Abstract
BACKGROUND
Many patients with primary brain tumors suffer from cognitive deficits, which negatively impact their quality of life. However, cognitive rehabilitation programs for these patients are scarce. We developed an iPad-based cognitive rehabilitation program for brain tumor patients, which was based on our effective face-to-face cognitive rehabilitation program. After successful completion of a feasibility study, a randomized controlled trial has been started.
OBJECTIVE
To evaluate the immediate and long-term effects of the iPad-based program on cognitive performance and patient-reported outcome measures (PROMs) in patients with primary brain tumors in an early stage of the disease.
METHODS
Prior to surgery, patients with presumed low-grade glioma and meningioma are included. Before surgery and 3 mo after surgery, neuropsychological assessments are conducted. After the second neuropsychological assessment, patients are assigned to the intervention group or waiting-list control group. The intervention consists of psychoeducation, compensation training, and retraining. Patients are advised to spend 3 h per week on the program for 10 wk. Immediately after completion of the program and a half-year thereafter, postintervention assessments take place. Patients in the control group are offered the opportunity to follow the program after all study assessments.
EXPECTED OUTCOMES
We expect that early cognitive rehabilitation has beneficial effects on cognitive performance and PROMs in brain tumor patients.
DISCUSSION
The iPad-based program allows brain tumor patients to follow a cognitive rehabilitation program from their homes. Forthcoming results may contribute to further improvement of supportive care for brain tumor patients.
Keywords: Cognitive rehabilitation, EHealth, Glioma, Intervention studies, Meningioma, Study protocol
ABBREVIATIONS
- CNS VS
central nervous system vital signs
- PROMs
patient-reported outcome measures
- RCT
randomized controlled trial
- SAEs
serious adverse events
GENERAL INFORMATION
Protocol Title
Cognitive rehabilitation in brain tumor patients after neurosurgery.
Trial Registration
The study has been registered in The Netherlands National Trial Register (NTR 5392) and on ClinicalTrials.gov (NTC03373487).
Funding
This research (project number: 842003009) is supported by the Dutch organization for health research and innovation, ZonMw (Laan van Nieuw Oost-Indie 334, 2593 CE, The Hague, The Netherlands). The development of the iPad-app ReMind was funded by Health Insurers Innovation Foundation, CbusineZ and ‘t Hoofdgerecht without commercial interest.
Investigators and Research Sites
An overview of the participating institutions and researchers involved is provided in Table 1.
TABLE 1.
Investigators and Research Sites of the Study
| Project member | Role | Research site |
|---|---|---|
| GJM Rutten, MD, PhD | Principal investigator, neurosurgeon | Elisabeth-TweeSteden Hospital |
| SD van der Linden, MSc | PhD student, coordinating investigator | 5022 GC Tilburg, The Netherlands |
| K Gehring, PhD | Project leader, coordinating investigator | Tilburg University |
| MM Sitskoorn, PhD | Project leader | 5000 LE, Tilburg, the Netherlands |
| CMF Dirven, MD, PhD | Associate investigator | Erasmus Medical Center |
| DD Satoer, PhD | Associate investigator, contact person EMC | 3015 CE Rotterdam, The Netherlands |
| MJB Taphoorn, MD, PhD | Associate investigator | Haaglanden Medical Center |
| L Dirven, PhD | Associate investigator, contact person HMC | 2501 CK The Hague, The Netherlands |
RATIONALE AND BACKGROUND INFORMATION
Patients with primary brain tumors experience various symptoms, including cognitive deficits. Many factors can cause or aggravate cognitive deficits, for example, the tumor itself, tumor treatment, tumor-related epilepsy, or psychological distress.1,2 Cognitive rehabilitation programs are aimed at alleviating (the impact of) these cognitive deficits. A few methodologically well-designed studies demonstrated positive effects of cognitive rehabilitation in brain tumor patients.3,4 However, despite the high need for rehabilitation services and supportive care in brain tumor patients, cognitive rehabilitation programs are not always available or accessible for patients with primary brain tumors in clinical practice.5-7
Several years ago, our group conducted a randomized controlled trial (RCT) in 140 patients with glioma on the effects of a face-to-face cognitive rehabilitation program and demonstrated beneficial effects of the program.3 In a joint patient–researcher initiative, the program was converted into an iPad-based cognitive rehabilitation program, both in Dutch and English, to make the program widely available for patients with primary brain tumors. The content of the program has largely remained the same. We successfully completed a small-scale study to evaluate the feasibility of the use of the renewed program in a clinical (research) setting.8 Although recruitment of patients appeared to be challenging, patients were satisfied with the program and dropout rate was low. Based on the findings in the feasibility study, adjustments were made to improve the study protocol and the program, before the initiation of a larger RCT. In the RCT, the efficacy of the iPad-based cognitive rehabilitation program will be evaluated. In this manuscript, a detailed description of the study protocol is presented.
STUDY GOALS AND OBJECTIVES
The purpose of this study is to evaluate the immediate and long-term effects of early cognitive rehabilitation in patients with primary brain tumors. Effects on cognitive performance as determined by neuropsychological testing, as well as effects on patient-reported outcome measures (PROMs) will be evaluated, both on a group level and on an individual level. We hypothesize that early cognitive rehabilitation has beneficial effects on cognitive test performance and PROMs in brain tumor patients recovering from neurosurgery.
The specific objectives are:
To investigate the immediate and long-term effects of early cognitive rehabilitation via the ReMind-app on group and individual cognitive performance (ie, tests of attention, memory, and executive functioning).
To investigate the immediate and long-term effects of early cognitive rehabilitation via the ReMind-app on group and individual self-reported cognitive functioning, fatigue, psychological distress, community integration, and professional functioning.
STUDY DESIGN
Figure illustrates the design of the study. This prospective, controlled study compares outcomes of 2 parallel groups, namely an intervention group and a waiting-list control-group, to evaluate the efficacy of an early cognitive rehabilitation program. Adult patients with presumed low-grade glioma and meningioma who will undergo resective surgery are screened for eligibility. Inclusion and exclusion criteria are described in Table 2. Neuropsychological assessments are carried out 1 d before surgery (T0), 3 mo after surgery (T3; preintervention), 6 mo after surgery (T6; postintervention), and 12 mo after surgery (T12; half-year follow-up). With the use of this dual baseline design, practice effects can be minimized. In the coordinating center of the study, T0 and T3 assessments are embedded in standard clinical care in the hospital. Immediately after T3, the preintervention assessment, patients are allocated in a 1:1 ratio to the intervention group or control group, after which the intervention group follows the cognitive rehabilitation program on a borrowed iPad (Apple Inc, Cupertino, California) for about 10 wk. Immediate effects of the intervention are examined at T6. A half-year later (T12), long-term effects are evaluated. After completion of all study assessments, patients in the control group have the opportunity to follow the cognitive rehabilitation program.
FIGURE.
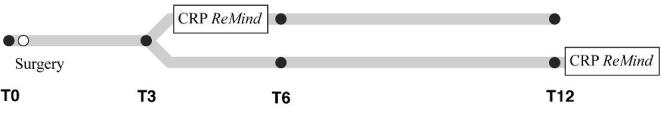
Study design. CRP, cognitive rehabilitation program.
TABLE 2.
Eligibility Criteria of the Study
| Inclusion criteria | |
| • Adult patients (age ≥ 18) | |
| • A supratentorial or infratentorial brain tumor that is radiologically suspect for either a meningioma or low-grade glioma | |
| • Resective surgery for this brain tumor | |
| Exclusion criteria | |
| • Tumor resection in the last year | |
| • Chemotherapy or radiotherapy in the last 2 yr | |
| • Presence/history of progressive neurological disease, severe psychiatric disorder, or substance abuse | |
| • Diagnosis of acute neurological or mild psychiatric disorders in the last 2 yr (eg, CVA) | |
| • Multiple (>1) tumors | |
| • Lack of basic proficiency in Dutch | |
| • Karnofsky Performance Score below 70 | |
| • IQ below 85, or (very) low cognitive skills | |
| • Insufficient reading skills, visual impairment, or motor impairment limiting the ability to follow the cognitive rehabilitation program | |
| Exclusion after informed consent | |
| • Severe surgery-related complication (eg, meningitis or CVA) | |
| • Referral to formal cognitive rehabilitation |
METHODOLOGY
Participants
Between February 2016 and July 2018, patients are included according to the eligibility criteria listed in Table 2. Patients were included in the coordinating center, and 2 medical centers were recently added. We aim to include 150 participants prior to surgery. With a maximum attrition rate of 33%, 100 patients will be evaluated (50 per group). Every effort will be made to obtain assessments for patients who drop out of the study, to facilitate carrying out intention-to-treat analyses. Prior to the first neuropsychological assessment (T0), informed consent is obtained. Patients can choose to involve an informal caregiver in the study/rehabilitation program. If they choose so, the informal caregiver will have to provide informed consent as well.
Intervention
The iPad-app ReMind, based on our face-to-face cognitive rehabilitation program3,9,10, is used in this study. The program consists of psychoeducation, compensation training, and retraining. In the compensation training, compensatory strategies are provided, together with fill-in exercises to practice with the strategies in daily life. The retraining includes game-like exercises aimed at training different forms of attention (ie, sustained, selective, alternating, and divided attention). For a detailed description of content of the ReMind-app, we refer to our feasibility study.8 In a first face-to-face meeting with the researcher, patients receive an iPad (Apple Inc) with the app installed, so that they can work through the program at home. After this meeting, patients are called every 2 wk by the researcher to monitor their progress. It is expected that patients spend approximately 3 h per week on the program to complete the program within 10 wk. Adherence to the program is considered acceptable if patients complete ≥80% of both the strategy training and the retraining. An English version of the app is currently being evaluated in a pilot study in San Francisco (NCT02783495).
“Randomization” by Minimization
Group assignment takes place immediately after the 3 mo assessment (ie, the preintervention assessment). Patients are consecutively assigned to the cognitive rehabilitation group and the waiting-list control group in a 1:1 ratio by means of the minimization method, which will balance the groups for age, tumor histology, baseline cognitive performance, physical status, and participation in other psychosocial interventions. The minimization method has been proven to provide more balanced groups in smaller trials, compared to restricted (stratified) and unrestricted (simple) randomization.11 Access to an online minimization program is provided by the Dutch Cancer Institute.12
Measures
Outcome measures of the study are listed in Table 3. A computerized neuropsychological test battery, central nervous system Vital Signs (CNS VS;13 CNS Vital Signs, LCC, Morrisville, North Carolina), is administered to measure different aspects of cognitive functioning, including attention, memory, and executive functioning. This user-friendly tool can be easily embedded in clinical care, due to rapid administration and semi-automatic processing of results. The battery consists of 7 tests, which are based on conventional neuropsychological tests (eg, Stroop and Symbol Digit Coding). Additionally, 3 paper-and-pencil (sub)tests were added to the assessment protocol, to measure verbal memory recall,14 working memory,15 and word fluency;16 cognitive functions that are not sufficiently covered by the tests of CNS VS.
TABLE 3.
Overview of Neuropsychological Tests and Questionnaires Used in the Study
| Neuropsychological tests | Cognitive domain(s) | T0 | T3 | T6 | T12 |
|---|---|---|---|---|---|
| 1. Verbal memory test (CNS VS)13,a | Verbal memory | X | X | X | X |
| 2. Visual memory test (CNS VS)13,a | Visual memory | X | X | X | X |
| 3. Finger tapping test (CNS VS)13, | Psychomotor speed | X | X | X | X |
| 4. Symbol digit coding (CNS VS)13,a | Processing speed | X | X | X | X |
| 5. Stroop test (CNS VS)13,a | Selective attention, cognitive flexibility | X | X | X | X |
| 6. Shifting attention test (CNS VS)13,a | Cognitive flexibility | X | X | X | X |
| 7. Continuous performance test (CNS VS)13,a | Sustained attention | X | X | X | X |
| 8. Paired associates (Wechsler memory scale-III)14 | Verbal memory | X | X | X | X |
| 9. Digit span (Wechsler adult intelligence scale-III)15 | Working memory | X | X | X | X |
| 10. Letter fluency16 | Semantic memory, executive functioning, verbal fluency | X | X | X | X |
| Questionnaires | PROMs | T0 | T3 | T6 | T12 |
| a. Cognitive failure questionnaire17 | Cognitive complaints | X | X | X | X |
| b. Multidimensional fatigue inventory18 | Fatigue | X | X | X | X |
| c. Hospital anxiety and depression scale19 | Anxiety and depression | X | X | X | X |
| d. Community integration questionnaire20 | Independence and participation | X | X | ||
| e. Work ability index21 | Work ability | X | X | ||
| f. Work limitation questionnaire22 | Work limitations | X | X | ||
| g. Behavior rating inventory of executive function—adult version23,b | Executive functioning | Xb | Xb | ||
| h. Study-specific evaluation questionnaire (intervention group only)b | Experience with the ReMind-program | Xb |
aCNS Vital Signs, LCC
bPatient-report and proxy-report versions are used.
Self-reported cognitive functioning, fatigue, and psychological distress are evaluated at all time-points using different questionnaires.17-19 At T0 and T12, questionnaires on community integration and professional functioning are administered as well.20-22 Additionally, self-report and proxy-report questionnaires on executive functioning are filled out before (T3) and immediately after (T6) the intervention,23 and a study-specific evaluation questionnaire is administered at T6. This distribution of questionnaires was chosen to minimize patient burden per time point (see Table 3).
DISCUSSION
Many patients with primary brain tumors suffer from cognitive deficits, but evidence-based interventions targeting these problems are scarce.2,24,25 A few studies have been conducted on the effectiveness of cognitive rehabilitation in brain tumor patients, but studies are often hampered by methodological limitations. For example, the majority of previous studies included (very) small sample sizes and/or did not include a control group.26-30 A decade ago, our RCT demonstrated positive results of our face-to-face cognitive rehabilitation program in 140 glioma patients with stable disease.3 Shortly thereafter, the RCT of Zucchella and colleagues in 53 brain tumor patients indicated that early cognitive rehabilitation had beneficial effects on cognitive function.4 Unfortunately, in the last couple of years, very little additional research has been carried out on this topic. More research with larger patient samples and comparison of an intervention group to a control condition is needed, to rule out effects of practice and natural recovery. Also, attention should be paid to the dissemination of the program and the implementation in clinical care.
Therefore, we initiated an RCT on the effects of the iPad-based cognitive rehabilitation program ReMind, which was based on our effective face-to-face program and specifically developed for brain tumor patients in a joint patient–researcher initiative. One of the strengths of the study is that both objective cognitive performance as well as PROMs are included. Using relevant questionnaires, insight is gained into patients’ daily functioning, which we aim to improve with cognitive rehabilitation. Also, a unique aspect of the study is that informal caregivers are involved. This is important, since brain tumor diagnosis does not only affect the patient, but also the people in his or her environment. Informal caregivers are invited to assist the patient during the intervention and to complete a few questionnaires. Besides an extra source of information, involvement of informal caregivers may also be associated with better treatment adherence and less caregiver burden. In addition, patient-proxy agreement on patient's executive functioning can be studied using the completed questionnaires from this study.
Based on previous research and patients’ needs, some authors have suggested that cognitive rehabilitation should preferably start as early as possible.4,7,27 Potentially, this has the advantage that cognitive dysfunction, for example due to adjuvant treatment, can be minimized or prevented. By including a half-year follow-up assessment (T12) in our study, such potential preventive effects can be evaluated.
A weakness of the study may be that patients are not selected based on presence of cognitive deficits/complaints at T0. However, as we expect preventative effects of early cognitive rehabilitation, potential stable good performance in the intervention group vs a decline in the control group may be observed over time. Also, based on our feasibility study8 and patient recruitment up to now, we expect that accrual of sufficient participants in the RCT will be challenging. This is not only a problem in our study, but a common phenomenon in studies in cancer patients.31,32 To increase patient accrual, 2 additional participating centers are recruiting patients now.
Our study will include a mix of patients with glioma and meningioma. Different types and grades of brain tumors may affect reorganizational processes in the brain in different ways. In addition, varying treatment regimens (radiotherapy and/or chemotherapy or none) that our patients undergo may further impact cognitive functioning. Subgroup analyses in patients with glioma and meningioma separately may help to determine potentially distinctive gains, and maintenance thereof, after cognitive rehabilitation.
To conclude, the effects of an iPad-based cognitive rehabilitation program on cognitive performance and PROMs will be examined in patients with primary brain tumors early in the course of the disease. If this program proves to be effective, we may be able to improve supportive care for brain tumor patients, by implementing this easily accessible cognitive rehabilitation program in clinical practice early after surgery.
TRIAL STATUS
The trial status at the time of submission of this manuscript is recruiting.
SAFETY CONSIDERATIONS
For patients in this study, there are no risks of participation, which is also confirmed by the local medical ethical review board. All serious adverse events (SAEs) are immediately recorded in the Investigator Site File and reported to the local medical ethical review board on a yearly basis.
FOLLOW-UP
Neuropsychological assessments are conducted prior to surgery and 3, 6, and 12 mo after surgery. SAEs are reported until the end of the study.
DATA MANAGEMENT AND STATISTICAL ANALYSIS
Data are handled confidentially. A patient identification code list, which is only accessible by direct members of the research team, is used to link the data obtained from neuropsychological testing, questionnaires and medical charts to the participant. Collected data (ie, pseudonymized paper/digital files) are stored at the coordinating medical center and are only accessible by direct members of the research team. The ReMind-app saves data locally on the PIN code protected iPad (Apple Inc).
All statistical analyses will be conducted using SPSS version 24 (IBM Inc, Armonk, New York), with an alpha set at .05. First, descriptive statistics will be calculated. Subsequently, it will be checked whether the randomization via the minimization method has been successful in balancing the intervention and control group. Then, group analyses on the efficacy of the program will be conducted on an intention-to-treat basis. Analysis of (co)variance will be conducted to compare mean post intervention scores of the intervention group with mean scores of the control group. Alternatively, we may use linear mixed models that implicitly deal with missing data under the assumption of missing at random.
Since group results may mask the variability in individual responses to the intervention, we also plan to study change at the individual patient level. Reliable change indices will be calculated, reflecting change at the individual level in the context of observed changes for the control group of this study.33 Using this method, possible practice effects, natural recovery, and measurement errors are taken into account. Numbers of patients who have improved vs the number of patients who remained stable, or declined, will be compared between groups.
QUALITY ASSURENCE
Annual monitoring is performed by an independent clinical monitor within the hospital. Interim progress reports are sent to the local medical ethical review board and to the funding agency. The principal investigator and coordinating investigator have successfully completed the course on Good Clinical Practice, and the study is carried out in accordance with these guidelines.
EXPECTED OUTCOMES OF THE STUDY
After the feasibility study,8 this RCT is the next necessary step towards broader dissemination of the cognitive rehabilitation program. There is a high need for management of cognitive problems and patients do not always find their way to cognitive rehabilitation.34 As previously described, cognitive rehabilitation programs for brain tumor patients are scarce and research on cognitive rehabilitation in brain tumor patients is lagging. If we are able to demonstrate that cognitive rehabilitation via this eHealth intervention is effective in our sample of meningioma and low-grade glioma patients, the next step will be to make the app widely available for patients in both Dutch and English.
DURATION OF THE PROJECT
Patient recruitment runs from February 2016 to June 2018. The study ends after the last follow-up assessment one year later, in June 2019.
PROJECT MANAGEMENT
The study is designed and led by the principal investigator Dr Rutten, and project leaders Dr Gehring and Prof Dr Sitskoorn. The treating neurosurgeon/physician assistant identifies eligible patients and provide information about the study. Neuropsychological assessments are carried out by well-trained research assistants. Prior to the first neuropsychological assessment, informed consent is obtained by the research assistants or the study investigator. The study investigator, Ms Van der Linden, coordinates the logistics, supervises all patients, and manages the data. The investigators will present the findings in manuscripts and on the registered platforms. App maintenance is managed by Dr Gehring.
ETHICS
The study is approved by the local medical ethical review board (METC Brabant/CCMO: P1449, NL51152.028.14), and the study protocol is approved by the institutional review board of each participating center. All substantial changes to the protocol will be resubmitted to the relevant review boards. The study will be conducted in accordance with the Declaration of Helsinki35 and in accordance with the Dutch Medical Research Involving Human Subjects Act (WMO). Prior to the first neuropsychological assessment (T0), written informed consent will be obtained from all participants. For ethical reasons, patients in the waiting list control group may borrow an iPad (Apple Inc) and follow the cognitive rehabilitation program after completion of all study assessments (Figure).
Disclosures
This research is supported by the Dutch organization for health research and innovation (ZonMw; project number: 842003009). The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
REFERENCES
- 1. Taphoorn MJB, Klein M. Cognitive deficits in adult patients with brain tumours. Lancet Neurol. 2004;3(3):159–168. [DOI] [PubMed] [Google Scholar]
- 2. Day J, Gillespie DC, Rooney AG, et al.. Neurocognitive deficits and neurocognitive rehabilitation in adult brain tumors. Curr Treat Options Neurol. 2016;18(5):22. [DOI] [PubMed] [Google Scholar]
- 3. Gehring K, Sitskoorn MM, Gundy CM, et al.. Cognitive rehabilitation in patients with gliomas: a randomized, controlled trial. J Clin Oncol. 2009;27(22):3712–3722. [DOI] [PubMed] [Google Scholar]
- 4. Zucchella C, Capone A, Codella V, et al.. Cognitive rehabilitation for early post-surgery inpatients affected by primary brain tumor: a randomized, controlled trial. J Neurooncol. 2013;114(1):93–100. [DOI] [PubMed] [Google Scholar]
- 5. Bergo E, Lombardi G, Pambuku A, et al.. Cognitive rehabilitation in gliomas and other brain tumors: state of the art. Biomed Res Int. 2016;2016:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pace A, Villani V, Parisi C, et al.. Rehabilitation pathways in adult brain tumor patients in the first 12 months of disease. A retrospective analysis of services utilization in 719 patients. Support Care Cancer. 2016;24(11):4801–4806. [DOI] [PubMed] [Google Scholar]
- 7. Langbecker D, Yates P. Primary brain tumor patients’ supportive care needs and multidisciplinary rehabilitation, community and psychosocial support services: awareness, referral and utilization. J Neurooncol. 2016;127(1):91–102. [DOI] [PubMed] [Google Scholar]
- 8. Van der Linden SD, Sitskoorn MM, Rutten GJM, Gehring K. Feasibility of the evidence-based cognitive telerehabilitation program ReMind for patients with primary brain tumors. J Neurooncol. 2018;137(3):523–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gehring K, Aaronson NK, Taphoorn MJB, Sitskoorn MM. A description of a cognitive rehabilitation programme evaluated in brain tumour patients with mild to moderate cognitive deficits. Clin Rehabil. 2011;25(8):675–692. [DOI] [PubMed] [Google Scholar]
- 10. Gehring K, Aaronson NK, Gundy CM, Taphoorn MJB, Sitskoorn MM. Predictors of neuropsychological improvement following cognitive rehabilitation in patients with gliomas. J Int Neuropsychol Soc. 2011;17(02):256–266. [DOI] [PubMed] [Google Scholar]
- 11. Scott NW, McPherson GC, Ramsay CR, Campbell MK. The method of minimization for allocation to clinical trials. a review. Control Clin Trials. 2002;23(6):662–674 [DOI] [PubMed] [Google Scholar]
- 12. ALEA Online Randomisation Software. Available at: http://www.aleaclinical.eu. Accessed March 28, 2018. [Google Scholar]
- 13. Gualtieri CT, Johnson LG. Reliability and validity of a computerized neurocognitive test battery, CNS Vital Signs. Arch Clin Neuropsychol. 2006;21(7):623–643. [DOI] [PubMed] [Google Scholar]
- 14. Wechsler D. Wechsler Memory Scale. 3rd ed San Antonio: The Psychological Corporation; 1997. [Google Scholar]
- 15. Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed Nederlandstalige bewerking. Technische handleiding Amsterdam: Harcourt test Publishers; 2015. [Google Scholar]
- 16. Schmand B, Groenink SC, Van den Dungen M. Letter fluency: psychometrische eigenschappen en Nederlandse normen. GEEG. 2008;39(2):64–74. [DOI] [PubMed] [Google Scholar]
- 17. Broadbent DE, Cooper PF, FitzGerald P, Parkes KR. The cognitive failures questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982;21(1):1–16. [DOI] [PubMed] [Google Scholar]
- 18. Smets EMA, Garssen B, Bonke B, De Haes JCJM. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39(3):315–325. [DOI] [PubMed] [Google Scholar]
- 19. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 20. Willer B, Ottenbacher KJ, Coad ML. The community integration questionnaire a comparative examination. Am J Phys Med Rehabil. 1994;73(2):103–111. [DOI] [PubMed] [Google Scholar]
- 21. De Zwart BC, Frings-Dresen MH, Van Duivenbooden JC. Test-retest reliability of the work ability index questionnaire. Occup Med. 2002;52(4):177–181. [DOI] [PubMed] [Google Scholar]
- 22. Lerner D, Amick BC 3, Rogers WH, Malspeis S, Bungay K, Cynn D. The work limitations questionnaire. Med Care. 2001;39(1):72–85. [DOI] [PubMed] [Google Scholar]
- 23. Scholte E, Noens I. BRIEF-A Vragenlijst Over Executief Functioneren Bij Volwassenen. Handleiding. Amsterdam: Hogrefe; 2011. [Google Scholar]
- 24. Gehring K, Sitskoorn MM, Aaronson NK, Taphoorn MJB. Interventions for cognitive deficits in adults with brain tumours. Lancet Neurol. 2008;7(6):548–560. [DOI] [PubMed] [Google Scholar]
- 25. Gehring K, Aaronson NK, Taphoorn MJB, Sitskoorn MM. Interventions for cognitive deficits in patients with a brain tumor: an update. Expert Rev Anticancer Ther. 2010;10(11):1779–1795. [DOI] [PubMed] [Google Scholar]
- 26. Sherer M, Meyers CA, Bergloff P. Efficacy of postacute brain injury rehabilitation for patients with primary malignant brain tumors. Cancer.1997;80(2):250–257. [PubMed] [Google Scholar]
- 27. Locke DE, Cerhan JH, Wu W, et al.. Cognitive rehabilitation and problem-solving to improve quality of life of patients with primary brain tumors: a pilot study. J Support Oncol. 2008;6(8):383–391. [PubMed] [Google Scholar]
- 28. Hassler MR, Elandt K, Preusser M, et al.. Neurocognitive training in patients with high-grade glioma: a pilot study. J Neurooncol. 2010;97(1):109–115. [DOI] [PubMed] [Google Scholar]
- 29. Maschio M, Dinapoli L, Fabi A, Giannarelli D, Cantelmi T. Cognitive rehabilitation training in patients with brain tumor-related epilepsy and cognitive deficits: a pilot study. J Neurooncol. 2015;125(2):419–426. [DOI] [PubMed] [Google Scholar]
- 30. Sacks-Zimmerman A, Duggal D, Liberta T. Cognitive remediation therapy for brain tumor survivors with cognitive deficits. Cureus. 2015;7(10):e350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Grunfeld E, Zitzelsberger L, Coristine M, Aspelund F. Barriers and facilitators to enrollment in cancer clinical trials: qualitative study of the perspectives of clinical research associates. Cancer. 2002;1(7):1577–1583. [DOI] [PubMed] [Google Scholar]
- 32. Sateren WB, Trimble EL, Abrams J, et al.. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. J Clin Oncol. 2002;20(8):2109–2117. [DOI] [PubMed] [Google Scholar]
- 33. Maassen GH, Bossema E, Brand N. Reliable change and practice effects: outcomes of various indices compared. J Clin Exp Neuropsychol. 2009;31(3):339–352. [DOI] [PubMed] [Google Scholar]
- 34. Langbecker D, Ekberg S, Yates P. Don’t need help, don’t want help, can’t get help: How patients with brain tumors account for not using rehabilitation, psychosocial and community services. Patient Educ Couns. 2017;100(9):1744–1750. [DOI] [PubMed] [Google Scholar]
- 35. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. [DOI] [PubMed] [Google Scholar]


