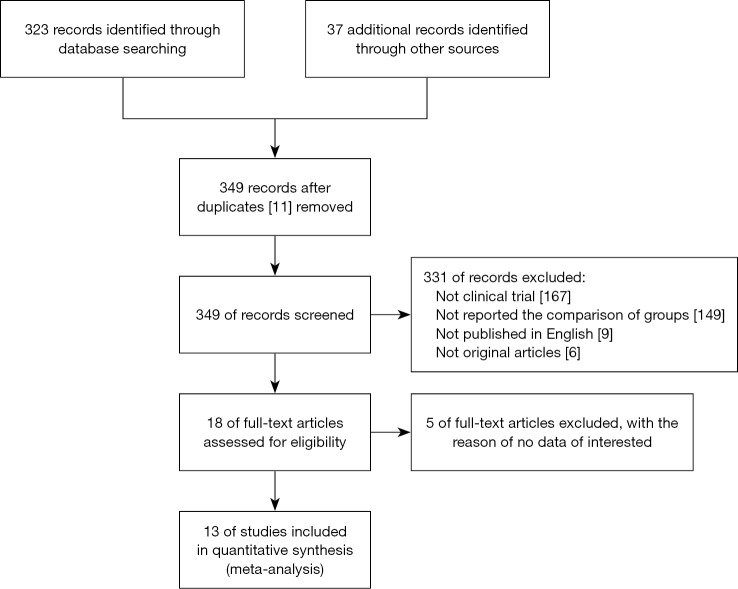
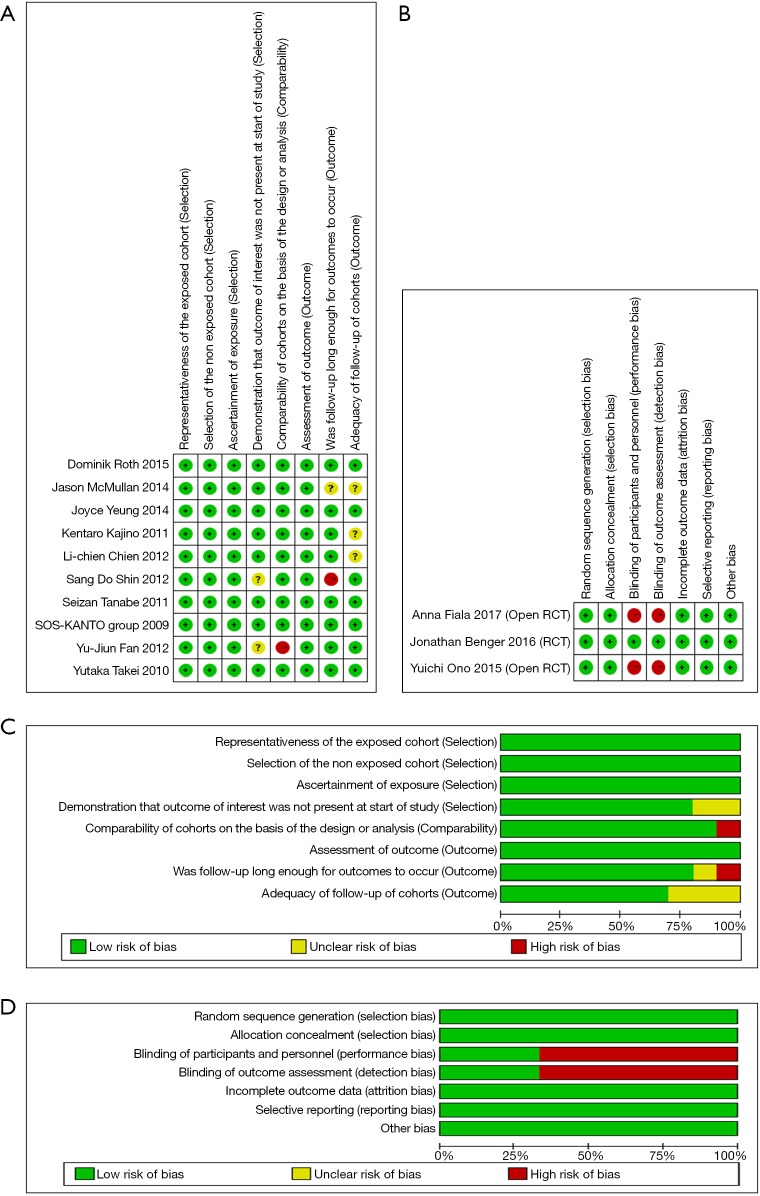
A total of 349 records were screened after exclusion of duplicates up to July 31, 2018 (Tables 1,2). The screening accuracy rate of two independent researchers were (77% vs. 70%; P=0.50). Finally, 13 full-text articles reporting efficacy among BVM, ETI, and LMA met the inclusion criteria and were considered in this analysis. Of the included articles, 4 were studies focus on LMA vs. BVM (2,16-18), 4 were studies of LMA vs. ETI (8,19-21), and 5 included both comparisons (Figure 1) (22-26). All studies got at least 7 points according to the Newcastle-Ottawa Scale and Cochrane risk of bias assessment tool (Figure 2).
Table 1. Characters of included studies (LMA vs. BVM).
| First author | Year | Region | Study type | Study period | Number of patients (n) | Age (mean/median) | Male sex (%) | Witnessed (n) | Bystander CPR (n) | Shockable rhythm (n) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | LMA | BVM | LMA | BVM | LMA | BVM | LMA | BVM | LMA | BVM | LMA | BVM | ||||||||||
| Anna Fiala | 2017 | Austria | Prospective randomized study | September 2012 to February 2014 | 76 | 35 | 41 | 69.1 | 71.4 | 23 [66] | 26 [63] | 11 | 15 | 18 | 13 | NA | NA | |||||
| Dominik Roth | 2015 | Austria | Prospective observational study | June 2011 to December 2012 | 469 | 395 | 74 | 73 | 70 | 54 [14] | 24 [32] | 184 | 30 | 171 | 21 | 181 | 26 | |||||
| Joyce Yeung | 2014 | England | Prospective observational study | November 2008 to May 2011 | 50 | 25 | 25 | 72.4 | 73.1 | 16 [64] | 19 [76] | NA | NA | NA | NA | 3 | 2 | |||||
| Li-chien Chien | 2010 | Taiwan | Prospective observational study | September 2004 to June 2007 | 398 | 309 | 89 | 63.2 | 63.2 | 209 [68] | 53 [60] | NA | NA | NA | NA | NA | NA | |||||
| SOS-KANTO group | 2009 | Japan | Prospective observational study | January 2002 to January 2004 | 382 | 173 | 209 | 64 | 64 | 149 [86] | 157 [75] | NA | NA | 61 | 84 | All | All | |||||
| Sang Do Shin | 2011 | Korea | Retrospective cohort study | January 2006 to December 2008. | 5,028 | 391 | 4,637 | 61 | 60.8 | 270 [69] | 3,154 [68] | 136 | 1,711 | 16 | 125 | 62 | 436 | |||||
| Jason McMullan | 2014 | USA | Retrospective cohort study | 2011 | 5,039 | 3,110 | 1,929 | 63.9 | 65.3 | 1,934 [62] | 1,165 [60] | NA | NA | 1,101 | 733 | 703 | 556 | |||||
| Jonathan Benger | 2016 | England | Cluster-randomized trial | 12 months (not exact year mentioned) | 383 | 174 | 209 | 71 | 71 | 104 [60] | 119 [57] | 51 | 72 | 86 | 83 | NA | NA | |||||
| Yutaka Takei | 2010 | Japan | Retrospective cohort study | July 2004 to March 2008 | 2,199 | 660 | 1,539 | 76 | 76 | 418 [63] | 890 [58] | 246 | 547 | 328 | 661 | 53 | 139 | |||||
BVM, bag-valve mask; ETI, endotracheal intubation; LMA, laryngeal mask airway; CPR, cardiopulmonary resuscitation.
Table 2. Characters of included studies (LMA vs. ETI).
| First author | Year | Region | Study type | Study period | Number of patients (n) | Age (mean/median) | Male sex (%) | Witnessed (n) | Bystander CPR (n) | Shockable rhythm (n) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | LMA | ETI | LMA | ETI | LMA | ETI | LMA | ETI | LMA | ETI | LMA | ETI | ||||||||||
| Seizan Tanabe | 2011 | Japan | Retrospective cohort study | 2005–2007 | 50,179 | 34,125 | 16,054 | 72.1 | 73.8 | 20,657 [61] | 9,397 [59] | 13,413 | 7,126 | 12,930 | 6,722 | 2,943 | 1,201 | |||||
| Yuichi Ono | 2015 | Japan | Prospective randomized study | 2012–2013 | 313 | 148 | 165 | 75.84 | 72.41 | 101 [68] | 90 [55] | 63 | 52 | 74 | 42 | 8 | 17 | |||||
| Yu-Jiun Fan | 2012 | Taiwan | Observational study | January to June 2010 | 481 | 294 | 31 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |||||
| Jonathan Benger | 2016 | England | Prospective randomized study | 12 months (not exact year mentioned) | 406 | 174 | 232 | 71 | 70 | 104 [60] | 144 [62] | 51 | 73 | 86 | 106 | NA | NA | |||||
| Kentaro Kajino | 2011 | Japan | Prospective cohort study | January 2005 to December 2008 | 5,377 | 3,698 | 1,679 | 71.9 | 73.8 | 2,291 [62] | 1,021 [61] | NA | NA | 1,472 | 686 | 622 | 278 | |||||
| Sang Do Shin | 2011 | Korea | Retrospective cohort study | January 2006 to December 2008 | 5,028 | 391 | 4,637 | 61 | 60.8 | 270 [69] | 3,154 [68] | 136 | 1,711 | 16 | 125 | 62 | 436 | |||||
| Yutaka Takei | 2010 | Japan | Retrospective cohort study | July 2004 to March 2008 | 923 | 660 | 263 | 76 | 76 | 418 [63] | 154 [59] | 246 | 105 | 328 | 130 | 53 | 18 | |||||
| Jason McMullan | 2014 | USA | Retrospective cohort study | 2011 | 5,039 | 3,110 | 1,929 | 63.9 | 65.3 | 1934 [62] | 1,165 [60] | NA | NA | 1,101 | 733 | 703 | 556 | |||||
| Joyce Yeung | 2014 | England | Prospective observational study | November 2008 to May 2011 | 50 | 25 | 25 | 72.4 | 73.1 | 16 [64] | 19 [76] | NA | NA | NA | NA | 3 | 2 | |||||
BVM, bag-valve mask; ETI, endotracheal intubation; LMA, laryngeal mask airway; CPR, cardiopulmonary resuscitation.
Figure 1.
Flow diagram detailing the search strategy and identification of studies used in meta-analysis.
Figure 2.
Quality assessment of included studies. Quality assessment was conducted using the Cochrane risk of bias assessment tool. Risk of bias assessment for included studies in meta-analysis was classified as “high”, “low” or “unclear”. (A,C) Quality assessment of cohort studies; (B,D) quality assessment of randomised controlled trial.
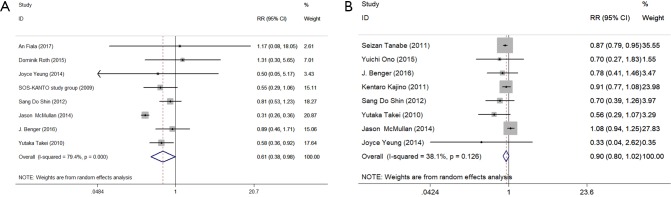
ROSC
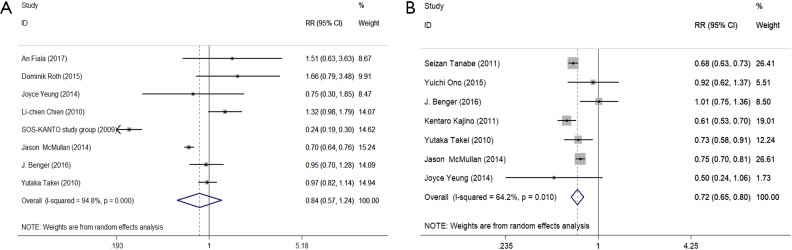
In total, 8 studies reported ROSC between LMA and BVM. The random model was used. The result showed that there was no significant difference between LMA and BVM (23% vs. 24%; RR =0.84; 95% CI, 0.57–1.24; heterogeneity: I2=94.8%, P<0.001) (Figure 3A). ETI was significantly superior to LMA in ROSC based on the pooled analysis of 7 studies (48% vs. 23%; RR =0.72; 95% CI, 0.65–0.80; heterogeneity: I2=64.2%, P=0.01) (Figure 3B). According to indirect comparison, no difference was observed between BVM and ETI in improving ROSC (24% vs. 48%; RR =0.86; 95% CI, 0.58–1.28).
Figure 3.
Forest plot of return of spontaneous circulation. (A) LMA vs. BVM; (B) LMA vs. ETI. BVM, bag-valve mask; ETI, endotracheal intubation; LMA, laryngeal mask airway; CPR, cardiopulmonary resuscitation; RR, risk ratio; CI, confidence interval.
Survival to admission
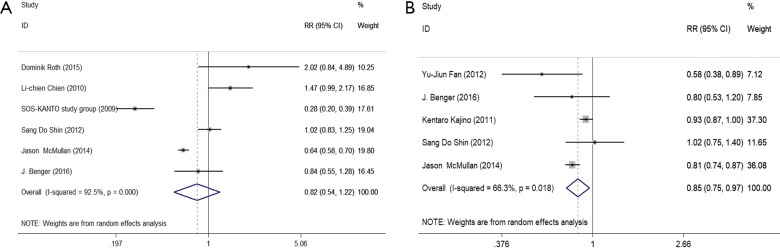
In total, 6 studies reported the survival status between LMA and BVM when subjects were admitted to hospitals. The result indicated no significance existed between LMA and BVM (19% vs. 21%; RR =0.82; 95% CI, 0.54–1.22; heterogeneity: I2=92.5%, P<0.001) (Figure 4A). ETI was significantly superior to LMA in improving survival rate on admission based on the pooled analysis of 5 studies (27% vs. 19%; RR =0.85; 95% CI, 0.75–0.97; heterogeneity: I2=66.3%, P=0.018) (Figure 4B). According to indirect comparison, an equal admission survival rate was observed when BVM was compared with ETI (21% vs. 27%; RR =1.037; 95% CI, 0.677–1.589).
Figure 4.
Forest plot of survive to admission. (A) LMA vs. BVM; (B) LMA vs. ETI. BVM, Bag-valve mask; ETI, endotracheal intubation; LMA, laryngeal mask airway; CPR, cardiopulmonary resuscitation; RR, risk ratio; CI, confidence interval.
Survival to discharge
In total, 8 studies reported the survival status between LMA and BVM when subjects were discharged. The result showed BVM was significantly better than LMA (6% vs. 4%; RR =0.61; 95% CI, 0.38–0.98; heterogeneity: I2=79.4%, P<0.001) (Figure 5A). ETI was equal to LMA in improving survival rate when discharged (12% vs. 4%; RR =0.90; 95% CI, 0.80–1.02; heterogeneity: I2=38.1%, P=0.126) (Figure 5B). According to an indirect comparison, a comparable survival rate at discharge was observed between BVM and ETI (6% vs. 12%; RR =1.476; 95% CI, 0.905–2.407).
Figure 5.
Forest plot of survive to discharge. (A) LMA vs. BVM; (B) LMA vs. ETI. BVM, bag-valve mask; ETI, endotracheal intubation; LMA, laryngeal mask airway; CPR, cardiopulmonary resuscitation; RR, risk ratio; CI, confidence interval.
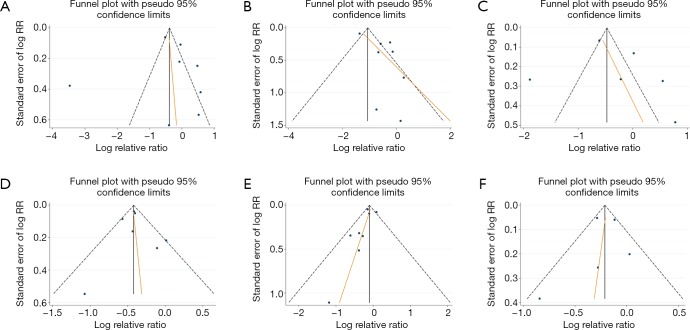
Publication bias and sensitivity analysis
Visual inspection of funnel plots suggested a symmetric distribution for majority of the outcomes (Figure 6). Begg and Egger’s test confirmed there was no significant publication bias. A sensitivity analysis was performed by excluding the studies with the lowest-quality score. This did not influence the results.
Figure 6.
Funnel plot of outcomes. (A) ROSC LMA vs. BVM; (B) ROSC LMA vs. ETI; (C) survive to admission LMA vs. BVM; (D) survive to admission LMA vs. ETI; (E) survive to discharge LMA vs. BVM; (F) survive to discharge LMA vs. ETI. BVM, bag-valve mask; ETI, endotracheal intubation; LMA, laryngeal mask airway; CPR, cardiopulmonary resuscitation; RR, risk ratio; CI, confidence interval. ROSC, return of spontaneous circulation.
Discussion
For subjects with OHCA, ineffective ventilation is the most common clinical event contributing to severe respiratory depression and worse survival outcomes. BVM, ETI, and LMA are the most common methods of ventilation support, but the best choice is still controversial. Herein, we conducted a meta-analysis and indirect comparison of these three methods, and the results indicated that ETI offers the best outcomes among these three methods and LMA is relatively inferior to the other two methods.
BVM is the most commonly used ventilation airway adjunct and has been widely used for pre-hospital emergencies. It is simple and practical to operate and can quickly establish ventilation and gain valuable time for successful recovery. However, efficiency of the ventilation depends on whether the airway is effectively open and whether the mask is tightly closed. In a pre-hospital rescue, improper operation leads to flatulence, food reflux, and even suffocation.
ETI has been a “gold standard” for the airway management of subjects with OHCA for a long time (27). In the United States, 80% of subjects with OHCA are treated with ETI for advanced airway management during CPR (23). It provides better airway protection and ventilation control to prevent upper airway obstruction and effectively reduces the risk of bloating, reflux aspiration, and carbon dioxide retention. Nevertheless, ETI also has shortcomings in pre-hospital rescue, such as aspiration pneumonia, insertion into the esophagus, time-consuming preparation, unnecessary interruption of chest compression, complex requirements for intubation, and high failure rate. As a result, out-of-hospital ETI has been increasingly questioned as the preferred method of management of advanced airways (28,29).
LMA is a common supraglottic respiration airway adjunct that has been listed by the American Society of Anesthesiologists as a first-aid method for subjects with difficult airways. It can quickly establish and maintain respiratory ventilation. Moreover, in comparison with ETI, laryngoscope is not needed, and the success rate is higher than that of ETI. Even if LMA is not properly placed, it can maintain an unobstructed airway and is suitable for first-time emergency use. In Japan, South Korea, and other countries, LMA is widely used for resuscitation of subjects with OHCA as an alternative to airway management, such as ETI (8,19,24). However, it also has some shortcomings, such as poor sealing, displacement during transportation, flatulence, food reflux aspiration, and pharyngeal wall or epiglottis edema.
All three methods have advantages and disadvantages, but which method of ventilation should be chosen for subjects with OHCA? A meta-analysis of neonatal resuscitation by Qureshi et al. (7) suggested that LMA can achieve effective ventilation during neonatal resuscitation. However, in the present study, when a meta-analysis of adult subjects was conducted on these three methods of ventilation for pre-hospital cardiac arrest resuscitation, the results were unexpected.
BVM ventilation is recommended by the 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care and the European Resuscitation Committee (30,31) when professionals perform early CPR on subjects with OHCA. With respect to bystander CPR with chest compression only, a prospective multicenter, non-randomized controlled trial SOS-KANTO (18) reported that the arterial potential of hydrogen (pH) of the extracorporeal ventricular fibrillation or pulseless ventricular tachycardia was higher in the LMA group than in the BVM group, but LMA was not as beneficial as BVM in improving the respiratory status of such subjects. A large study of 649,359 subjects in Japan with OHCA found that subjects with BVM had better neurological outcomes after 1 month than subjects with LMA or ETI, and this was thought to be related to the benefits of sustained chest compressions (32).
In our analysis, although without significance, the use of ETI offered an absolute higher survival rate for subjects with OHCA in comparison to BVM and LMA, in the meanwhile, ETI was also associated a higher success rate of recovery and the rate of hospital admission after successful recovery. However, from the trend of the forest plot, the success rate of recovery and the rate of live admission were similar for subjects treated with BVM and LMA. Therefore, for unskilled rescuers, to reduce the interruption time of chest compression and improve the success rate of resuscitation, BVM should be preferred for early CPR. But according to our study, ETI should be considered when the mask cannot be fixed to ensure ventilation or long-distance transportation.
Pre-hospital first aid in European countries, Canada, Australia, and the United States had excellent outcomes for ETI for advanced airway management. Although emergency medical services (EMSs) are available in most Asian countries, emergency personnel have limited experience with pre-hospital ETI (33,34). A study by Kajino (21) showed that professionals can quickly and effectively perform successful ETI for subjects with OHCA. Wang et al. (35) found that ETI was associated with a better 24-hour survival rate and a higher discharge rate and was more effective in achieving ROSC in comparison to LMA. However, EMSs in many Asian countries still encourage pre-hospital first-responders to use LMA as the most common method of airway management. Our meta-analysis of the success rate of recovery, survival to admission rate, and survival to discharge rate of subjects with OHCA demonstrated that ETI is more beneficial than LMA for subjects with OHCA. This may be due to the following reasons. Firstly, LMA may shift the ventilation quality during transport and care of subjects. Secondly, pre-hospital first-responders are unfamiliar with the LMA procedure. Finally, in comparison with LMA, ETI can better manage airway secretions and reduce the aspiration of gastric reflux, which is helpful in improving the respiratory status of subjects (23).
There are several limitations to our study: firstly, not all included studies were prospective comparisons, leading to data deficiency and potential selection and reporting bias in some outcomes; secondly, the majority of included studies reported an insufficient follow-up period, consequently, we were unable to evaluate long-term outcomes, such as 1 year survival rate after OHCA; third, small-study effects refer to the pattern that small studies are more likely to report beneficial effect in the intervention arm (36), although the funnel plot showed there was no obvious study bias in our analysis, some small-sample studies could still potentially affect the outcomes; finally, we have to admit the methodology of ITC has limitation of estimating HR, substantially diminishing the statistical significance, thus its evidence level is not as strong as traditional meta-analysis.
For subjects with OHCA, ETI should be considered for airway management as early as possible, which can improve the subject’s success rate of recovery and survival to admission rate. In future, large-scale, multi-center, randomized controlled studies should be conducted to evaluate the exact efficacy of BVM, ETI, and LMA for the first aid of subjects with OHCA, particularly the long-term effects, such as survival and discharge rates and quality of life after discharge.
Acknowledgments
Funding: This work was supported by the following funding (Funder: L Rong): Science and Technology Foundation of Guangdong Province, China (2012B061700046), and the Research Program for Colleges and Universities in Guangzhou (2012C054).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2307-15. 10.1056/NEJMoa1405796 [DOI] [PubMed] [Google Scholar]
- 2.Fiala A, Lederer W, Neumayr A, et al. EMT-led laryngeal tube vs. face-mask ventilation during cardiopulmonary resuscitation - a multicenter prospective randomized trial. Scand J Trauma Resusc Emerg Med 2017;25:104. 10.1186/s13049-017-0446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khoury A, Hugonnot S, Cossus J, et al. From mouth-to-mouth to bag-valve-mask ventilation: evolution and characteristics of actual devices--a review of the literature. Biomed Res Int 2014;2014:762053. 10.1155/2014/762053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jarman AF, Hopkins CL, Hansen JN, et al. Advanced Airway Type and Its Association with Chest Compression Interruptions During Out-of-Hospital Cardiac Arrest Resuscitation Attempts. Prehosp Emerg Care 2017;21:628-35. 10.1080/10903127.2017.1308611 [DOI] [PubMed] [Google Scholar]
- 5.Maignan M, Koch FX, Kraemer M, et al. Impact of laryngeal tube use on chest compression fraction during out-of-hospital cardiac arrest. A prospective alternate month study. Resuscitation 2015;93:113-7. 10.1016/j.resuscitation.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 6.Keilholz G, Mutzbauer TS. The laryngeal tube - a helpful tool for cardiopulmonary resuscitation in the dental office? Br Dent J 2015;218:E15. 10.1038/sj.bdj.2015.385 [DOI] [PubMed] [Google Scholar]
- 7.Qureshi MJ, Kumar M. Laryngeal mask airway versus bag-mask ventilation or endotracheal intubation for neonatal resuscitation. Cochrane Database Syst Rev 2018;3:CD003314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanabe S, Ogawa T, Akahane M, et al. Comparison of neurological outcome between tracheal intubation and supraglottic airway device insertion of out-of-hospital cardiac arrest patients: a nationwide, population-based, observational study. J Emerg Med 2013;44:389-97. 10.1016/j.jemermed.2012.02.026 [DOI] [PubMed] [Google Scholar]
- 9.Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg 2011;39:91-2. 10.1016/j.jcms.2010.11.001 [DOI] [PubMed] [Google Scholar]
- 10.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang Q, Wei Y, Chen YX, et al. Indirect comparison showed survival benefit from adjuvant chemoradiotherapy in completely resected gastric cancer with d2 lymphadenectomy. Gastroenterol Res Pract 2013;2013:634929. 10.1155/2013/634929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mauger D, Apter AJ. Indirect treatment comparisons and biologics. J Allergy Clin Immunol 2019;143:84-6. 10.1016/j.jaci.2018.11.005 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chien LC, Hsu HC, Lin CH, et al. Use of an intubating laryngeal mask airway on out-of-hospital cardiac arrest patients in a developing emergency medical service system. J Formos Med Assoc 2012;111:24-9. 10.1016/j.jfma.2012.01.004 [DOI] [PubMed] [Google Scholar]
- 17.Roth D, Hafner C, Aufmesser W, et al. Safety and feasibility of the laryngeal tube when used by EMTs during out-of-hospital cardiac arrest. Am J Emerg Med 2015;33:1050-5. 10.1016/j.ajem.2015.04.048 [DOI] [PubMed] [Google Scholar]
- 18.SOS-KANTO study group Comparison of arterial blood gases of laryngeal mask airway and bag-valve-mask ventilation in out-of-hospital cardiac arrests. Circ J 2009;73:490-6. 10.1253/circj.CJ-08-0874 [DOI] [PubMed] [Google Scholar]
- 19.Ono Y, Hayakawa M, Maekawa K, et al. Should laryngeal tubes or masks be used for out-of-hospital cardiac arrest patients? Am J Emerg Med 2015;33:1360-3. 10.1016/j.ajem.2015.07.043 [DOI] [PubMed] [Google Scholar]
- 20.Fan YJ, Dai CY, Huang DC, et al. Does tracheal intubation really matter? Discrepant survival between laryngeal mask and endotracheal intubation during out-of-hospital cardiac arrest. J Formos Med Assoc 2017;116:134-5. 10.1016/j.jfma.2016.11.001 [DOI] [PubMed] [Google Scholar]
- 21.Kajino K, Iwami T, Kitamura T, et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit Care 2011;15:R236. 10.1186/cc10483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benger J, Coates D, Davies S, et al. Randomised comparison of the effectiveness of the laryngeal mask airway supreme, i-gel and current practice in the initial airway management of out of hospital cardiac arrest: a feasibility study. Br J Anaesth 2016;116:262-8. 10.1093/bja/aev477 [DOI] [PubMed] [Google Scholar]
- 23.McMullan J, Gerecht R, Bonomo J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation 2014;85:617-22. 10.1016/j.resuscitation.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 24.Shin SD, Ahn KO, Song KJ, et al. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation 2012;83:313-9. 10.1016/j.resuscitation.2011.10.028 [DOI] [PubMed] [Google Scholar]
- 25.Takei Y, Enami M, Yachida T, et al. Tracheal intubation by paramedics under limited indication criteria may improve the short-term outcome of out-of-hospital cardiac arrests with noncardiac origin. J Anesth 2010;24:716-25. 10.1007/s00540-010-0974-6 [DOI] [PubMed] [Google Scholar]
- 26.Yeung J, Chilwan M, Field R, et al. The impact of airway management on quality of cardiopulmonary resuscitation: an observational study in patients during cardiac arrest. Resuscitation 2014;85:898-904. 10.1016/j.resuscitation.2014.02.018 [DOI] [PubMed] [Google Scholar]
- 27.Wang HE, Kupas DF, Paris PM, et al. Preliminary experience with a prospective, multi-centered evaluation of out-of-hospital endotracheal intubation. Resuscitation 2003;58:49-58. 10.1016/S0300-9572(03)00058-3 [DOI] [PubMed] [Google Scholar]
- 28.Fullerton JN, Roberts KJ, Wyse M. Can experienced paramedics perform tracheal intubation at cardiac arrests? Five years experience of a regional air ambulance service in the UK. Resuscitation 2009;80:1342-5. 10.1016/j.resuscitation.2009.07.023 [DOI] [PubMed] [Google Scholar]
- 29.Raatiniemi L, Lankimaki S, Martikainen M. Pre-hospital airway management by non-physicians in Northern Finland -- a cross-sectional survey. Acta Anaesthesiol Scand 2013;57:654-9. 10.1111/aas.12101 [DOI] [PubMed] [Google Scholar]
- 30.Neumar RW, Shuster M, Callaway CW, et al. Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S315-67. 10.1161/CIR.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 31.Monsieurs KG, Nolan JP, Bossaert LL, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015;95:1-80. 10.1016/j.resuscitation.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 32.Hasegawa K, Hiraide A, Chang Y, et al. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA 2013;309:257-66. 10.1001/jama.2012.187612 [DOI] [PubMed] [Google Scholar]
- 33.Springer DK, Jahr JS. The laryngeal mask airway. Safety, efficacy, and current use. Am J Anesthesiol 1995;22:65-9. [PubMed] [Google Scholar]
- 34.Barata I. The laryngeal mask airway: prehospital and emergency department use. Emerg Med Clin North Am 2008;26:1069-83, xi. 10.1016/j.emc.2008.07.006 [DOI] [PubMed] [Google Scholar]
- 35.Wang HE, Kupas DF, Greenwood MJ, et al. An algorithmic approach to prehospital airway management. Prehosp Emerg Care 2005;9:145-55. 10.1080/10903120590924618 [DOI] [PubMed] [Google Scholar]
- 36.Zhang Z, Xu X, Ni H. Small studies may overestimate the effect sizes in critical care meta-analyses: a meta-epidemiological study. Crit Care 2013;17:R2. 10.1186/cc11919 [DOI] [PMC free article] [PubMed] [Google Scholar]