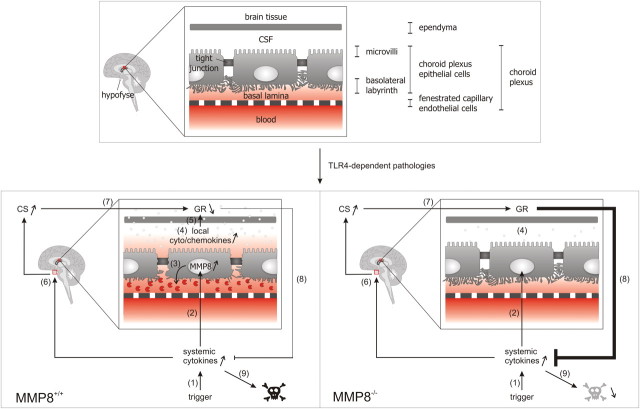
Figure 7.
Effect of TLR4-mediated pathologies and MMP8 deficiency on BCSFB and lethality. 1, During a trigger, such as sepsis or kidney I/R, systemic cytokine levels are increased. 2, This increase results in MMP8 upregulation in the CP, a highly perfused organ in which a single epithelial cell layer separates the blood from the CSF. Importantly, the CP regulates homeostasis in the CNS but also participates in the interaction between the periphery and the brain. 3, The increase in MMP8 subsequently leads to collagen I cleavage, resulting in morphological changes of the choroidal epithelial cells: loss of cuboidal shape and loss of basal labyrinth. 4, Next, this injury of the CP causes impairment of the BCSFB and increases local cytokine and chemokine levels. 5, When these chemokines and cytokines leak into the surrounding brain tissue, this results in increased local inflammation and downregulation of the GR. Steps 3–5 are absent or reduced in the MMP8−/− mice. 6, Increased systemic cytokine levels also lead to activation of the HPA axis, which results in upregulation of corticosterone (CS) serum levels. 7, CS activates to the GR, which is an important feedback mechanism in inflammatory conditions, ensuring the appropriate dampening of the inflammatory response. 8, Downregulation of the GR in the brain after LPS challenge, detected in the MMP8+/+ but not in the MMP8−/− mice, reduces the anti-inflammatory effect of the corticosterone activated GR. 9, The resulting exaggerated immune response in the MMP8+/+ mice causes MOF and death, which is reduced in the MMP8−/− mice.