Abstract
Surgical management for glenohumeral instability has advanced to provide stronger fixation and to be less invasive. Arthroscopic suture anchor repair has been the gold standard for isolated capsulolabral tears over the years. Despite the ability of the solid suture anchors to handle physiologic load, they can present challenges such as chondral damage due to anchor size and imperfect angulation, osteolysis, anchor breakage, revision drilling, difficulty of revision surgery with accompanied bone loss, and compromised postoperative magnetic resonance imaging quality. Recently, knotless all-suture anchors have been introduced as a technique to overcome these challenges. These anchors lack a rigid component and can be placed in a tunnel of smaller diameter, thereby allowing for maintenance of glenoid bone stock. The purpose of this Technical Note is to describe our preferred surgical technique with a minimally invasive approach for the fixation of capsulolabral tears using a knotless all-suture anchor construct.
Surgical techniques for anterior shoulder stabilization have advanced to provide safer and stronger fixation methods. Recently, the development of all-suture anchors has grown in popularity in arthroscopic stabilization. All-suture anchors are advantageous because they preserve bone stock, improve postoperative imaging after surgery, and may facilitate easier revision surgery if necessary.1 Furthermore, due to a lack of a rigid component and curved guides, correct and simple anchor placement without impairment of the subscapularis tendon is possible. There are concerns about all-suture anchors regarding the biomechanical load; however, studies comparing all-suture anchors and solid suture anchors have shown similar biomechanical properties between the 2 anchors.2 A knotless, tensionable all-suture anchor has been developed (FiberTak, Arthrex, FL), which eliminates the potential problems associated with knot tying such as knot migration, knot impingement, and chondral abrasion.3, 4 The aim of this Technical Note is to report on a technique using knotless all-soft suture anchors and provide the pearls and pitfalls of this strategy.
Surgical Technique
Preoperative Planning
In addition to taking a comprehensive history, a global and functional examination is performed to determine the instability direction, the general joint laxity (healthy contralateral shoulder), and possible concomitant pathologies. In addition, an imaging assessment that includes anteroposterior, axial, and y-view radiographs as well as magnetic resonance imaging is mandatory to rule out relevant bony defects and to evaluate for possible concomitant soft tissue pathologies.5, 6 If radiographs or magnetic resonance imaging are suspicious for glenoid or humeral bone defects, 2- or 3-dimensional computed tomography can help assess size, shape, and location of bony glenoid fragments and/or Hill-Sachs lesions.
Patient Position
After induction of general anesthesia, the patient is placed in the beach chair position. The operative extremity is fixed in a mechanical arm holder (e.g., Trimano, Arthrex), and the operative shoulder and axilla are prepared and draped using standard sterile fashion. A careful examination under anesthesia is performed to assess the stability and the degree of joint translation.
Portal Placement and Diagnostic Arthroscopy
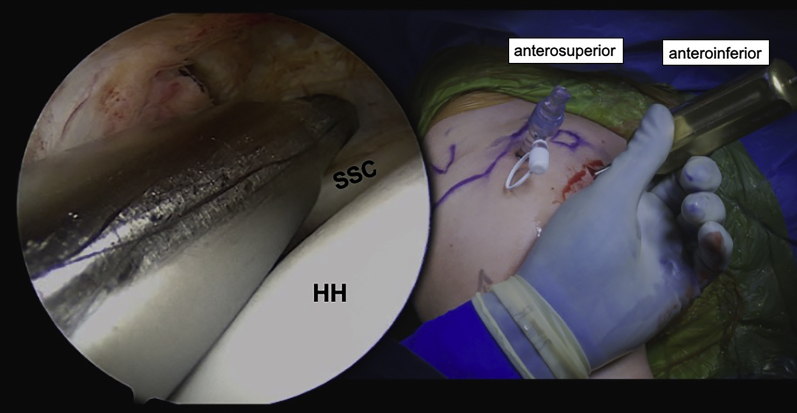
The complete surgical technique is shown in Video 1. Three standard portals are required for this arthroscopic procedure: a standard posterior portal, an anterosuperior portal (upper rotator cuff interval), and an anteroinferior portal (above the upper border of the subscapularis tendon; Fig 1).
Fig 1.
Right shoulder: operative setup showing the anteroinferior and anterosuperior portals with a cannula placed through the anterosuperior portal. A second canula is being placed via the anteroinferior portal just above the upper border of the subscapularis tendon. HH, humeral head; SSC, subscapularis tendon.
Two cannulas are placed into the anterior portals. A 5.0-mm cannula is used in the superior portal. This portal is made quite high in the interval and parallel to the glenoid. An 8.25-mm cannula is used in the anteroinferior portal. This portal enters from slightly lateral in the rotator interval and just superior to the subscapularis tendon (Fig 1). A larger portal is needed to insert the suture shuttling device (Lasso, Arthrex). The camera for the diagnostic arthroscopy is placed through the posterior portal and is aligned parallel with the glenoid.
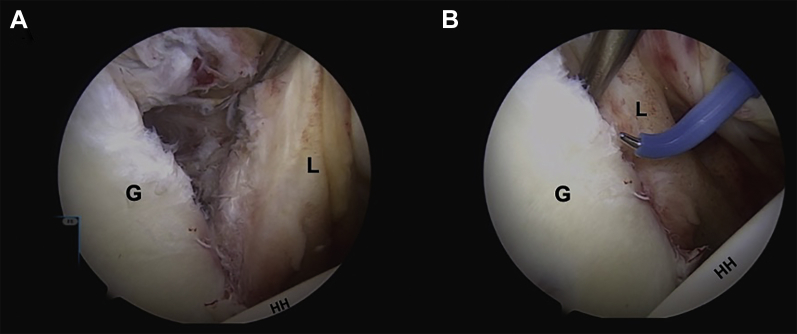
A diagnostic arthroscopy is performed next. First, the suspected primary structural lesions at the anteroinferior glenoid rim (Fig 2) and posterolateral humeral head (Hill-Sachs lesion) are identified. Second, concomitant lesions, for example, rotator cuff injuries in elderly patients, SLAP lesion, or pathology of the long head of the biceps tendon, are assessed.7, 8 To better evaluate the anteroinferior glenoid rim and its capsulolabral attachments, the use of a 70° scope is recommended. Additionally, evaluating the Bankart lesion from the anterosuperior portal can be helpful.
Fig 2.
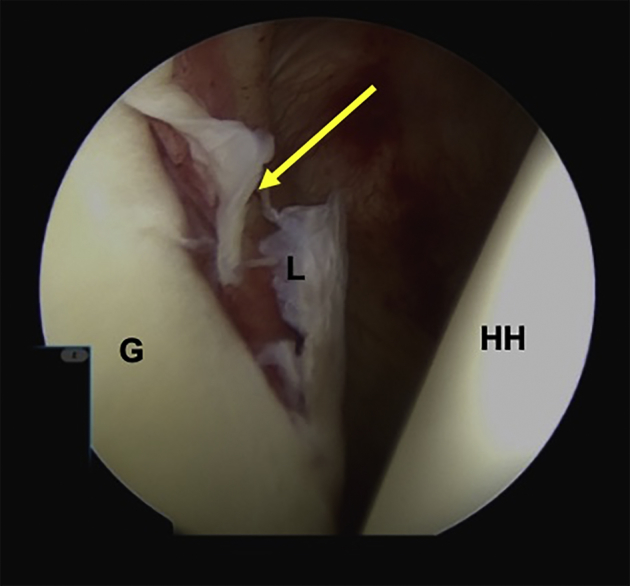
Right shoulder: Arthroscopic visualization of the anterior capsulolabral defect (arrow) seen through posterior portal. G, glenoid; HH, humeral head; L, labrum.
Capsulolabral Release and Glenoid Rim Preparation
While viewing with a 70° scope through the posterior portal, the capsulolabral complex is extensively mobilized using a periosteal elevator (Fig 3A; Periosteal Elevator, Arthrex). An electrothermal instrument can also be used through the anterosuperior portal to carefully elevate the capsulolabral sleeve (Fig 3B).
Fig 3.
(A) Right shoulder: with the arthroscope in the posterior portal, the capsulolabral tissue can be elevated and mobilized with a periosteal elevator through the anterosuperior portal. (B) An electrothermal instrument is used to release the labrum and capsular sleeve from the glenoid neck. G, glenoid; HH, humeral head; L, labrum.
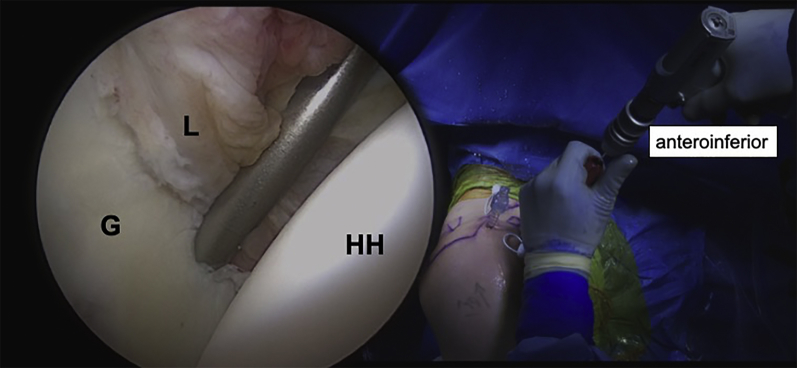
The glenoid neck is then debrided by the use of a rasp or oscillating burr (Fig 4), and the footprint of the capsule attachment on the glenoid neck is prepared until a denuded surface is created with slight bleeding to facilitate bone-to-capsule healing.
Fig 4.
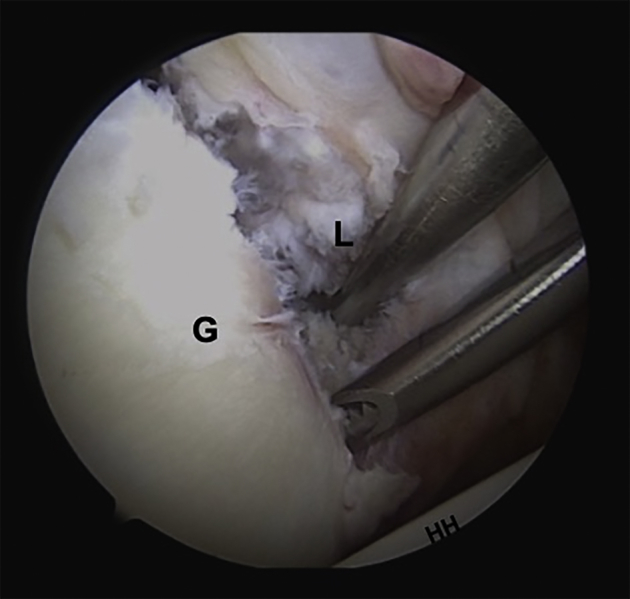
Right shoulder: arthroscopic visualization through the posterior portal showing debridement and preparation of the glenoid neck with an oscillating burr to create a denuded surface for healing. G, glenoid; HH, humeral head; L, labrum.
Capsulolabral Repair
The capsulolabral complex is mobilized, and the amount of capsular shift is determined based on a number of factors such as the severity of instability, the degree of capsular laxity, and the extent of the tissue mobilization. The capsulolabral sleeve should be reattached with at least 3, preferably 4 or 5, knotless, all-suture anchors in a simple stitch configuration (1.8 mm FiberTak, Arthrex).
First, the most inferior anchor is placed at the 5:30 o’clock position. A curved drill sleeve makes this easier and is placed through the anteroinferior portal to the glenoid rim. The drill hole and anchor should be placed 1 to 2 mm on the glenoid faces to achieve the appropriate restoration of the labrum. If the appropriate trajectory cannot be achieved using the anteroinferior portal, the drill guide can be inserted percutaneously through the subscapularis to achieve the appropriate position on the glenoid face as well as the appropriate trajectory. After drilling through the curved drill guide (Fig 5), the first all-suture anchor is inserted into the bone tunnel through the drill guide. The anchor should be started by hand into the tunnel to make sure it is seated properly before it is impacted into its final position. The anchor is then gently pulled to expand the anchor and seat it securely in the bone tunnel of the glenoid.
Fig 5.
Right shoulder: a curved drill sleeve is placed through the anteroinferior portal to the glenoid rim at 5:30 o’clock position. G, glenoid; HH, humeral head; L, labrum.
The repair suture (colored white-blue) is retrieved through the anterosuperior portal with a tape retriever (Fiber Tape Retriever, Arthrex). A 25° angulated shuttling device (Suture lasso, Arthrex) is then inserted through the anteroinferior cannula, and the capsule is penetrated lateral to the glenoid and inferior to the anchor (Fig 6A). The farther lateral and the farther inferior that the shuttling device penetrates the capsule, the greater the degree of capsular shift. A handheld grasper is used to shift and stabilize the tissue while the shuttling device is passed through it. The tip of the shuttling device passes around the labrum and comes intra-articular again between the osteochondral junction of the glenoid medially and the labrum ring laterally (Fig 6B).
Fig 6.
(A) Right shoulder: the angulated suture-shuttling device is placed in the anteroinferior cannula and penetrates the capsule lateral to the glenoid rim and inferior to the anchor. (B) Reduction of the capsulolabral defect to the glenoid rim with a grasper while penetrating the capsule with the shuttling device. G, glenoid; HH, humeral head; L, labrum.
While the capsulolabral tissues are being shifted, the capsulolabral complex can be reduced to the glenoid rim with the help of the grasper through the anterosuperior portal. Once the nitinol wire is introduced into the joint, it is retrieved through the anterosuperior portal using the grasper (Fig 6B). The repair suture is placed into the wire loop and shuttled through the soft tissue and exits out of the anteroinferior portal. The repair suture is now successfully passed around the capsulolabral tissue, although it still needs to be passed back through the self-locking mechanism.
The anchor has a shuttling suture built into its mechanism that allows the repair suture to be passed back through the self-locking mechanism. All longitudinal twists should be carefully removed from the repair suture. The repair suture is then passed through the looped end of the shuttle suture (colored white-black), and the free end of the shuttle suture is pulled until the repair suture passes back into the self-locking mechanism of the anchor. The self-locking mechanism is buried within the bone tunnel. Before the self-locking repair stitch loop is tightened (loop security), an additional shift of the capsulolabral complex can be achieved by grabbing the tissue with a grasper and holding it in the desired position while the repair suture is tensioned (Fig 7). Tension should now be applied to the repair suture to secure the capsulolabral tissues, until the desired loop tension is achieved.
Fig 7.
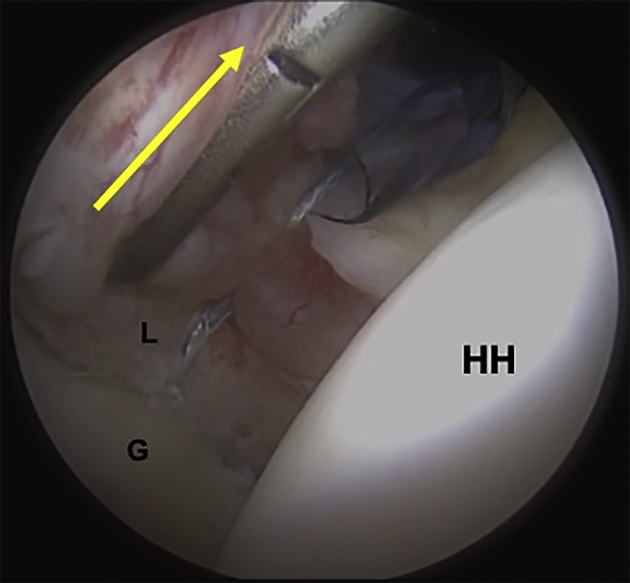
Right shoulder: an additional capsulolabral shift is achieved by using a grasper to shift the tissue superiorly while the loop of the repair suture is tightened (arrow). This shifts the capsulolabral tissue to the desired position. G, glenoid; HH, humeral head; L, labrum.
Finally, using a minisuture cutter, which cuts the suture flush, the free suture end is cut, creating a knotless construct. In this way, there is no knot stack and the repair stitch retensions the capsulolabral complex. Alternatively, the suture can be left uncut until all anchors are placed and then retensioned at the end of the procedure.
The process is repeated 3 to 5 times for each anchor working from inferior to superior, depending on the extent of the tear and desired degree of shift and stability that is needed.
The first anchor typically is used to shift the inferior glenohumeral ligament complex and labrum superiorly and tighten the axillary pouch. The second anchor is typically placed at the level of the anterior band of the inferior glenohumeral ligament. The third anchor is typically placed at the level of the middle glenohumeral ligament, and the fourth anchor is used to repair the anterosuperior labrum.
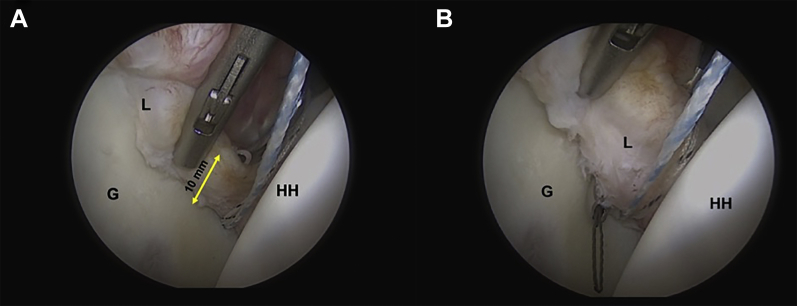
A minimum of 3, but preferably 4 or more, anchors should be placed for an adequate Bankart repair. Because the anchors are so small and so little bone is removed, it is easier to place more anchors, which creates more points of fixation along the anterior glenoid rim. For a right shoulder, the anchors are typically placed at the 5:30, 4:00 3:30, and 2 o’clock positions with an average anchor-to-anchor distance of 7 mm in the superior direction (Fig 8). If there is an associated SLAP tear, the repair is continued superiorly to secure the biceps anchor.9
Fig 8.
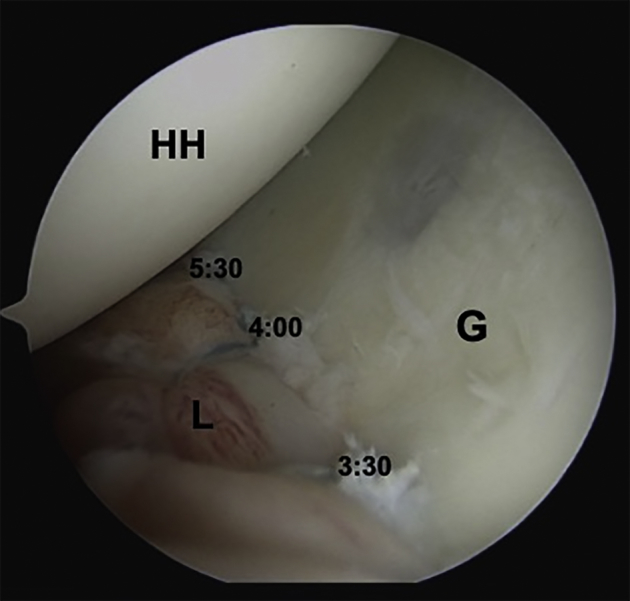
Right shoulder: with the arthroscope in the anterosuperior portal, visualization of final repair is seen with anchors at the 3:30, 4:00, and 5:30 positions and an average distance of 7 mm in the superior direction. G, glenoid; HH, humeral head; L, labrum.
Postoperative Rehabilitation
Following surgery, patients are protected in a sling for 4 weeks. During this time, rehabilitation focuses on gentle passive motion, protecting the surgical repair, alleviating pain, and eliminating swelling. Maintaining mobility of the accessory joints (hand, wrist, elbow) is crucial within the first weeks. While passive range of motion is initiated, external rotation is intentionally limited to 30° to avoid overstressing the repair. By week 5, the sling is removed and patients are allowed full unrestricted passive motion, and they start active range of motion of the glenohumeral joint. At this time, muscular strengthening is introduced starting with isometrics and progressing to closed chain exercises. By 6 to 7 weeks postop, open chain strengthening exercises are initiated. By 4 months postop, patients are typically cleared to return to full activities.
Discussion
Arthroscopic techniques for anterior shoulder instability continue to advance. There is a vast array of suture anchor types and sizes, and therefore it is imperative that the surgeon understand both the benefits and limitations of the implants to maximize patient outcomes. This surgical technique details the use of knotless all-suture anchors. The technique described herein highlights some of the pearls and pitfalls (Table 1) of using knotless all-suture anchors for Bankart repair, with appropriate placement and capsulolabral tensioning to maximize patient benefit and limit recurrence.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Smaller drill holes allow for preservation of glenoid bone stock. | Malpositioning of the anchors, with potential damage to the glenoid cartilage. |
| Lack of rigid component and curved insertion guide allow anchor positioning at deep 5:30 position through the anteroinferior portal. | Additional portals may be needed with impairment of the subscapularis tendon (transtendon). |
| Anchor placement through the drilling/insertion guide provides simple and faster surgery and allows percutaneous insertion. | Shifting of the guide may need a second drill. |
| Approximating the tissue superiorly and medially (capsular shift) before tightening the loop provides better tensioning of the capsulolabral complex. | Inadequate tensioning of the capsulolabral tissue can lead to recurrence of glenohumeral instability. |
| Knotless, self-locking. | Knots are inconsistent, take more time, and create risk of soft tissue and cartilage abrasion. |
The main advantages of the presented technique are the small size of the anchors, which allows multiple points of fixation with minimal bone removal; the anchor material, which is both small and strong; the unique ability to tension the repair under direct visualization; and the knotless aspect of the construct. As described in this technique, using a grasper to determine and create the desired tension of the repair is an advantage. The self-locking knotless design is quickly reproducible and eliminates any risk of chondral or soft tissue abrasion from the knot stack. Furthermore, the anchors can be retensioned after subsequent anchors have been inserted to “dial in” the entire tension of the repair construct.
Appropriately retensioning the inferior capsulolabral-ligament-complex is crucial for recreating a stable glenohumeral joint and preventing of recurrent shoulder instability.10, 11, 12 Arthroscopic labral repairs can be limited by the fact that the inferior glenoid rim can be difficult to access. In some instances, clinicians have advocated for a transtendon low anteroinferior (5:30 o’clock) portal through the lower subscapularis tendon/muscle.13 The knotless all-suture anchor repair is advantageous due to a lack of a rigid component and the ability to both drill and insert the anchor through curved guides. With the use of a curved drilling and insertion guide, the glenoid rim at the 5:30 position is easily accessible via a standard anteroinferior portal without risk of impairment of the subscapularis tendon. In addition, being able to insert the anchor through a guide not only makes it easier to insert the anchor but also gives the surgeon the option to insert it percutaneously should the need arise.
The use of knotless anchors offers the advantage of a more efficient surgery and eliminates the weak link of the knot in anchor repairs for shoulder instability.14 The self-locking mechanism of the knotless all-suture anchor repair is time saving, avoids the inconsistencies of knot tying, and eliminates knot stacks and the potential issues of knot abrasion, which can cause unwanted soft tissue or cartilage damage.3 Moreover, with this design, the suture compresses and rolls up the soft tissue over the anchor and allows the surgeon the option to use either a simple or mattress stitch configuration.
With these anchors, only a 1.8-mm diameter bone tunnel is required to be drilled and bone preservation is maximized. This is one of the reasons why we prefer knotless all-suture anchors, especially in young, professional athletes who are at high risk for traumatic shoulder reinjury. Not only is this anchor useful for young patients with good-quality bone, but this anchor is also suitable and strong for older patients as well. The anchor has excellent pullout both in the lab and clinically. All-suture anchors provide the benefit of removing less bone upon insertion and occupy a less total volume of bone, yet other all-suture anchor designs have shown equivalent biomechanical properties as that of traditional solid suture anchors.15 Erickson et al.15 compared second-generation all-soft suture anchors to first-generation all-soft suture anchors as well as a traditional PEEK hard suture anchor. Their findings demonstrated equivalent biomechanical properties in terms of displacement after cyclic loading when comparing the second-generation all-soft tissue suture anchor to the hard PEEK anchor; furthermore, they showed that the second-generation anchors demonstrated improvement in the biomechanical properties compared with the first generation of all-soft tissue suture anchors.15
Clinical studies have shown that arthroscopic Bankart repair techniques that include bone preservation strategies and advanced soft tissue management have led to improved outcomes and function in patients with anterior shoulder instability.15, 16, 17 Moreover, knotless suture anchors using modern designs have shown equivalent results when compared to traditional knotted anchors.4, 18, 19, 20, 21
In conclusion, the technique described offers the benefits of bone preservation, strong fixation, time saving, and a knotless repair construct. The surgeon can use this technique both in primary and revision Bankart repairs to optimize patient outcomes and decrease the risk of recurrence of instability.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.L. receives support from Arthrex. P.J.M. is a consultant for and receives royalties from Arthrex, Medbridge, and Springer; owns stock in GameReady and VuMedi; receives support from the Steadman Philippon Research Institute and Vail Valley Medical Center; and has corporate sponsorship from the Steadman Philippon Research Institute, Smith & Nephew, Arthrex, Siemens, and Össur. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step video illustration of an arthroscopic knotless, tensionable all-suture anchor Bankart repair in a patient’s left shoulder in beach chair position. Three knotless FiberTak all-suture anchors (Arthrex) are placed at the 5:30, 4:00, and 3:30 o’clock positions to restore the capsulolabral complex.
References
- 1.Willemot L., Elfadalli R., Jaspars K.C. Radiological and clinical outcome of arthroscopic labral repair with all-suture anchors. Acta Orthop Belg. 2016;82:174–178. [PubMed] [Google Scholar]
- 2.Mazzocca A.D., Chowaniec D., Cote M.P. Biomechanical evaluation of classic solid and novel all-soft suture anchors for glenoid labral repair. Arthroscopy. 2012;28:642–648. doi: 10.1016/j.arthro.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 3.Bents E.J., Brady P.C., Adams C.R., Tokish J.M., Higgins L.D., Denard P.J. Patient-reported outcomes of knotted and knotless glenohumeral labral repairs are equivalent. Am J Orthop (Belle Mead NJ) 2017;46:279–283. [PubMed] [Google Scholar]
- 4.Thal R., Nofziger M., Bridges M., Kim J.J. Arthroscopic Bankart repair using Knotless or BioKnotless suture anchors: 2- to 7-year results. Arthroscopy. 2007;23:367–375. doi: 10.1016/j.arthro.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 5.Mook W.R., Petri M., Greenspoon J.A., Horan M.P., Dornan G.J., Millett P.J. Clinical and anatomic predictors of outcomes after the Latarjet procedure for the treatment of anterior glenohumeral instability with combined glenoid and humeral bone defects. Am J Sports Med. 2016;44:1407–1416. doi: 10.1177/0363546516634089. [DOI] [PubMed] [Google Scholar]
- 6.Martetschlager F., Kraus T.M., Hardy P., Millett P.J. Arthroscopic management of anterior shoulder instability with glenoid bone defects. Knee Surg Sports Traumatol Arthrosc. 2013;21:2867–2876. doi: 10.1007/s00167-012-2198-9. [DOI] [PubMed] [Google Scholar]
- 7.Braun S., Horan M.P., Elser F., Millett P.J. Lesions of the biceps pulley. Am J Sports Med. 2011;39:790–795. doi: 10.1177/0363546510393942. [DOI] [PubMed] [Google Scholar]
- 8.Pogorzelski J., Horan M.P., Hussain Z.B., Vap A., Fritz E.M., Millett P.J. Subpectoral biceps tenodesis for treatment of isolated type II SLAP lesions in a young and active population. Arthroscopy. 2018;34:371–376. doi: 10.1016/j.arthro.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 9.Yian E., Wang C., Millett P.J., Warner J.J. Arthroscopic repair of SLAP lesions with a bioknotless suture anchor. Arthroscopy. 2004;20:547–551. doi: 10.1016/j.arthro.2004.01.036. [DOI] [PubMed] [Google Scholar]
- 10.Randelli P., Ragone V., Carminati S., Cabitza P. Risk factors for recurrence after Bankart repair a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20:2129–2138. doi: 10.1007/s00167-012-2140-1. [DOI] [PubMed] [Google Scholar]
- 11.van der Linde J.A., van Kampen D.A., Terwee C.B., Dijksman L.M., Kleinjan G., Willems W.J. Long-term results after arthroscopic shoulder stabilization using suture anchors: An 8- to 10-year follow-up. Am J Sports Med. 2011;39:2396–2403. doi: 10.1177/0363546511415657. [DOI] [PubMed] [Google Scholar]
- 12.Lacheta L., Siebenlist S., Imhoff A.B., Willinger L. [Recurrent instability and instability arthropathy] Unfallchirurg. 2018;121:142–151. doi: 10.1007/s00113-017-0408-0. [DOI] [PubMed] [Google Scholar]
- 13.Buchmann S., Brucker P.U., Beitzel K. Long-term effects on subscapularis integrity and function following arthroscopic shoulder stabilization with a low anteroinferior (5:30 o'clock) portal. Knee Surg Sports Traumatol Arthrosc. 2016;24:422–429. doi: 10.1007/s00167-015-3545-4. [DOI] [PubMed] [Google Scholar]
- 14.Cole B., Sekiya J. Elsevier Health Sciences; London: 2013. Surgical techniques of the shoulder, elbow, and knee in sports medicine. [Google Scholar]
- 15.Erickson J., Chiarappa F., Haskel J. Biomechanical comparison of a first- and a second-generation all-soft suture glenoid anchor. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117717010. 2325967117717010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J.S., Novikov D., Kaplan D.J., Meislin R.J. Effect of additional sutures per suture anchor in arthroscopic Bankart repair: A review of single-loaded versus double-loaded suture anchors. Arthroscopy. 2016;32:1415–1420. doi: 10.1016/j.arthro.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 17.Richmond J.C., Donaldson W.R., Fu F., Harner C.D. Modification of the Bankart reconstruction with a suture anchor. Report of a new technique. Am J Sports Med. 1991;19:343–346. doi: 10.1177/036354659101900404. [DOI] [PubMed] [Google Scholar]
- 18.Hayashida K., Yoneda M., Mizuno N., Fukushima S., Nakagawa S. Arthroscopic Bankart repair with knotless suture anchor for traumatic anterior shoulder instability: Results of short-term follow-up. Arthroscopy. 2006;22:620–626. doi: 10.1016/j.arthro.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Ng D.Z., Kumar V.P. Arthroscopic Bankart repair using knot-tying versus knotless suture anchors: Is there a difference? Arthroscopy. 2014;30:422–427. doi: 10.1016/j.arthro.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Kocaoglu B., Guven O., Nalbantoglu U., Aydin N., Haklar U. No difference between knotless sutures and suture anchors in arthroscopic repair of Bankart lesions in collision athletes. Knee Surg Sports Traumatol Arthrosc. 2009;17:844–849. doi: 10.1007/s00167-009-0811-3. [DOI] [PubMed] [Google Scholar]
- 21.Thal R. Knotless suture anchor: Arthroscopic bankart repair without tying knots. Clin Orthop Relat Res. 2001;390:42–51. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step video illustration of an arthroscopic knotless, tensionable all-suture anchor Bankart repair in a patient’s left shoulder in beach chair position. Three knotless FiberTak all-suture anchors (Arthrex) are placed at the 5:30, 4:00, and 3:30 o’clock positions to restore the capsulolabral complex.