Abstract
Objective:
To investigate if food insecurity affects child body mass index (BMI) through parental feeding demandingness and/or responsiveness and dietary quality 18 months later among low-income Hispanic preschoolers.
Design:
Secondary analysis of data at baseline and 18 months post-baseline.
Setting:
Houston, Texas.
Participants:
Hispanic parent-preschooler dyads (n=137).
Variables:
Food insecurity (6-item Household Food Security Survey), child BMI (BMI z-score), child dietary quality (Healthy Eating Index), parental feeding demandingness and responsiveness (Caregiver’s Feeding Style Questionnaire).
Analysis:
Ordinary least squares regression models and 95% bootstrapped confidence interval to estimate effects.
Results:
Controlling for baseline child BMI, maternal acculturation, and maternal BMI, total indirect effect of food insecurity on child BMI through feeding demandingness, responsiveness, and subsequent child dietary quality were estimated to be 0.00, 95% bias-controlled bootstrap CI [−0.01, 0.01]). Confidence intervals for all indirect pathways straddled zero. As food insecurity worsened, child dietary quality 18-months post-baseline improved (c= 1.06, 95% CI [0.41, 1.71]).
Conclusions and Implications:
Food insecurity had no influence on child BMI through feeding demandingness/responsiveness and/or child dietary quality. Additional research is needed to examine why food insecurity had a “protective” effect on dietary quality 18-months later. This finding suggests adoption of coping mechanisms.
Keywords: Food insecurity, Food security, Child obesity, Parenting, Dietary quality, Feeding style
INTRODUCTION
In 2017, nearly a quarter of Hispanic children lived in food insecure homes.1 Additionally, between 2013-2016, 16.5% of Hispanic children aged 2 through 5 and 25.3% of 6 through 11 year olds were obese.2 In comparison, the prevalence of obesity among non-Hispanic white children in the same time period was 9.9% for 2 through 5 year olds and 14.0% for 6 through 11 year olds.2 This suggests that Hispanic preschoolers are disproportionately at risk for food insecurity and obesity. Food insecurity is the lack of access to food because of restricted financial resources.1 Although the direct relationship between food insecurity and child obesity remains unclear, both issues co-exist.3,4 One possible pathway linking the issues is poor dietary quality. Individuals living in food insecure households may consume lower-cost, energy-dense foods that have low nutritional value but are readily accessible and affordable.5-9 Over time, this type of diet may contribute to excess body mass (i.e., overweight/obesity). Several studies that examined dietary intake in Hispanic children at risk for food insecurity found that their dietary quality was less likely to meet dietary recommendations compared to children with increased food security.8-10
Parents struggling with food insecurity may also develop behaviors that contribute to increased child body mass index (BMI).11 The Family Stress Model supports this idea.12 It proposes that economic hardships affect outcomes in children indirectly through parenting behaviors. Economic hardships are difficulties resulting from a lack of money or other resources.13 Therefore, food insecurity- a lack of access to food due to financial limitations- is a form of economic hardship which could affect parental feeding behaviors. Indeed, studies that examined parental feeding practices found that food insecure parents from diverse racial/ethnic backgrounds restricted the types of food their children consumed11,14 or pressured their child to eat.15,16 These types of parenting feeding behaviors are associated with increased child BMI.17
Feeding style is another parenting behavior associated with dietary intake and BMI.18 Feeding style describes the emotional climate in which parents feed their children and is measured on two scales: demandingness and responsiveness.18 Demandingness refers to the amount of control a parent expresses when feeding his/her child. Responsiveness refers to the amount of warmth with which a parent expresses that demandingness. Generally, parents with increased stress reflected feeding styles that were low in demandingness and responsiveness.18,19 However, Hispanic parents tend to exhibit low demandingness and high responsiveness.20 Children whose parents reported low demandingness with either low or high responsiveness generally had nutritionally poor diets21 and elevated BMIs.22
To the extent known, no study has examined food insecurity’s influence on child’s BMI through parental feeding style or child’s dietary quality. To test these potential mediators, the investigators used data that was initially collected as part of a larger study funded by the National Institute of Child Health and Human Development (HD062567). The parent study was designed to examine the development of eating and general self-regulation in children starting in preschool and their influence on child BMI after 18 months.23,24
The current study aims to examine the indirect effects of food insecurity on child BMI after 18 months through levels of parental feeding demandingness and responsiveness and subsequent quality of child’s diet among low-income Hispanic preschoolers. The investigators hypothesized that feeding demandingness and responsiveness would contribute to poor dietary quality and elevated BMI in low-income Hispanic preschoolers. (Because feeding responsiveness appears to be low in stressed parents18,19 but high in Hispanic parents20, they could not hypothesize which direction feeding responsiveness would follow in food insecure Hispanic parents. However, they suspect that feeding demandingness will increase.)
METHODS
Study Design, Participants, and Recruitment
The current study used data that was collected at baseline (Time 1) and 18 months post-baseline (Time 2) from an observational study (HD06257, PI: Hughes). Data collection began in August 2011 at the USDA/ARS Children’s Nutrition Research Center (CNRC) in Houston, TX.
At Time 1, researchers collected data from 187 self-identified Hispanic parent-child dyads. At Time 2, 144 parent-child dyads returned for data collection. The nonprobability sample was recruited through Head Start Centers located in Houston, TX through fliers and parent information meetings. Only one child and parent per family were recruited. At the time of recruitment, household income for children enrolled in Texas Head Start needed to be ≤ $22,350 before tax for a family of four.25
Sample selection criteria for the parent study included children being between four and five years of age at time of recruitment. If a family had more than one child that met inclusion criteria, the parent was instructed to select a child to participate in the study. Adults had to be the primary caregiver of the child when child was not at school. Because children would be eating food prepared at the research center, children with food allergies were excluded. Children who were unable to serve themselves or eat without assistance were also excluded.
Institutional Review Board
The current study underwent an expedited review and was approved through the Committee of the Protection of Human Subjects at the University of Texas Health Science Center. The parent study (HD06257, PI: Hughes) had Institutional Review Board approval from Baylor College of Medicine and participants provided written consent.
Measurements and Instruments
Food insecurity.
Food insecurity was measured using a 5-item, self-administered, paper version of the 6-item Household Food Security Survey (6-item HFSS).26 Questions AD1 and AD1a were consolidated as per the instrument’s user notes.26 The questions are a subset of the standard 18 items asked in the U.S. Household Food Security Survey Module and focus on household and adult food security. This instrument has robust evidence of reliability and validity.27,28 Individuals respond to the questions by indicating the frequency of an event (i.e., often true/sometimes true/never true or yes, almost every month/ yes, some months but not every month/ yes, only 1 or 2 months, no) or whether they have or have not (i.e., yes/no) experienced an event. The raw food security status score was calculated by summing the number of affirmative responses as per the 6-item HFSS’s user notes.26 For descriptive purposes, the raw score was categorized into: high/marginal food security (raw score = 0 or 1), low food security (raw score = 2-4), and very low food security (raw score = 5-6). The raw score was then converted to an interval-level scale score (range 0 to 8.48) per the instrument’s user notes.26 Higher scores indicate greater food insecurity.
Levels of parental feeding demandingness and responsiveness.
The Caregiver’s Feeding Styles Questionnaire (CFSQ)18 operationalized feeding demandingness and responsiveness. For a copy of the instrument, please contact second author. This instrument was specifically designed to assess feeding in low-income minority populations in the US- namely African Americans and Hispanics- and has demonstrated convergent and predictive validity.18 Cronbach’s alpha in this sample for child-centered (used to calculate responsiveness) and parent-centered feeding were .67 and .84, respectively.29
The instrument consists of 19 items with 5-point Likert-scale responses (never/rarely/sometimes/most of the time/always). Demandingness was determined by averaging the responses for all 19 items and ranged from one to five.18 Higher scores represent greater control by parents with respect to their child’s feeding/eating. Responsiveness scores were calculated by dividing the mean of seven child-centered questions (#3, 4, 6, 8, 9, 15, and 17) by the overall average score of all 19 items.18 Child-centered questions assessed promotion of child autonomy (e.g., reasoning, complimenting, and helping the child to eat).18 Scores ranged between 0.20 and 2.02 with higher scores representing greater parental responsiveness.
Feeding demandingness and responsiveness have cutoff points that are used to categorize parents into one of four specific feeding styles.30 However, in the current study, feeding demandingness and responsiveness were intentionally kept as distinct, continuous variables to identify changes or trends that may have been too small to be identified if categorical feeding styles were used.
Dietary quality.
Dietary quality was measured using the Healthy Eating Index 2015 (HEI).31 Total scores ranged from 0 to 100. Higher scores reflect greater adherence to the Dietary Guidelines for Americans.31 The developers evaluated the HEI for construct validity, criterion validity, and reliability.32
Children’s HEI scores at baseline and 18-months post-baseline were calculated from three 24-hour dietary recalls. The first dietary recall was completed in-person. Subsequent recalls were collected over the phone. Participating parents were called randomly over a two-week period to complete three dietary recalls (two weekdays, one weekend day) for their preschool child. Information regarding meals consumed at Head Start were collected from the child’s teacher. Trained staff used a standard script that included the 5-step multipass method33 and entered dietary data following the scripts provided in the Nutrition Data System for Research Software (NDSR) versions 2012 (Time 1) and 2014 (Time 2).
Each participant’s food group or nutrient intake was averaged across the three recalls collected per timepoint using the method described by Guenther.34 These averages were then used to calculate the 13 HEI component scores and final score per NDSR35 and the Epidemiology and Genomics Research Program guidelines.31
Maternal and Child body mass index.
Trained CNRC staff members took two measurements of each participant’s height and weight using a standard protocol.36 A stadiometer and an electronic self-calibrating digital scale were used to take the measurements. Participants wore light clothing and removed their shoes. Trained research assistants measured each participants’ height to the nearest 0.1 cm and weight to the nearest 0.1 kg twice. Each participant’s averaged height and weight were used to generate BMI scores for parents and age and gender specific BMI z-scores for children based on the Centers for Disease Control and Prevention Reference Standards.37
Acculturation.
Parental acculturation, a covariate to dietary quality and child body mass, was measured using the Bidimensional Acculturation Scale.38 This 24-item, 4-point Likert scale questionnaire consists of a Hispanic domain (12 items) and English domain (12 items). Hispanic and English acculturation scores were calculated by averaging responses to each of the 12 items in the respective domain.38 Each domain’s final score ranged between one and four. In this sample, the Cronbach’s alpha were .92 (Spanish domain) and .97 (English domain).29 Convergence validity with generation, age at arrival, residence in US, education, and self-identification ranged from .46 to .86 for the English domain and −.28 to −.66 for the Hispanic domain.38
Data Collection Procedures
Data collection at Time 1 and Time 2 followed the same protocols. All data except for two of the three food recalls at each time point were completed at the CNRC lab. Trained CNRC staff members who were fluent in Spanish and English obtained data from participants in the language of the participant’s choice. All surveys, including the 6-item HFSS and CFSQ, were given to parents for completion in random order.
Statistical Analysis
Data was analyzed using IBM Statistical Program for the Social Sciences (SPSS) version 25. Descriptive statistics examined the distributions and variability for food security status (FSS), child BMI z-score (BMIz), child dietary quality (HEI), parental feeding demandingness (PFD), parental feeding responsiveness (PFR), and demographics at both time points. Independent T-tests and Chi-square analyses were used to compare for differences in FSS, HEI, PFD, PFR, BMIz, and demographics between participants who returned for Time 2 data collection with those who did not return. Paired T-tests and Chi-square analyses (McNemar-Bowker Test) were used to detect changes between Time 1 and Time 2 among returning participants. Statistical significance was set at a p-value of ≤ 0.05.
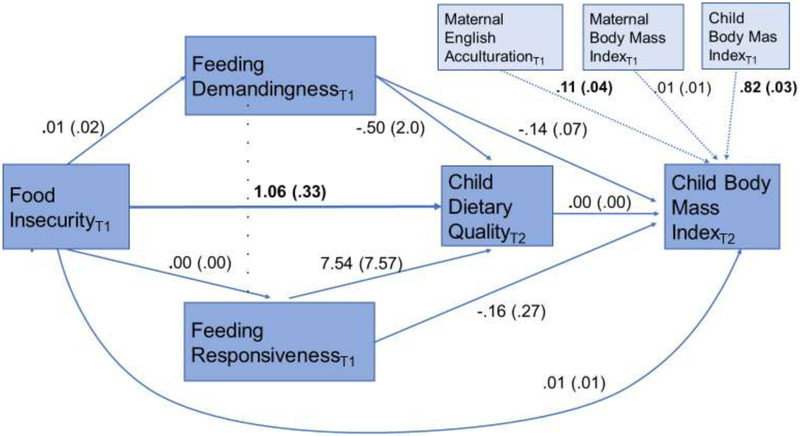
A cross-lagged panel model approach39 was used to assess direct and indirect effects using data collected at two timepoints. A single model was used to compute the direct and indirect effects of food insecurity at baseline on child BMIz 18 months post-baseline first through its effects on feeding demandingness and feeding responsiveness at baseline (parallel mediators) and then through feeding demandingness and responsiveness’s impact on child dietary quality 18 months post-baseline. Please refer to Figure 1 to view the pathways being tested in this model.
Figure 1.
Direct and Indirect pathways between Food Insecurity and Child Body Mass Index through Feeding Demandingness and Responsiveness and Child Dietary Quality. Co-variates included. Subscript indicates timepoint at which given measure was obtained. Pathways labeled with unstandardized coefficient (standard error). Coefficients in bold indicate 95% confidence interval did not contain zero.
Direct and indirect effect estimates were calculated using PROCESS40, a SPSS macro that uses ordinary least squares regression path analysis. PROCESS calculated a 95% confidence interval for the direct effect and 95% bias-corrected bootstrapped confidence interval using 10,000 repetitions for the indirect effect. If confidence intervals contained zero, the effect was not significant.
Covariates included: child gender, number of household members and children, parental Hispanic and English acculturation, marital status, parental employment status, parental education level, and parental BMI. After testing each co-variate for significance in the models, English acculturation and parental BMI were the only significant co-variates. To be consistent with the cross-lagged panel model approach, the model controlled for the child BMIz at Time 1. Steps used to identify significant co-variates are available on request.
RESULTS
Sample Characteristics
At Time 1, 187 parent-child dyads participated. At Time 2, 137 returning dyads had a measure for FSS, child BMIz, and child HEI. However, because of additional missing data, the analytic sample for the mediation model was 126. All but two adult participants were mothers. The remaining two were grandmothers. Girls accounted for 47.8% of child participants. At Time 1 and 2 the average age of children was 4.8 and 6.3 years, respectively. The median number of household members was five and the median number of children per household was three. At Time 1, 46% of participant households had some level of food insecurity (low or very low). Table 1 lists additional sample characteristics for both time points. At Time 1 and 2, HEI, BMIz, PFD, and PFR had normal distributions.
Table 1.
Characteristics of participants who had food security score, child dietary quality, & child body mass index scores at both timepoints (n=137)
| Baseline | 18 months post-baseline | ||||
|---|---|---|---|---|---|
| Characteristic | Levels | n or mean | % or SD | n or mean | % or SD |
| Household Food Security Status | High or marginal food security | 74 | 54.0% | 88 | 64.3% |
| Low food security | 39 | 28.5% | 28 | 20.4% | |
| Very low food security | 24 | 17.5% | 21 | 15.3% | |
| Child’s Healthy Eating Index-2015 | Potential Range (0-100) | 60.51 | 9.47 | 61.98 | 11.82 |
| Child’s Body Mass Index Categories | Underweight (< 5th Percentile) | 1 | 0.7% | 1 | 0.7% |
| Normal (5th < 85thPercentile) | 67 | 48.9% | 69 | 50.4% | |
| Overweight (85th < 95th Percentile) | 29 | 21.2% | 30 | 21.9% | |
| Obese (≥ 95th Percentile) | 40 | 29.2% | 37 | 27.0% | |
| Parenting Feeding Demandingness | Potential Range (1-5) | 3.07 | 0.59 | 2.80 | 0.62 |
| Parenting Feeding Responsiveness | Potential Range (0.20-2.02) | 1.22 | 0.17 | 1.25 | 0.18 |
| Maternal Hispanic Acculturation | Potential Range (1-4) | 3.64 | 0.51 | 3.60 | 0.51 |
| Maternal English Acculturation | Potential Range (1-4) | 2.20 | 0.88 | 2.33 | 0.87 |
| Maternal Marital Status | Married | 78 | 56.9% | 76 | 55.5% |
| Never married | 18 | 13.1% | 23 | 16.8% | |
| Divorced/Separated/Widowed | 23 | 16.8% | 24 | 17.5% | |
| Other* | 18 | 13.1% | 14 | 10.2% | |
| Maternal Education Status | Some high school or less | 53 | 38.7% | 52 | 37.9% |
| High school/GED | 33 | 24.1% | 38 | 27.7% | |
| Technical school/ Some college | 44 | 32.1% | 37 | 27.0% | |
| College graduate | 7 | 5.1% | 10 | 7.3% | |
| Maternal Employment | Employed | 32 | 23.4% | 44 | 32.1% |
| Unemployed | 105 | 76.6% | 93 | 67.9% | |
| Maternal Body Mass Index | Healthy range 18.5 – 24.9 | 31.90 | 7.20 | 31.81 | 7.20 |
Most common response to “other” marital status was ‘union libre’ which is living together without being legally married.
Group Comparisons
There were no statistically significant differences in FSS, HEI, PFD, PFR, BMIz, household size and number of children, maternal marital/employment/education status between the participants who returned for Time 2 data collection and those who did not return. However, the returning group scored higher in Hispanic acculturation (M = 3.64, SD = 0.51) compared to the non-returning group (M = 3.44, SD = 0.66) (t (167) = 2.02, p = 0.05). The returning group also had lower English acculturation (M = 2.20, SD = 0.88) compared to the non-returning group (M = 2.53, SD = 0.96) (t (167) = −2.07, p = .04).
Paired t-test comparisons between just those 137 participants who had a score for FSS, child HEI, and child BMIz at Time 2 indicate no significant change over the 18 months for these three variables. However, PFD decreased between Time 1 (M = 3.07, SD = 0.59) and Time 2 (M = 2.80, SD = 0.62) (t (132) = 6.10, p = .00) while PFR increased between Time 1 and Time 2 (Mdifference = 0.03, SD = 0.16) (t (132) = −2.35, p = .02). English acculturation (Mdifference = 0.07, SD = 0.32) (t (122) = −2.44, p = .016) also increased, although Hispanic acculturation levels remained stable (Mdifference = .01, SD = .34) (t (121) = .22, p = .83). Employment increased by 8.7% between the time points.
Direct and Indirect Effects of Food Insecurity on Child BMI
Findings did not support the hypothesis that food insecurity would over time indirectly affect child’s BMI through feeding demandingness and responsiveness and subsequent dietary quality. The total indirect effect of FSS at Time 1 on child BMIz at Time 2 was not statistically different from zero (total indirect effect = 0.00, 95% bias-controlled bootstrap CI [−0.01, 0.01]). Each of the five indirect pathways between FSS at Time 1 and child BMIz at Time 2 included zero in the 95% bias-controlled bootstrap confidence interval based on 10,000 iterations. The direct pathways in Figure 1 are labeled with unstandardized coefficients.
Because of concerns regarding the time needed to see effects unfold between food insecurity and feeding demandingness and responsiveness, we tested a similar mediation model changing PFD and PFR to their values at Time 2. The total indirect effect was 0.00 (95% bias-controlled bootstrap CI [−0.01, 0.01]). The direct and indirect effects also straddled zero. A table with the indirect effects and a path analysis model with unstandardized coefficients for this model are available on request.
Additional Findings
The path between FSS at Time 1 and child HEI at Time 2 was significant (β = 1.06, 95% CI [0.41, 1.71], p = .002). A regression model to test the effect of FSS at Time 1 on child HEI at Time 2 while controlling for English acculturation and child HEI at Time 1, revealed that FSS at Time 1 explained 8.5% of the variance for child HEI at Time 2. However, a cross-sectional regression model that examined the effect of FSS at Time 1 on child HEI at Time 1 while controlling for maternal English acculturation at Time 1 found no significant association between the variables (β = −0.05, 95% CI [−0.53, 0.43], p = .825). A similar cross-sectional regression model examining the effect of FSS at Time 2 on child HEI at Time 2 while controlling for maternal English acculturation at Time 2 and child dietary quality at Time 1 also found no significant association between the variables (β = 0.27, 95% CI [−0.40, 0.94], p = .430)
Because more families at Time 2 were food secure compared to Time 1, a mediation model was used to test if the association between FSS at Time 1 and child dietary quality at Time 2 could be explained by a mediating effect of FSS at Time 2. The independent variable was FSS at Time 1, the dependent variable was child dietary quality at Time 2, and the mediating variable was FSS at Time 2. We controlled for maternal acculturation, child dietary quality, and maternal dietary quality all at Time 1. As reported earlier, there was a direct association between FSS at Time 1 and child dietary quality at Time 2 (c’=1.07, 95% CI [0.26, 1.87], p = .010). However, FSS at Time 2 did not mediate the relationship between FSS at Time 1 and child dietary quality at Time 2 (ab = −0.09, 95% bootstrapped CI [−0.49, 0.32].
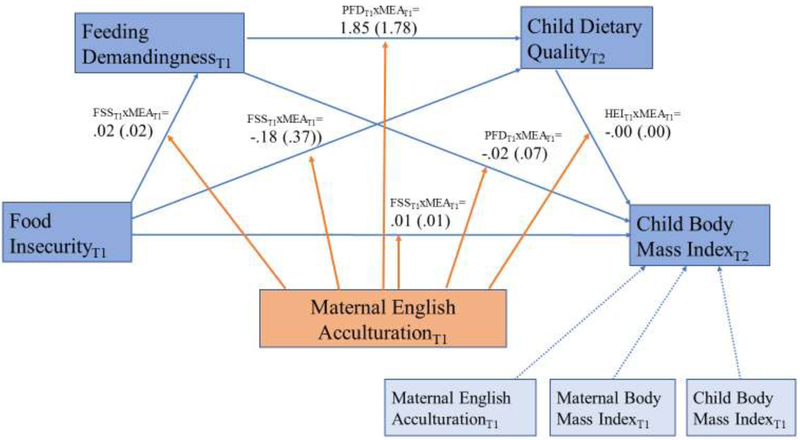
Because maternal English acculturation at Time 1 was a significant co-variate for all three mediators listed in Figure 1 and child BMI at Time 2, analysis was performed to investigate if the level of acculturation interacted with food insecurity at Time 1, feeding demandingness or responsiveness at Time 1, and child dietary quality at Time 2. Using the model depicted in Figures 2, investigators found that the level of maternal English acculturation did not have any significant conditional effect on the direct or indirect pathways between food insecurity at Time 1 and child BMI at Time 2. A separate model in which feeding responsiveness replaces feeding demandingness as the first mediator also found that maternal English acculturation had no significant conditional effect. This second model is available on request.
Figure 2.
Moderation by Maternal English Acculturation at Time 1. Subscript indicates timepoint at which given measure was obtained. Unstandardized coefficients (standard error) of the interaction terms are labeled in model. No significant interaction terms to report. Key to abbreviations: MEA= Maternal English Acculturation, FSS = Food Insecurity, PFD= Feeding Demandingness, HEI= Dietary Quality.
DISCUSSION
The purpose of this study was to examine the effects of food insecurity on child’s body mass index through a complex series of pathways that involve parental feeding demandingness and responsiveness, and child dietary quality. No significant paths between baseline food insecurity and child’s body mass index 18 months later were identified. Unexpectedly, exposure to household food insecurity had a protective effect on child’s dietary quality 18 months later.
Because this was the first study to test the relationship between food insecurity and child BMI through feeding demandingness and responsiveness and child dietary quality, there are no direct comparisons with other studies. However, other research on parenting practices and food insecurity may explain why the hypothesis did not hold.
Parenting practices refer to behaviors used by parents to accomplish specific, short-term feeding goals.41 Just as generations ago parents may have developed controlling feeding practices as a means of protecting their child from threats of food scarcity42, current-day parents living with food insecurity report controlling parenting practices such as pressuring a child to eat.11,15 In contrast, feeding style is conceptualized as a stable behavior that describes the emotional climate in which a parent feeds their child.18 Because food insecurity is often cyclical or episodic43, intermittent food insecurity may influence short-term feeding practices. However, it may not exist long enough to illicit significant change on stable behaviors such as feeding style.
A possible explanation for the lack of association between food insecurity and BMI through dietary quality in low-income Hispanic preschoolers may be that mothers protect children from the effects of food insecurity.7,44 Also, Head Start may have buffered the effects of food insecurity because of increased access to food assistance programs such as the Supplemental Nutrition Assistance Program and the Special Supplemental Nutrition Program for Women, Infants, and Children.45 Head Start also offers nutrition education to parents.45,46 The children in this study had graduated out of Head Start by Time 2 and any effects that could relate to Head Start would be residual. However, the children could still have received free or reduced-cost breakfast and/or lunch at their current schools.
Unexpectedly, lower baseline household food security was associated with higher dietary quality 18 months later. This relationship does not appear to be explained by the increase in food security at Time 2 as indicated by the lack of mediation in the model shared in the “additional findings” section. Most studies that examined the relationship between food security and diet found: (1) low food security was associated with low dietary quality9,47,48 or (2) no association between food security and diet.49-51 However, there is one longitudinal study that examined the relationship between food insecurity and diet and found that children who had experienced food insecurity consumed more fruits and vegetables compared to food secure children.52
These unexpected relationships between food insecurity and diet when viewed over a span of time call for the need for additional investigation using longitudinal methods that purposefully evaluate pathways and mechanisms between food insecurity and diet.52,53 In the current study, the investigators can only speculate the changes that occurred. For example, the families may have enrolled in a food assistance program, used food pantries, and/or implemented the nutrition education they received while their children were in Head Start. They may have also adopted other coping strategies that we need to recognize. Research examining the influence of food insecurity on each of the dietary components that constitute the Healthy Eating Index may provide additional clues to explain this unexpected relationship and should be examined in future research.
Limitations and Strengths
There are several limitations to this study worth noting. Low-income Hispanic families who choose not to enroll their children in Head Start programs are not represented in this sample and findings may not be generalizable to them. In addition, the parents’ responses on the 6-item HFSS and CFSQ are subject to self-report bias. The HEI is also dependent on accurate recall of the child’s dietary intake as reported by the parents. Additionally, household participation in food assistance programs or differences in child autonomy between ages 4-5 and 5.5-6.5 could not be controlled. Finally, it is unclear if the time lag of 18 months is appropriate to test for effects of food security status on child dietary quality and BMI. Other studies examining the same variables have used time lags of 6 months54,55, 12 months47, and 24 months.56
Having two timepoints to test indirect effects is a primary strength of the current study. This design allows for control of prior levels of the dependent variable which subsequently reduces possible over-inflation of estimates. It also allows for the effects to unfold over time.57 For these reasons, data with two time-points enables testing of indirect effects with greater rigor compared to cross-sectional design.39,57 Additionally, by using bias-corrected bootstrap method to estimate indirect effects, the current analytic sample size of 126 is adequate to detect medium to large effects.58 These effect sizes would be considered clinically significant.
IMPLICACTIONS FOR RESEARCH AND PRACTICE
The relationships tested in this study were complex. The lack of association between most of them indicates that there may be other factors in play that have yet to be identified. Future research examining the relationships between food insecurity, dietary quality, and body mass index in low-income populations should consider using a mixed-method approach. Qualitative data would provide the context needed to further understand quantitative findings-particularly when the hypothesis is not supported. For example, in this study, child dietary quality had no statistical association with child BMI. If qualitative data were available, it may have been able to help identify explanations for the lack of this logical association.
Additionally, the directionality of the association between baseline food insecurity and child dietary quality a year and half later was unexpected. There was no significant relationship between food insecurity and dietary quality when examined cross-sectionally at either baseline or 18 months later which suggests that the effect of food insecurity takes time to unfold. Further investigation on the long-term impact of early exposure to food insecurity on children and their parents is needed.
Furthermore, the current operationalization of food insecurity focuses on financial limitations for access to food. However, other factors, such as limited time, transportation, and nutritional literacy, may also be barriers to healthy foods for low-income families. A comprehensive measure of food insecurity is needed.
The current operationalization of food insecurity also does not allow for differentiation between episodic and chronic food insecurity. Because these two types of food insecurity may have different effects on factors such as diet, parenting behaviors, and body mass index, additional research needs to be directed at discerning episodic from chronic food insecurity.
Although there was no evidence to support the relationship between food insecurity and child body mass index, investigators need to continue exploring environmental or behavioral factors that may bridge this gap. Further exploration on these topics is needed to help find innovative paths to reduce the prevalence of child obesity in a young, vulnerable, and rapidly-expanding population.
Practice Points.
Further investigation on the long-term impact of early exposure to food insecurity on children and their parents is needed. (character count with spacing = 126, location line 327)
Additional research needs to be directed at discerning episodic from chronic food insecurity. (character count with spacing = 96, location line 337)
Acknowledgments
This research was supported in part by the National Institute of Child Health and Human Development (R01 HD062567) and the Robert Wood Johnson Future of Nursing Scholars Program. Acknowledgements to Kirstin Vollrath, RD for assistance on calculating the Healthy Eating Index score; Nilda Micheli Correa; & Maria Papaioannou for your assistance with data access. Anita Garodnick for reviewing the manuscript. This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Footnotes
There are no known conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Statistical supplement to household food security in the United States in 2017. 2018;AP-079. [Google Scholar]
- 2.Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. 2018; 319:2410–2418. doi: 10.1001/jama.2018.5158. PubMed PMID: 29922826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson NI, Story MT. Food insecurity and weight status among U.S. children and families: A review of the literature. Am J Prev Med. 2011;40:166–173. [DOI] [PubMed] [Google Scholar]
- 4.Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obesity Reviews. 2011;12:e73–e83. [DOI] [PubMed] [Google Scholar]
- 5.Drewnowski A, Specter SE. Poverty and obesity: The role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. [DOI] [PubMed] [Google Scholar]
- 6.Frongillo EA, Bernal J. Understanding the coexistence of food insecurity and obesity. Current Pediatrics Reports. 2014;2:284–290. [Google Scholar]
- 7.Hanson KL, Connor LM Food insecurity and dietary quality in US adults and children: A systematic review. Am J Clin Nutr. 2014;100:684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- 8.Quandt SA, Trejo G, Suerken CK, Pulgar CA, Ip EH, Arcury TA. Diet quality among preschool-age children of Latino migrant and seasonal farmworkers in the United States. Journal of Immigrant and Minority Health. 2016;18:505–512. doi: 10.1007/s10903-015-0304-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaiser LL, Lamp CL, Johns MC, Sutherlin JM, Harwood JO, Melgar-Quinonez HR. Food security and nutritional outcomes of preschool-age Mexican-American children. J Am Diet Assoc. 2002;102:924–929. [DOI] [PubMed] [Google Scholar]
- 10.Sharkey JR, Nalty C, Johnson CM, Dean WR. Children's very low food security is associated with increased dietary intakes in energy, fat, and added sugar among Mexican-origin children (6-11 y) in Texas border colonias. BMC pediatrics. 2012;12:16–16. doi: 10.1186/1471-2431-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Darling KE, Fahrenkamp AJ, Ruzicka EB, Sato AF Controlling feeding practices mediate the association between food insecurity and parent-reported child BMI percentile. Child Health Care. 2017:1–14. doi: 10.1080/02739615.2017.1337517. [DOI] [Google Scholar]
- 12.Conger RD, Donnellan MB. An interactionist perspective on the socioeconomic context of human development. Annu Rev Psychol. 2007;58:175–199. doi: 10.1146/annurev.psych.58.110405.085551. [DOI] [PubMed] [Google Scholar]
- 13.Conger RD. The effects of poverty and economic hardship across generations. Davis: Center for Public Policy Research, University of California, Davis; 2005. [Google Scholar]
- 14.Kral TVE, Chittams J, Moore RH. Relationship between food insecurity, child weight status, and parent-reported child eating and snacking behaviors. J Spec Pediatr Nnrs. 2017;22:e12177. doi: 10.1111/jspn.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conlon BA, McGinn AP, Lounsbury DW, et al. The role of parenting practices in the home environment among underserved youth. Child Obes. 2015;11:394–405. doi: 10.1089/chi.2014.0093 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feinberg E, Kavanagh PL, Young RL, Prudent N. Food insecurity and compensatory feeding practices among urban black families. Pediatrics. 2008;122:e854–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obes Res. 2004; 12:1711–1722. [DOI] [PubMed] [Google Scholar]
- 18.Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: Parenting styles in a child-feeding context. Appetite. 2005;44:83–92. [DOI] [PubMed] [Google Scholar]
- 19.Hurley KM, Black MM, Papas MA, Caulfield LE, Caufield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. J Nntr. 2008;138:799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes SO, Power TG, O’Connor TM, Orlet Fisher J, Chen T. Maternal feeding styles and food parenting practices as predictors of longitudinal changes in weight status in Hispanic preschoolers from low-income families. Journal of Obesity. 2016;2016:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoerr SL, Hughes SO, Fisher JO, Nicklas TA, Liu Y, Shewchuk RM. Associations among parental feeding styles and children's food intake in families with limited incomes. Int J Behav Nutr Phys Act. 2009;6:55–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes SO, Shewchuk RM, Baskin ML, Nicklas TA, Qu H. Indulgent feeding style and children's weight status in preschool. J Dev Behav Pediatr. 2008;29:403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes SO, Power TG, O'Connor TM, Fisher JO. Executive functioning, emotion regulation, eating self-regulation, and weight status in low-income preschool children: How do they relate? Appetite. 2015;89:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Power TG, Olivera YA, Hill RA, et al. Emotion regulation strategies and childhood obesity in high risk preschoolers. Appetite. 2016;107:623–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sebelius K 2011 poverty guidelines, federal register notice. https://aspe.hhs.gov/2011-poverty-guidelines-federal-register-notice Updated 2011. Accessed January 17, 2019.
- 26.Economic Research Service. U.S. household food security survey module: Six-item short form. https://www.ers.usda.gov/media/8282/short2012.pdf Updated 2012. Accessed July 12, 2018.
- 27.Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health. 1999;89:1231–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrison GG, Stormer A, Herman DR, Winham DM. Development of a Spanish-language version of the U.S. Household Food Security Survey Module. J Nutr. 2003;133:1192–1197. [DOI] [PubMed] [Google Scholar]
- 29.Power TG, O'Connor TM, Orlet Fisher J, Hughes SO. Obesity risk in children: The role of acculturation in the feeding practices and styles of low-income Hispanic families. Childhood Obesity. 2015;11:715–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hughes SO, Cross MB, Hennessy E, Tovar A, Economos CD, Power TG. Caregiver's feeding styles questionnaire: Establishing cutoff points. Appetite. 2012;58:393–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Epidemiology and Genomics Research Program. Developing the healthy eating index. https://epi.grants.cancer.gov/hei/developing.html Updated February 12, 2018. Accessed July 5, 2018
- 32.Reedy J, Lerman JL, Krebs-Smith SM, Kirkpatrick SI, Pannucci TE, Wilson MM, Subar AF, Kahle LL, Tooze JA. Evaluation of the Healthy Eating Index-2015. J Acady Nutr Diet. 2018;118:1622–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77:1171–1178. [DOI] [PubMed] [Google Scholar]
- 34.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nutrition Coordination Center, University of Minnesota. Guide to creating variables needed to calculate scores for each component of the Healthy Eating Index-2015 (HEI-2015). http://www.ncc.umn.edu/healthy-eating-index-hei/. Accessed July 7, 2018.
- 36.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign: Human kinetics books; 1988. [Google Scholar]
- 37.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002;(246):1–190. http://www.ncbi.nlm.nih.gov/pubmed/12043359. Accessed January 25, 2019. [PubMed] [Google Scholar]
- 38.Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: The Bidimensional Acculturation Scale for Hispanics (BAS). Hispanic Journal of Behavioral Sciences. 1996;18:297–316. [Google Scholar]
- 39.Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112:558–577. [DOI] [PubMed] [Google Scholar]
- 40.Hayes A Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression Based Approach. 2nd ed. New York: Guilford Press; 2018. [Google Scholar]
- 41.Shloim N, Edelson LR, Martin N, Hetherington MM. Parenting Styles, Feeding Styles, Feeding Practices, and Weight Status in 4–12 Year-Old Children: A Systematic Review of the Literature. Front Psychol. 2015;6:1849. doi: 10.3389/fpsyg.2015.01849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: Conception to adolescence. The Journal of Law, Medicine & Ethics. 2007;35:22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Panel to Review U.S Department of Agriculture's Measurement of Food Insecurity and Hunger. Food insecurity and Hunger in the United States: An Assessment of the Measure. Washington, D.C.: National Academies Press; 2006. [Google Scholar]
- 44.Nalty CC, Sharkey JR, Dean WR. Children's reporting of food insecurity in predominately food insecure households in Texas border colonias. Nutr J. 2013;12:15. doi: 10.1186/1475-2891-12-15 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gooze RA, Hughes CC, Finkelstein DM, Whitaker RC. Reaching staff, parents, and community partners to prevent childhood obesity in Head Start, 2008. Prev Chronic Dis. 2010;7(3):A54 http://www.ncbi.nlm.nih.gov/pubmed/20394693. Accessed January 7, 2019. [PMC free article] [PubMed] [Google Scholar]
- 46.Lee R, Zhai F, Han W, Brooks-Gunn J, Waldfogel J. Head start and children's nutrition, weight, and health care receipt. Early Childhood Research Quarterly. 2013;28:723–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jansen EC, Kasper N, Lumeng JC, et al. Changes in household food insecurity are related to changes in BMI and diet quality among Michigan head start preschoolers in a sex-specific manner. Soc Sci Med. 2017;181:168–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nackers LM, Appelhans BM Food insecurity is linked to a food environment promoting obesity in households with children. J Nutr Educ Behav. 2013;45(6):780–784. doi: 10.1016/j.jneb.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 49.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23:839–862. [DOI] [PubMed] [Google Scholar]
- 50.Knol LL, Haughton B, Fitzhugh EC. Food insufficiency is not related to the overall variety of foods consumed by young children in low-income families. J Am Diet Assoc. 2004;104:640–644. doi: 10.1016/j.jada.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 51.Trapp CM, Burke G, Gorin AA, et al. The relationship between dietary patterns, body mass index percentile, and household food security in young urban children. Child Obes. 2015;11:148–155. doi: 10.1089/chi.2014.0105. [DOI] [PubMed] [Google Scholar]
- 52.Howard FF. Food Insecurity Experiences Predict Children’s Fruit and Vegetable Consumption in the USA. ISRN Nutr. 2013; 426029. doi: 10.5402/2013/426029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morales ME, Berkowitz SA. The Relationship between Food Insecurity, Dietary Patterns, and Obesity. Curr Nutr Rep. 2016;5(1):54–60. doi: 10.1007/s13668-016-0153-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Metallinos-Katsaras E, Must A, Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutri Diet. 2012;112:1949–1958. doi: 10.1016/j.jand.2012.08.031. [DOI] [PubMed] [Google Scholar]
- 55.Rose D, Bodor JN. Household food insecurity and overweight status in young school children: Results from the Early Childhood Longitudinal Study. Pediatrics. 2006;117:464–473. [DOI] [PubMed] [Google Scholar]
- 56.Bhargava A, Jolliffe D, Howard LL. Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study-Kindergarten. Br J Nutr. 2008;100:438–444. doi: 10.1017/S0007114508894366 [doi]. [DOI] [PubMed] [Google Scholar]
- 57.Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Research in Human Development. 2009;6:144–164. [Google Scholar]
- 58.Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]