Abstract
The nuclear receptor (NR) superfamily consists of 48 members that are divided into seven subfamilies. NRs are transcription factors that play an important role in a number of biological processes. The NR superfamily includes androgen receptor, which is a key player in prostate cancer pathogenesis, suggesting the functional roles of other NRs in prostate cancer. The findings on the roles of NRs in prostate cancer thus far have shown that several NRs such as vitamin D receptor, estrogen receptor β, and mineralocorticoid receptor play antioncogenic roles, while other NRs such as peroxisome proliferator-activated receptor γ and estrogen receptor α as well as androgen receptor play oncogenic roles. However, the roles of other NRs in prostate cancer remain controversial or uninvestigated. Further research on the role of NRs in prostate cancer is required and may lead to the development of novel preventions and therapeutics for prostate cancer.
Keywords: androgen receptor, estrogen receptor, glucocorticoid receptor, mineralocorticoid receptor, nuclear receptor, progesterone receptor, prostate cancer, steroid receptor
1. Introduction
Prostate cancer is primarily characterized by a dependence on the axis of androgen and its cognitive receptor, the nuclear receptor (NR) androgen receptor (AR), which plays roles in carcinogenesis, cancer development, disease progression, and treatment resistance [1]. Therefore, AR axis-targeting therapeutics such as androgen-deprivation therapy and antiandrogens have been the gold-standard treatments for recurrent or advanced prostate cancer [2].
The NR superfamily consists of 48 members that are divided into seven subfamilies [3]. The classification into subfamilies was determined by phylogenetic tree analysis based on their sequences [4]. NRs are transcription factors that play important functions in various biological processes including growth, development, metabolism, reproduction, and inflammation [3]. Except for subfamily 0, the structure of NRs is composed of five or six domains: A–E(F) (A/B, N-terminal domain; C, DNA-binding domain; D, hinge region; E/(F), ligand-binding domain [LBD]). Most NRs are regulated by endogenous small lipophilic ligands, such as steroids, retinoids, and phospholipids, while some NRs are still classified as orphan receptors with no identified ligand thus far [3]. Ligand binding induces conformational changes within the NR, leading to its translocation into the nucleus and binding to cognitive binding sites on DNA throughout the genome [3]. Coregulator proteins, chromatin remodeling factors, and the general transcriptional machinery are then recruited to regulate the expression of NR target genes [3]. Notably, multiple NRs are involved in various aspects of reproduction and several NRs also function in the prostate. In addition, NR-regulated biological processes, such as growth, development, metabolism, and inflammation, are critical factors for prostate cancer pathogenesis [5,6]. Accordingly, other NRs have been speculated to function in prostate cancer pathogenesis in addition to their roles in physiological and pathological conditions. Most NRs are expressed and functional in the nonmalignant prostate as well as during prostate cancer or are dysregulated in prostate cancer [7,8]. Multiple NRs, including retinoic acid receptors (RARs), retinoid X receptors (RXRs), vitamin D receptor (VDR), liver X receptors (LXRs), peroxisome proliferator-activated receptors (PPARs), farnesoid X receptors (FXRs), and chicken ovalbumin upstream promoter transcription factor γ (COUP-TFγ), are strongly expressed in nonmalignant prostate epithelial RWPE-1 cells and normal human prostate epithelial cells [7]. In contrast, the expression levels of several NRs including LXRα, LXRβ, RARγ, and RXRα are downregulated in malignant-transformed prostate epithelial RWPE-2 cells as well as clinical prostate cancer samples [7]. These studies suggest that better clarification of the precise roles of NRs in prostate cancer may not only help better elucidate their cellular functions but may also lead to the development of novel prevention and therapeutic strategies for prostate cancer.
In this review, we summarize the roles of NRs in prostate cancer according to the classification into subfamilies with a focus on NRs other than AR (Table 1).
Table 1.
Nuclear receptor superfamily proteins and their roles in prostate cancer.
| Family | Common Name | Abbreviation | GENE Name | Ligand | Gene Expression in Prostate Tissues (Ref. [7]) | Expression in Prostate Cancer | Effect on AR Signaling | Oncogenic Role in Prostate Cancer | References |
|---|---|---|---|---|---|---|---|---|---|
| 0B | Dosage-sensitive sex reversal-adrenal hypoplasia congenital critical region on the X chromosome, Gene 1 | DAX1 | NR0B1 | Orphan | Detectable | Controversial (increased/decreased) | Suppressive | - | [9,10,11,12] |
| Short heterodimeric partner | SHP | NR0B2 | Orphan | Non-detectable | Decreased | Suppressive | Suppressive | [14,15,16,17,18,19] | |
| 1A | Thyroid hormone receptor-α | TRα | THRA | Thyroid hormones | Detectable | - | - | - | - |
| Thyroid hormone receptor-β | TRβ | THRB | Thyroid hormones | Non-detectable | - | - | - | - | |
| 1B | Retinoic acid receptor-α | RARα | RARA | Retinoic acids | Non-detectable | - | - | - | - |
| Retinoic acid receptor-β | RARβ | RARB | Retinoic acids | Detectable | Decreased | - | Suppressive | [23,24,26,27,28,29,31] | |
| Retinoic acid receptor-γ | RARγ | RARG | Retinoic acids | Non-detectable | Decreased | Suppressive | Suppressive | [7,21,22,24,25,26,27,28,29,30] | |
| 1C | Peroxisome proliferator-activated receptor-α | PPARα | PPARA | Fatty acids | Detectable | No change | - | - | [34] |
| Peroxisome proliferator-activated receptor-β | PPARβ | PPARD | Fatty acids | Detectable | No change | - | Controversial (promotive/suppressive) | [34,44,45,46] | |
| Peroxisome proliferator-activated receptor-γ | PPARγ | PPARG | Fatty acids | Non-detectable | Increased | Controversial(promotive/suppressive) | Promotive | [34,35,36,37,38,39,40,41,42,43] | |
| 1D | Reverse-Erb-α | REV-ERBα | NR1D1 | Heme | Non-detectable | - | - | - | - |
| Reverse-Erb-β | REV-ERBβ | NR1D2 | Heme | Detectable | - | - | - | - | |
| 1F | Retinoic acid receptor-related orphan receptor-α | RORα | RORA | Sterols | Detectable | Decreased | Suppressive | [51,52] | |
| Retinoic acid receptor-related orphan receptor-β | RORβ | RORB | Sterols | Detectable | - | - | - | - | |
| Retinoic acid receptor-related orphan receptor-γ | RORγ | RORC | Sterols | Non-detectable | Increased | Promotive | Promotive | [49,50] | |
| 1H | Farnesoid X receptor-α | FXRα | NR1H4 | Bile Acids | Detectable | Decreased | - | Suppressive | [54,55,56] |
| Farnesoid X receptor-β | FXRβ | NR1H5P | Orphan | - | Decreased | - | Suppressive | [54,55,56] | |
| Liver X receptor-α | LXRα | NR1H3 | Oxysterols | Detectable | Decreased | None | Suppressive | [7,58,59,60,61,62,63,64,65,66,67] | |
| Liver X receptor-β | LXRβ | NR1H2 | Oxysterols | Detectable | Decreased | None | Suppressive | [7,58,59,60,61,62,63,64,65,66,67] | |
| 1I | Vitamin D receptor | VDR | VDR | 1α,25-dihydroxyvitamin D3 | Non-detectable | - | - | Suppressive | [70,71,72,73,74,75] |
| Pregnane X receptor | PXR | NR1I2 | Endobiotics and xenobiotics | Non-detectable | - | - | - | - | |
| Constitutive androstane receptor | CAR | NR1I3 | Xenobiotics | Non-detectable | - | - | - | - | |
| 2A | Hepatocyte nuclear factor-4-α | HNF4α | HNF4A | Fatty acids | Detectable | - | - | - | - |
| Hepatocyte nuclear factor-4-γ | HNF4γ | HNF4G | Fatty acids | Non-detectable | - | - | - | - | |
| 2B | Retinoid X receptor-α | RXRα | RXRA | 9-cis retinoic acid | Detectable | Decreased | - | Suppressive | [7,26,35,81,82,83,84] |
| Retinoid X receptor-β | RXRβ | RXRB | 9-cis retinoic acid | Detectable | - | - | Suppressive | [26,84,85] | |
| Retinoid X receptor-γ | RXRγ | RXRG | 9-cis retinoic acid | Detectable | - | - | - | - | |
| 2C | Testicular orphan nuclear receptor 2 | TR2 | NR2C1 | Orphan | Non-detectable | - | - | - | - |
| Testicular orphan nuclear receptor 4 | TR4 | NR2C2 | Orphan | Detectable | - | - | Controversial (promotive/suppressive) | [87,88,89,90,91,92,93] | |
| 2E | Tailless homolog orphan receptor | TLX | NR2E1 | Orphan | Non-detectable | - | - | - | - |
| Photoreceptor-cell-specific nuclear receptor | PNR | NR2E3 | Orphan | Non-detectable | - | - | - | - | |
| 2F | Chicken ovalbumin upstream promoter-transcription factor α | COUP-TFα | NR2F1 | Orphan | Detectable | Increased | - | - | [95] |
| Chicken ovalbumin upstream promoter-transcription factor β | COUP-TFβ | NR2F2 | Orphan | Detectable | - | Suppressive | Controversial (promotive/suppressive) | [96,97] | |
| Chicken ovalbumin upstream promoter-transcription factor γ | COUP-TFγ | NR2F6 | Orphan | Detectable | - | - | - | - | |
| 3A | Estrogen receptor-α | ERα | ESR1 | Estrogens | Detectable | Increased | - | Promotive | [101,102,103,104] |
| Estrogen receptor-β | ERβ | ESR2 | Estrogens | Detectable | Decreased | Suppressive | Suppressive | [103,107,108,109,110] | |
| 3B | Estrogen-related receptor-α | ERRα | ESRRA | Orphan | Detectable | Increased | - | - | [112,113,114] |
| Estrogen-related receptor-β | ERRβ | ESRRB | Orphan | Non-detectable | Decreased | - | Suppressive | [112,114,116,117,118] | |
| Estrogen-related receptor-γ | ERRγ | ESRRG | Orphan | Non-detectable | Decreased | - | Suppressive | [112,114,116,117,118] | |
| 3C | Androgen receptor | AR | AR | Androgens | Non-detectable | Increased | Promotive | Promotive | [98,99] |
| Glucocorticoid receptor | GR | NR3C1 | Glucocorticoids | Detectable | Controversial (increased/decreased) | Promotive | Promotive | [7,119,121,122,123,124,125,126] | |
| Mineralocorticoid receptor | MR | NR3C2 | Mineralocorticoids and glucocorticoids | Non-detectable | - | Suppressive | Suppressive | [128,129,130,131,132,133,134] | |
| Progesterone receptor | PR | PGR | Progesterone | Non-detectable | Controversial (increased/decreased) | Unknown | Suppressive | [136,137,138,139,140,141,142] | |
| 4A | Nerve growth factor 1B | NGF1-B | NR4A1 | Orphan | Detectable | - | - | - | - |
| Nurr-related factor 1 | NURR1 | NR4A2 | Unsaturated fatty acids | Non-detectable | - | - | - | - | |
| Neuron-derived orphan receptor-1 | NOR-1 | NR4A3 | Orphan | Non-detectable | - | - | - | - | |
| 5A | Steroidogenic factor-1 | SF-1 | NR5A1 | Phospholipids | Detectable | Increased | Promotive | Promotive | [143] |
| Liver receptor homolog-1 | LRH-1 | NR5A2 | Phospholipids | Detectable | - | Promotive | Promotive | [144] | |
| 6A | Germ cell nuclear factor | GCNF | NR6A1 | Orphan | Non-detectable | Increased | - | - | - |
-, Not investigated.
2. Subfamilies of NRs
2.1. Subfamily 0
This subfamily includes the atypical NRs, including dosage-sensitive sex reversal-adrenal hypoplasia congenital critical region on the X chromosome, Gene 1 (DAX1) and small heterodimer partner (SHP) [3]. These two NRs are unique in that their structures contain only a LBD, which interacts with the LBDs of other NRs to regulate the transcriptional activity of the interacting NRs [3].
2.1.1. Dosage-Sensitive Sex Reversal-Adrenal Hypoplasia Congenital Critical Region on the X Chromosome, Gene 1 (DAX1)
DAX1 is predominantly expressed in male and female reproductive organs, including testis, prostate, ovary, and adrenal gland, where DAX1 regulates steroidogenesis, development, and reproduction via interactions with other NRs [9]. The expression pattern of DAX1 in nonmalignant prostate and prostate cancer is controversial. Strong nuclear expression of DAX1 was observed in normal prostatic epithelial cells, but reduced expression was observed in benign prostatic hyperplasia (BPH) and androgen-independent PC-3 prostate cancer cells [9,10,11]. However, DAX1 exhibited a variable expression pattern in nuclei of prostate cancer cells and its expression was inversely correlated with Gleason score [12]. Functionally, DAX1 repressed AR activity in androgen-dependent LNCaP prostate cancer cells [9]. However, a biological role for DAX1 in prostate cancer has not been reported so far.
2.1.2. Short Heterodimeric Partner (SHP)
SHP is abundantly expressed mainly in the enterohepatic system, including in liver and intestine, where SHP regulates bile acid synthesis and cholesterol homeostasis [13]. A recent study showed downregulation of SHP in several human prostate cancer cell lines compared with nonmalignant prostatic epithelial cells [14]. SHP expression was also reduced in prostate cancer tissues compared with BPH tissues [15]. Moreover, decreased SHP expression in prostate cancer tissues was associated with increased risks of recurrence and progression after radical prostatectomy [16]. Similar to DAX1, SHP was shown to repress AR transcriptional activity in LNCaP cells [14]. Furthermore, synthetic SHP agonists could induce apoptosis and suppress the in vitro growth of androgen-independent DU-145 prostate cancer cells [17]. SHP overexpression also suppressed cell proliferation in prostate cancer cells [16], increased apoptosis in LNCaP cells [18], and induced cell cycle arrest at G1 phase in PC-3 cells [19], suggesting SHP exerts an antioncogenic role in prostate cancer.
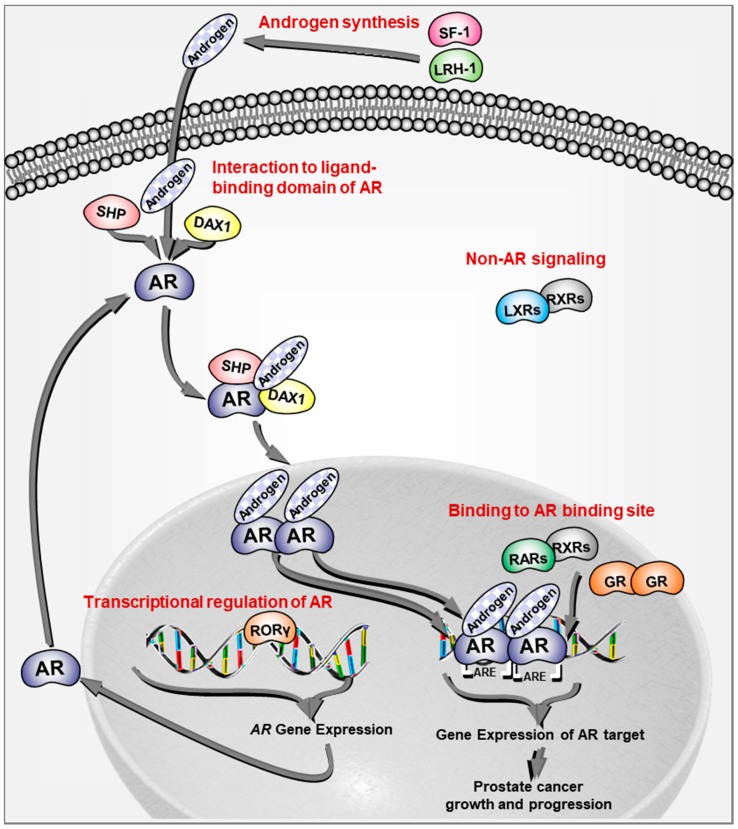
Taken together, these studies indicate that the NRs in subfamily 0 play an antioncogenic role in prostate cancer partially through an inhibitory effect on AR, which may be mediated by their interactions with the LBD of AR (Figure 1).
Figure 1.
Schematic representation of the signaling pathways on androgen receptor signaling in prostate cancer by nuclear receptors. Nuclear receptors regulate androgen receptor (AR) signaling via various mechanisms including androgen synthesis, transcriptional regulation of AR, interaction with the ligand-binding domain of AR, and binding to AR-binding sites in addition to non-AR signaling.
2.2. Subfamily 1
This large subfamily consists of thyroid hormone receptors, RARs, PPARs, reverse-Erb receptors (REV-ERBs), retinoic acid receptor-related orphan receptors (RORs), FXRs, LXRs, and VDR [3]. These receptors are regulated by a variety of lipophilic molecules such as thyroid hormone, fatty acids, bile acids, and sterols [3].
2.2.1. Retinoic Acid Receptors (RARs)
Retinoic acid, the major bioactive metabolite of retinol or vitamin A, induces pleiotropic effects on cell growth and differentiation in various organs [20]. Retinoic acid activity is mediated primarily by members of the RAR subfamily (RARα, RARβ, and RARγ), which form heterodimers with members of the RXR subfamily and regulate the expression of target genes through binding to retinoic acid-response elements [20]. Data from Memorial Sloan Kettering Cancer Center [21] and TCGA Prostate Adenocarcinoma showed that RARγ was significantly and uniquely downregulated in prostate cancer compared with other cancers [22]. In addition, the RARβ promoter methylation status was higher in prostate cancer compared with nonmalignant tissues, suggesting reduced expression of RARβ in prostate cancer [23]. In LNCaP cells, RARγ signaling was shown to suppress AR signaling by competitive binding to AR-binding sites (Figure 1) [24,25]. Consistent with these findings, agonists for RARs alone and in combination with other agents suppressed oncogenic characteristics in prostate cancer cells, including cell proliferation, and reduced prostate tumor growth [24,26,27,28,29]. Interestingly, a selective agonist for RARγ, but not a selective agonist for RARα, showed a suppressive effect on cell proliferation in DU-145 cells, which was reversed by RAR antagonist treatment [30]. In addition, RARβ overexpression was shown to reduce prostate cancer cell proliferation [31]. Taken together, RARβ and RARγ seem to play an antioncogenic role in prostate cancer through an inhibitory effect on AR signaling by competitive binding to AR-binding sites (Figure 1).
2.2.2. Peroxisome Proliferator-Activated Receptors (PPARs)
The PPAR subfamily members (PPARα, PPARβ/δ, and PPARγ) are fatty acid-activated transcription factors that are involved in several physiological processes including modulation of cellular differentiation, development, and metabolism [32]. Upon ligand binding of fatty acids to PPARs, these NRs translocate into the nucleus as heterodimers with RXRs and bind to peroxisome proliferator response elements in target genes to regulate target gene expression [33]. PPARα and PPARβ/δ expressions are detected among normal prostate, BPH, and prostate cancer tissues, while expression of PPARγ was observed in prostate cancer but not in normal prostate and BPH [34]. Furthermore, PPARγ expression was shown to increase with cancer grade/stage and correlate with poor survival in prostate cancer patients, suggesting that PPARγ plays an oncogenic role in prostate cancer development and progression [35,36,37]. Functionally, the effect on AR signaling by PPARγ is controversial and dependent on the cellular context [38]. PPARγ was originally thought to exert antioncogenic properties in prostate cancer because PPARγ agonists inhibited the growth of prostate cancer cells. However, additional studies found that PPARγ agonists inhibited cell growth independent of PPARγ [37], and fatty acids promoted tumorigenesis [39]. Indeed, recent studies showed that PPARγ activation promoted prostate cancer progression [40,41], suggesting that PPARγ inhibition might be useful in prevention and treatment for prostate cancer [42]. Intriguingly, a previous study reported that AR signaling negatively regulated PPARγ signaling, suggesting that PPARγ function may be augmented in castrated conditions [43]. The role of PPARβ/δ in prostate cancer is still controversial [44,45,46], indicating complex functions of PPARs in prostate cancer biology.
2.2.3. Retinoic Acid Receptor-Related Orphan Receptors (RORs)
The ROR superfamily proteins (RORα, RORβ, and RORγ) are generally classified as orphan receptors, but sterols have been suggested as possible ligands. RORs regulate gene expression by binding to ROR response elements as monomers [3,47,48]. RORγ expression is upregulated in prostate cancer and further increased in castration-resistant prostate cancer (CRPC). RORγ drives AR expression while selective RORγ antagonists inhibit AR expression and prostate tumor growth (Figure 1) [49,50], suggesting an oncogenic role for RORγ and its potential as a therapeutic target in prostate cancer. In contrast, an antioncogenic role for RORα in prostate cancer was indicated by its tumor suppression and anti-invasion functions [51,52]. Taken together, these findings suggest distinct functions of RORs in prostate cancer.
2.2.4. Farnesoid X Receptors (FXRs)
The FXR subfamily (FXRα and FXRβ, pseudogene in human) is activated by bile acids to bind to FXR response elements as monomers or as heterodimers with RXR and regulate the expression of diverse genes involved in the metabolism of bile acids, lipids, and carbohydrates [53]. So far, few studies have focused on the molecular effects of FXR activation in prostate cancer. FXR expression was significantly lower in prostate cancer tissues compared with nonmalignant tissues [54]. In addition, FXR and its agonists inhibited cell proliferation in LNCaP and PC-3 cells, suggesting FXR as a potential prevention and therapeutic target for prostate cancer [54,55,56].
2.2.5. Liver X Receptors (LXRs)
The LXR subfamily (LXRα and LXRβ) oxysterol-activated receptors bind to LXR responsive elements as heterodimers with RXRs and regulate the expression of target genes that are involved in lipid metabolism as sensors of cholesterol homeostasis [57]. LXRs are expressed in epithelial and stromal cells of prostate [58]. However, the expression of LXRs was decreased during the progression from hormone-naïve to castration-resistant tumors in a xenograft model [59]. Although the effect of LXR agonists on AR signaling is controversial, knockdown of LXRα and LXRβ revealed no direct effect of LXRs on AR signaling (Figure 1) [60,61]. LXR-deficient mice fed a high cholesterol diet presented prostatic intraepithelial neoplasia (PIN) [62]. In addition, activation of LXRs by their agonists decreased prostate cancer cell proliferation and prostate tumor invasion [59,63,64,65,66,67]. Thus, these data indicate that LXRs play an antioncogenic role in prostate cancer, suggesting that selective LXR modulators could be novel prevention and therapeutic strategies for prostate cancer [68].
2.2.6. Vitamin D Receptor (VDR)
VDR is activated by vitamin D (1,25-(OH)2D3) and acts as a transcription factor by heterodimerizing with RXR, migrating into the nucleus, and binding to vitamin D responsive elements [69]. VDR has been extensively investigated in association with prostate cancer pathogenesis. High VDR expression in prostate cancer clinical samples was associated with a reduced risk of lethal cancer, suggesting an antioncogenic role of the vitamin D pathway in prostate cancer progression [70]. Numerous epidemiological studies have shown the association between the amount of dietary vitamin D, vitamin D level in circulation, and sunlight exposure with prostate cancer risk [71]. In addition, genetic polymorphisms in VDR were associated with prostate cancer susceptibility and prostate cancer progression [72,73,74]. VDR-knockout mice showed higher cell proliferation than wild-type mice [75]. Consistent with these findings, numerous studies have demonstrated the anticancer effects of vitamin D treatment [76]. Based on these preclinical studies, vitamin D compounds such as calcitriol were examined as single agents as well as in combination with cytotoxic agents such as docetaxel in clinical trials and showed some clinical response such as slowing PSA elevation [76]. The phase III ASCENT I trial was promising, which showed possible favorable antitumor effects such as PSA decline and survival by calcitriol with weekly docetaxel [77]. However, the subsequent phase III ASCENT II trial was disappointing, showing detrimental survival by calcitriol with 3-weekly docetaxel [78].
2.3. Subfamily 2
This subfamily consists of hepatocyte nuclear factor-4, RXRs, testicular orphan nuclear receptors (TRs), and COUP-TFs [3].
2.3.1. Retinoid X Receptors (RXRs)
The RXR subfamily (RXRα, RXRβ, and RXRγ) plays diverse roles as NRs because they function either as homodimers that bind to direct repeat sites in gene promoters or as heterodimers with other receptors such as PPARs, LXRs, or FXRs [79]. RXRs are activated by the potent natural ligand 9-cis-retinoic acid as well as all-trans-retinoic acid and novel ligands such as fatty acid and phytanic acid [80]. Previous studies showed that the expression of RXRα was reduced in prostate cancer compared with nonmalignant prostate [35,81,82]. Inactivation of RXRα in the prostate epithelium led to the development of preneoplastic lesions in mice [83], while RXRα overexpression caused cell growth reduction or increased susceptibility to apoptosis in prostate cancer cells [81]. Consistent with these findings, RXR agonists suppressed cell growth and multidrug resistance in prostate cancer both alone [26,84] and in combination with insulin-like growth factor binding protein-3 [85]. These data suggest that RXRs play an antioncogenic role in prostate cancer with or without interactions with other NRs.
2.3.2. Testicular Orphan Nuclear Receptors (TRs)
TRs are classified as orphan receptors but can be activated by several natural molecules, their metabolites, and synthetic compounds including polyunsaturated fatty acids and the metabolites 13-hydroxyoctadecadienoic acid and 15-hydroxyeicosatetraenoic acid, as well as the antidiabetic drug thiazolidinedione [86]. Two TRs, TR2 and TR4, control the expression of target genes and play several roles in physiological and pathological conditions [86]. Only few studies have reported on the molecular effects of TRs in prostate cancer. TR4-knockout mice developed PIN and prostate cancer, indicating that the TR4 gene is a tumor suppressor gene in prostate carcinogenesis [87]. In contrast, TR4 also plays essential functions in various processes related to prostate cancer progression such as invasion and migration as well as cellular resistance to chemotherapy and radiotherapy [88,89,90,91,92,93]. Taken together, these findings suggest complex functions of TRs in prostate cancer biology.
2.3.3. Chicken Ovalbumin Upstream Promoter-Transcription Factors (COUP-TFs)
Orphan receptor COUP-TFs repress gene expression by directly binding to direct repeat sites in genes and they also activate gene expression through forming a modulatory complex with the Sp1 transcription factor [94]. Only few studies have reported on the molecular effects of COUP-TFs in prostate cancer. Genome-wide analysis on the target genes of AR indicated a direct negative regulation of COUP-TFα by AR, in which COUP-TFα localized in the nucleus in prostate cancer epithelium but not in nonmalignant prostate epithelium [95]. COUP-TFβ also functioned as a corepressor of AR and inhibited androgen-dependent proliferation in LNCaP cells [96]. In contrast, another study indicated that COUP-TFβ expression restored cell proliferation and migration inhibited by miR-382 in PC-3, DU-145, LNCaP, and castration-resistant 22Rv1 cells [97]. Taken together, these findings suggest complex roles of COUP-TFs in prostate cancer biology.
2.4. Subfamily 3
This subfamily consists of the steroid receptors (SRs) including estrogen receptors (ERs), estrogen-related receptors (ERRs), AR, glucocorticoid receptor (GR), mineralocorticoid receptor (MR), and progesterone receptor (PR) [3]. SRs are activated by cholesterol-derived hormones and translocate into the nucleus to modulate their target gene expressions, which lead to regulation of various processes in development, metabolism, and reproduction [3]. Cholesterol-derived hormones regulate SRs through direct binding [3]. AR is a leading player in prostate cancer pathogenesis and exerts its functional effect mainly through genomic pathway (Figure 1) [1]. Numerous excellent reviews have already summarized the roles of AR [98,99] and therefore we have omitted a summary on AR in this review.
2.4.1. Estrogen Receptors (ERs)
The ER subfamily proteins (ERα and ERβ) are activated upon binding with estrogen, form a dimer and bind to estrogen response elements in the genome to regulate the expressions of target genes [100]. ERα is highly expressed in female reproductive organs, whereas ERβ is abundantly expressed in the prostate, bladder, lung, testis, brain, and bone [100]. Previous studies showed that ERα was upregulated during malignant transformation of the prostatic epithelium and in high-grade and metastatic prostate cancer as well as CRPC, in which ERα expression was increased by androgen-deprivation therapy, implicating an oncogenic role of ERα [101,102,103]. Consistent with these findings, ERα-knockout mice showed no development of high-grade PIN or prostate cancer in experimental carcinogenesis by chronic treatment with testosterone and estradiol [104]. Based on these findings, ERα inhibitors such as the antiestrogen fulvestrant and ERα antagonist toremifene were examined in early-stage clinical trials and showed potential antitumor activity in prostate cancer [105,106].
In contrast to ERα, ERβ preferentially binding to phytoestrogens is likely to protect the prostate epithelium from malignant transformation [103]. ERβ was expressed at high levels in luminal cells of the prostatic epithelium but was partly lost in high-grade PIN, suggesting that ERβ acts as a tumor suppressor [107]. In addition, ERβ expression was suppressed by androgen-deprivation therapy [108]. In studies using ERβ-knockout mice, ERβ was shown to downregulate AR signaling via inducing the AR corepressor dachshund family in the prostate [109]. Consistent with these findings, ERβ agonist was shown to suppress AR expression, resulting in decreased cell survival and increased apoptosis in androgen-dependent VCaP cells [110]. Taken together, these results suggest that ERs may be novel prevention and therapeutic targets for prostate cancer.
2.4.2. Estrogen-Related Receptors (ERRs)
The ERRs (ERRα, ERRβ, and ERRγ) share a high degree of homology with ERs within the DNA-binding domain and LBD, but ERRs do not bind to estrogen [111]. ERRα was expressed in prostate cancer [112] and its expression further increased in aggressive disease [113,114]. In addition, ERRα expression was higher in bone metastases in CRPC than in primary hormone-naïve prostate cancer [115]. These findings suggest that ERRα might play an oncogenic role in the development and progression of prostate cancer. In contrast, ERRβ and ERRγ expressions were decreased in prostate cancer and further decreased in aggressive disease [112,114,116]. Consistent with these findings, overexpression of ERRβ or ERRγ suppressed cell proliferation in prostate cancer cells, suggesting that these receptors exhibit antioncogenic functions in prostate cancer [117,118].
2.4.3. Glucocorticoid Receptor (GR)
Various subtypes of GR are derived from a single gene by alternative splicing and alternative translation initiation mechanisms [119]. Upon binding to glucocorticoids, GR translocates to the nucleus as a homodimer, binds to glucocorticoid response elements in the promoter of target genes, and regulates the expression of target genes that function in broad physiological and pathological processes such as cell growth, energy production, metabolic processes, reproduction, and immune and cardiovascular function [120]. GR expression was reduced in prostatic cancer cells to lower levels than in epithelium of BPH [121] while GR expression was increased in malignant-transformed prostate epithelial RWPE-2 cells [7], indicating controversies on GR expression in prostate cancer. Classically, glucocorticoids were shown to exert antitumor effects in prostate cancer, in which glucocorticoid suppressed adrenal androgens in men with prostate cancer [119]. In addition, the potential for glucocorticoids to promote rather than to suppress prostate cancer growth has been raised based on the structural similarity to AR [122]. In GR-overexpressing cells, glucocorticoids have been shown to activate a transcriptional program that overlaps with genes induced by AR activation (Figure 1) [123]. Therefore, GR may maintain AR signaling in androgen-deprived environments by hijacking the transcriptional program of AR in prostate cancer cells. Previous studies showed that GR expression can be negatively regulated by AR signaling and increased after castration [119,124]. Consistent with these results, some reports demonstrated that GR plays an important role in resistance to androgen-deprivation therapy [125] and the antiandrogen enzalutamide [126]. Taken together, these findings suggest complex roles of GR in prostate cancer biology.
2.4.4. Mineralocorticoid Receptor (MR)
MR is activated primarily by mineralocorticoid aldosterone, but also by glucocorticoids, and translocates to the nucleus as a homodimer where it binds to mineralocorticoid response elements in gene promoters to regulate the expression of genes involved in physiological and pathological conditions in kidney and cardiovascular systems [127]. MR is expressed in both LNCaP and PC-3 cells [128]. Mineralocorticoids such as corticosterone and deoxycorticosterone have been shown to inhibit AR activity in the presence of androgens [129]. In addition, MR suppression by siRNA or antagonists such as spironolactone and eplerenone have been shown to activate AR signaling, suggesting an antagonistic activity to AR [130,131]. Consistent with these findings, mineralocorticoids such as corticosterone and deoxycorticosterone inhibited cell proliferation in androgen-dependent LAPC-4 and LNCaP cells in the presence of androgens [129], while MR antagonists increased LNCaP cell viability [132]. Moreover, MR signaling augmented cellular sensitivity to the antiandrogen enzalutamide [131]. Inversely, the MR antagonist was suggested to promote resistance to AR-targeting therapies [133]. Intriguingly, a genetic polymorphism in MR was associated with prognosis in androgen-deprivation therapy for metastatic prostate cancer, suggesting that MR plays a key role in the resistance of prostate cancer to AR axis-targeting therapies [134].
2.4.5. Progesterone Receptor (PR)
Among the PR isoforms (PRA, PRB, and PRC), PRA and PRB are derived from a single gene by alternative transcription initiation and these proteins represent the major functional isoforms [135]. Upon binding to progesterone, PR translocates to the nucleus as a homodimer, binds to progesterone response elements in the promoter of target genes, and regulates the expression of genes involved in developmental processes as well as proliferation and differentiation during the reproductive cycle and pregnancy in female reproductive tissues [136]. PR was expressed in prostate stroma, while PR expression in the prostate epithelium is controversial [137]. However, PR expression was reduced in cancer-associated stroma [138]. Consistent with these findings, stromal PR suppressed cancer cell migration and invasion via a paracrine mechanism of the stromal cell derived factor-1 and interleukin-6 [139], suggesting an antioncogenic function of PR in stromal cells. Furthermore, the expression level of PR in cancer cells increased with Gleason score, tumor progression, and clinical failure [140,141,142]. Interestingly, PR expression was increased after androgen-deprivation therapy, suggesting a negative regulation of PR expression by AR [137]. These results suggest that PR in cancer cells and the associated stromal cells distinctly regulate prostate cancer pathogenesis.
2.5. Subfamilies 5 and 6
Subfamily 5 contains steroidogenic factor-1 (SF-1) and liver receptor homolog-1 (LRH-1), which are generally still classified as orphan receptors, but phospholipids were suggested as possible ligands. These NRs function as a monomer and are required for development and metabolism [3]. Subfamily 6 contains only one orphan receptor, germ cell nuclear factor (GCNF), which is critical for development. The few available studies on these receptors have indicated a role in prostate cancer pathogenesis [3].
SF-1, a key regulator of steroidogenesis in normal endocrine tissues, is not expressed in benign cells, but present in prostate cancer cell lines [143]. SF-1 overexpression in benign prostate cells stimulated steroidogenic enzyme expression, steroid synthesis, and cell proliferation. Furthermore, SF-1 was required for steroid-mediated cell growth in prostate cancer cells [143]. Similarly, increased expression of LRH-1 was detected in high-grade prostate cancer and CRPC xenograft models [144]. LRH-1 was shown to promote de novo androgen biosynthesis via direct transactivation of several key steroidogenic enzyme genes, resulting in elevation of intratumoral androgen levels and reactivation of AR signaling in CRPC xenografts as well as abiraterone-treated CRPC tumors [144]. Thus, these NRs may promote prostate cancer progression via regulating steroidogenesis (Figure 1). Cellular levels of GCNF expression were higher in prostate cancer compared with normal prostate and further increased in metastatic lesions and CRPC [145], suggesting an oncogenic role of GCNF via an unknown mechanism.
3. Conclusions and Future Directions
The current literature on the functions of NRs in prostate cancer indicate that DAX1, SHP, RARβ/γ, FXRs, LXRs, VDR, ERβ, ERRβ/γ, and MR can play antioncogenic roles, while PPARγ, RORγ, SF-1, LRH-1, Erα, and GR, as well as AR, can play oncogenic roles (Table 1). However, the role of other NRs in prostate cancer remains controversial or uninvestigated, suggesting a need for further research. In particular, extensive research focusing on SRs in subfamily 3 including AR and other AR-mimic SRs should be required as these NRs are considered to play critical roles in prostate cancer pathogenesis. In addition, based on the recent demonstrated findings from other NRs in prostate cancer, examination of these NRs may lead to the development of novel preventions and therapeutics for prostate cancer.
Acknowledgments
We apologize to authors whose works were inadvertently overlooked or could not be cited because of space constraints. We thank Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Abbreviations
| AR | Androgen receptor |
| BPH | Benign prostatic hyperplasia |
| COUP-TF | Chicken ovalbumin upstream promoter transcription factor |
| CRPC | Castration-resistant prostate cancer |
| DAX1 | Dosage-sensitive sex reversal-adrenal hypoplasia congenital critical region on the X chromosome, Gene 1 |
| ER | Estrogen receptor |
| ERR | Estrogen-related receptor |
| FXR | Farnesoid X receptor |
| GCNF | Germ cell nuclear factor |
| GR | Glucocorticoid receptor |
| LRH-1 | Liver receptor homolog-1 |
| LXR | Liver X receptor |
| MR | Mineralocorticoid receptor |
| NR | Nuclear receptor |
| PIN | Prostatic intraepithelial neoplasia |
| PPAR | Peroxisome proliferator activated receptor |
| PR | Progesterone receptor |
| RAR | Retinoic acid receptor |
| REV-ERB | Reverse-Erb receptor |
| ROR | Retinoic acid receptor-related orphan receptor |
| RXR | Retinoid X receptor |
| SF-1 | Steroidogenic factor-1 |
| SHP | Small heterodimer partner |
| SR | Steroid receptor |
| TR | Testicular orphan nuclear receptor |
| VDR | Vitamin D receptor |
Author Contributions
Conceptualization, M.S.; writing—original draft preparation, M.S.; writing—review and editing, N.F, E.K., and M.E.
Funding
This work was funded in part by a JSPS KAKENHI grant (17K11145).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Basu S., Tindall D.J. Androgen action in prostate cancer. Horm. Cancer. 2010;1:223–228. doi: 10.1007/s12672-010-0044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shiota M., Eto M. Current status of primary pharmacotherapy and future perspectives toward upfront therapy for metastatic hormone-sensitive prostate cancer. Int. J. Urol. 2016;23:360–369. doi: 10.1111/iju.13091. [DOI] [PubMed] [Google Scholar]
- 3.Weikum E.R., Liu X., Ortlund E.A. The nuclear receptor superfamily: A structural perspective. Protein Sci. 2018;27:1876–1892. doi: 10.1002/pro.3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nuclear Receptors Nomenclature Committee A unified nomenclature system for the nuclear receptor superfamily. Cell. 1999;97:161–163. doi: 10.1016/S0092-8674(00)80726-6. [DOI] [PubMed] [Google Scholar]
- 5.Barfeld S.J., Itkonen H.M., Urbanucci A., Mills I.G. Androgen-regulated metabolism and biosynthesis in prostate cancer. Endocr. Relat. Cancer. 2014;21:T57–T66. doi: 10.1530/ERC-13-0515. [DOI] [PubMed] [Google Scholar]
- 6.Taverna G., Pedretti E., Di Caro G., Borroni E.M., Marchesi F., Grizzi F. Inflammation and prostate cancer: Friends or foe? Inflamm. Res. 2015;64:275–286. doi: 10.1007/s00011-015-0812-2. [DOI] [PubMed] [Google Scholar]
- 7.Long M.D., Thorne J.L., Russell J., Battaglia S., Singh P.K., Sucheston-Campbell L.E., Campbell M.J. Cooperative behavior of the nuclear receptor superfamily and its deregulation in prostate cancer. Carcinogenesis. 2014;35:262–271. doi: 10.1093/carcin/bgt334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olokpa E., Moss P.E., Stewart L.V. Crosstalk between the androgen receptor and PPARγ signaling pathways in the prostate. PPAR Res. 2017;2017:9456020. doi: 10.1155/2017/9456020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agoulnik I.U., Krause W.C., Bingman W.E., 3rd., Rahman H.T., Amrikachi M., Ayala G.E., Weigel N.L. Repressors of androgen and progesterone receptor action. J. Biol. Chem. 2003;278:31136–31148. doi: 10.1074/jbc.M305153200. [DOI] [PubMed] [Google Scholar]
- 10.Holter E., Kotaja N., Mäkela S., Strauss L., Kietz S., Jänne O.A., Gustafsson J.A., Palvimo J.J., Treuter E. Inhibition of androgen receptor (AR) function by the reproductive orphan nuclear receptor DAX-1. Mol. Endocrinol. 2002;16:515–528. doi: 10.1210/mend.16.3.0804. [DOI] [PubMed] [Google Scholar]
- 11.Lee M.Y., Lu A., Gudas L.J. Transcriptional regulation of Rex1 (zfp42) in normal prostate epithelial cells and prostate cancer cells. J. Cell. Physiol. 2010;224:17–27. doi: 10.1002/jcp.22071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakamura Y., Suzuki T., Arai Y., Sasano H. Nuclear receptor DAX1 in human prostate cancer: A novel independent biological modulator. Endocr. J. 2009;56:39–44. doi: 10.1507/endocrj.K08E-177. [DOI] [PubMed] [Google Scholar]
- 13.Ehrlund A., Treuter E. Ligand-independent actions of the orphan receptors/corepressors DAX-1 and SHP in metabolism, reproduction and disease. J. Steroid Biochem. Mol. Biol. 2012;130:169–179. doi: 10.1016/j.jsbmb.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Xiao J., Gong A.Y., Eischeid A.N., Chen D., Deng C., Young C.Y., Chen X.M. miR-141 modulates androgen receptor transcriptional activity in human prostate cancer cells through targeting the small heterodimer partner protein. Prostate. 2012;72:1514–1522. doi: 10.1002/pros.22501. [DOI] [PubMed] [Google Scholar]
- 15.Khorasani M., Teimoori-Toolabi L., Farivar T.N., Asgari M., Abolhasani M., Shahrokh H., Afgar A., Kalantari E., Peymani A., Mahdian R. Aberrant expression of miR-141 and nuclear receptor small heterodimer partner in clinical samples of prostate cancer. Cancer Biomark. 2018;22:19–28. doi: 10.3233/CBM-170696. [DOI] [PubMed] [Google Scholar]
- 16.Tassidis H., Brokken L.J., Jirström K., Ehrnström R., Pontén F., Ulmert D., Bjartell A., Härkönen P., Wingren A.G. Immunohistochemical detection of tyrosine phosphatase SHP-1 predicts outcome after radical prostatectomy for localized prostate cancer. Int. J. Cancer. 2010;126:2296–2307. doi: 10.1002/ijc.24917. [DOI] [PubMed] [Google Scholar]
- 17.Dawson M.I., Xia Z., Liu G., Ye M., Fontana J.A., Farhana L., Patel B.B., Arumugarajah S., Bhuiyan M., Zhang X.K., et al. An adamantyl-substituted retinoid-derived molecule that inhibits cancer cell growth and angiogenesis by inducing apoptosis and binds to small heterodimer partner nuclear receptor: Effects of modifying its carboxylate group on apoptosis, proliferation, and protein-tyrosine phosphatase activity. J. Med. Chem. 2007;50:2622–2639. doi: 10.1021/jm0613323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tassidis H., Culig Z., Wingren A.G., Härkönen P. Role of the protein tyrosine phosphatase SHP-1 in Interleukin-6 regulation of prostate cancer cells. Prostate. 2010;70:1491–1500. doi: 10.1002/pros.21184. [DOI] [PubMed] [Google Scholar]
- 19.Rodríguez-Ubreva F.J., Cariaga-Martinez A.E., Cortés M.A., Romero-De Pablos M., Ropero S., López-Ruiz P., Colás B. Knockdown of protein tyrosine phosphatase SHP-1 inhibits G1/S progression in prostate cancer cells through the regulation of components of the cell-cycle machinery. Oncogene. 2010;29:345–355. doi: 10.1038/onc.2009.329. [DOI] [PubMed] [Google Scholar]
- 20.Di Masi A., Leboffe L., De Marinis E., Pagano F., Cicconi L., Rochette-Egly C., Lo-Coco F., Ascenzi P., Nervi C. Retinoic acid receptors: From molecular mechanisms to cancer therapy. Mol. Asp. Med. 2015;41:1–115. doi: 10.1016/j.mam.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Taylor B.S., Schultz N., Hieronymus H., Gopalan A., Xiao Y., Carver B.S., Arora V.K., Kaushik P., Cerami E., Reva B., et al. Integrative genomic profiling of human prostate cancer. Cancer Cell. 2010;18:11–22. doi: 10.1016/j.ccr.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cancer Genome Atlas Research Network The molecular taxonomy of primary prostate cancer. Cell. 2015;163:1011–1025. doi: 10.1016/j.cell.2015.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dou M., Zhou X., Fan Z., Ding X., Li L., Wang S., Xue W., Wang H., Suo Z., Deng X. Clinical significance of retinoic acid receptor β promoter methylation in prostate cancer: A meta-analysis. Cell. Physiol. Biochem. 2018;45:2497–2505. doi: 10.1159/000488268. [DOI] [PubMed] [Google Scholar]
- 24.Dahiya R., Park H.D., Cusick J., Vessella R.L., Fournier G., Narayan P. Inhibition of tumorigenic potential and prostate-specific antigen expression in LNCaP human prostate cancer cell line by 13-cis-retinoic acid. Int. J. Cancer. 1994;59:126–132. doi: 10.1002/ijc.2910590122. [DOI] [PubMed] [Google Scholar]
- 25.Long M.D., Singh P.K., Russell J.R., Llimos G., Rosario S., Rizvi A., van den Berg P.R., Kirk J., Sucheston-Campbell L.E., Smiraglia D.J., et al. The miR-96 and RARγ signaling axis governs androgen signaling and prostate cancer progression. Oncogene. 2019;38:421–444. doi: 10.1038/s41388-018-0450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Vos S., Dawson M.I., Holden S., Le T., Wang A., Cho S.K., Chen D.L., Koeffler H.P. Effects of retinoid X receptor-selective ligands on proliferation of prostate cancer cells. Prostate. 1997;32:115–121. doi: 10.1002/(SICI)1097-0045(19970701)32:2<115::AID-PROS6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 27.Kucukzeybek Y., Gul M.K., Cengiz E., Erten C., Karaca B., Gorumlu G., Atmaca H., Uzunoglu S., Karabulut B., Sanli U.A., et al. Enhancement of docetaxel-induced cytotoxicity and apoptosis by all-trans retinoic acid (ATRA) through downregulation of survivin (BIRC5), MCL-1 and LTβ-R in hormone- and drug resistant prostate cancer cell line, DU-145. J. Exp. Clin. Cancer Res. 2008;27:37. doi: 10.1186/1756-9966-27-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karabulut B., Karaca B., Atmaca H., Kisim A., Uzunoglu S., Sezgin C., Uslu R. Regulation of apoptosis-related molecules by synergistic combination of all-trans retinoic acid and zoledronic acid in hormone-refractory prostate cancer cell lines. Mol. Biol. Rep. 2011;38:249–259. doi: 10.1007/s11033-010-0102-6. [DOI] [PubMed] [Google Scholar]
- 29.Liu Z., Ren G., Shangguan C., Guo L., Dong Z., Li Y., Zhang W., Zhao L., Hou P., Zhang Y., et al. ATRA inhibits the proliferation of DU145 prostate cancer cells through reducing the methylation level of HOXB13 gene. PLoS ONE. 2012;7:e40943. doi: 10.1371/journal.pone.0040943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu X.P., Fanjul A., Picard N., Shroot B., Pfahl M. A selective retinoid with high activity against an androgen-resistant prostate cancer cell type. Int. J. Cancer. 1999;80:272–278. doi: 10.1002/(SICI)1097-0215(19990118)80:2<272::AID-IJC17>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 31.Campbell M.J., Park S., Uskokovic M.R., Dawson M.I., Koeffler H.P. Expression of retinoic acid receptor-β sensitizes prostate cancer cells to growth inhibition mediated by combinations of retinoids and a 19-nor hexafluoride vitamin D3 analog. Endocrinology. 1998;139:1972–1980. doi: 10.1210/endo.139.4.5943. [DOI] [PubMed] [Google Scholar]
- 32.Derosa G., Sahebkar A., Maffioli P. The role of various peroxisome proliferator-activated receptors and their ligands in clinical practice. J. Cell. Physiol. 2018;233:153–161. doi: 10.1002/jcp.25804. [DOI] [PubMed] [Google Scholar]
- 33.Mirza A.Z., Althagafi I.I., Shamshad H. Role of PPAR receptor in different diseases and their ligands: Physiological importance and clinical implications. Eur. J. Med. Chem. 2019;166:502–513. doi: 10.1016/j.ejmech.2019.01.067. [DOI] [PubMed] [Google Scholar]
- 34.Segawa Y., Yoshimura R., Hase T., Nakatani T., Wada S., Kawahito Y., Kishimoto T., Sano H. Expression of peroxisome proliferator-activated receptor (PPAR) in human prostate cancer. Prostate. 2002;51:108–116. doi: 10.1002/pros.10058. [DOI] [PubMed] [Google Scholar]
- 35.Rogenhofer S., Ellinger J., Kahl P., Stoehr C., Hartmann A., Engehausen D., Wieland W.F., Müller S.C., Hofstädter F., Walter B. Enhanced expression of peroxisome proliferate-activated receptor γ (PPAR-γ) in advanced prostate cancer. Anticancer Res. 2012;32:3479–3483. [PubMed] [Google Scholar]
- 36.Forootan F.S., Forootan S.S., Malki M.I., Chen D., Li G., Lin K., Rudland P.S., Foster C.S., Ke Y. The expression of C-FABP and PPARγ and their prognostic significance in prostate cancer. Int. J. Oncol. 2014;44:265–275. doi: 10.3892/ijo.2013.2166. [DOI] [PubMed] [Google Scholar]
- 37.Elix C., Pal S.K., Jones J.O. The role of peroxisome proliferator-activated receptor γ in prostate cancer. Asian J. Androl. 2018;20:238–243. doi: 10.4103/aja.aja_15_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moss P.E., Lyles B.E., Stewart L.V. The PPARγ ligand ciglitazone regulates androgen receptor activation differently in androgen-dependent versus androgen-independent human prostate cancer cells. Exp. Cell Res. 2010;316:3478–3488. doi: 10.1016/j.yexcr.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Forootan F.S., Forootan S.S., Gou X., Yang J., Liu B., Chen D., Al Fayi M.S., Al-Jameel W., Rudland P.S., Hussain S.A., et al. Fatty acid activated PPARγ promotes tumorigenicity of prostate cancer cells by up regulating VEGF via PPAR responsive elements of the promoter. Oncotarget. 2016;7:9322–9339. doi: 10.18632/oncotarget.6975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmad I., Mui E., Galbraith L., Patel R., Tan E.H., Salji M., Rust A.G., Repiscak P., Hedley A., Markert E., et al. Sleeping Beauty screen reveals Pparg activation in metastatic prostate cancer. Proc. Natl. Acad. Sci. USA. 2016;113:8290–8295. doi: 10.1073/pnas.1601571113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tew B.Y., Hong T.B., Otto-Duessel M., Elix C., Castro E., He M., Wu X., Pal S.K., Kalkum M., Jones J.O. Vitamin K epoxide reductase regulation of androgen receptor activity. Oncotarget. 2017;8:13818–13831. doi: 10.18632/oncotarget.14639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sikka S., Chen L., Sethi G., Kumar A.P. Targeting PPARγ signaling cascade for the prevention and treatment of prostate cancer. PPAR Res. 2012;2012:968040. doi: 10.1155/2012/968040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olokpa E., Bolden A., Stewart L.V. The androgen receptor regulates PPARγ expression and activity in human prostate cancer cells. J. Cell. Physiol. 2016;231:2664–2672. doi: 10.1002/jcp.25368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stephen R.L., Gustafsson M.C., Jarvis M., Tatoud R., Marshall B.R., Knight D., Ehrenborg E., Harris A.L., Wolf C.R., Palmer C.N. Activation of peroxisome proliferator-activated receptor delta stimulates the proliferation of human breast and prostate cancer cell lines. Cancer Res. 2004;64:3162–3170. doi: 10.1158/0008-5472.CAN-03-2760. [DOI] [PubMed] [Google Scholar]
- 45.Wu T.T., Niu H.S., Chen L.J., Cheng J.T., Tong Y.C. Increase of human prostate cancer cell (DU145) apoptosis by telmisartan through PPAR-δ pathway. Eur. J. Pharmacol. 2016;775:35–42. doi: 10.1016/j.ejphar.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 46.Martín-Martín N., Zabala-Letona A., Fernández-Ruiz S., Arreal L., Camacho L., Castillo-Martin M., Cortazar A.R., Torrano V., Astobiza I., Zúñiga-García P., et al. PPARδ elicits ligand-independent repression of trefoil factor family to limit prostate cancer growth. Cancer Res. 2018;78:399–409. doi: 10.1158/0008-5472.CAN-17-0908. [DOI] [PubMed] [Google Scholar]
- 47.Solt L.A., Griffin P.R., Burris T.P. Ligand regulation of retinoic acid receptor-related orphan receptors: Implications for development of novel therapeutics. Curr. Opin. Lipidol. 2010;21:204–211. doi: 10.1097/MOL.0b013e328338ca18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Santori F.R., Huang P., van de Pavert S.A., Douglass E.F., Jr., Leaver D.J., Haubrich B.A., Keber R., Lorbek G., Konijn T., Rosales B.N., et al. Identification of natural RORγ ligands that regulate the development of lymphoid cells. Cell Metab. 2015;21:286–298. doi: 10.1016/j.cmet.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang J., Zou J.X., Xue X., Cai D., Zhang Y., Duan Z., Xiang Q., Yang J.C., Louie M.C., Borowsky A.D., et al. ROR-γ drives androgen receptor expression and represents a therapeutic target in castration-resistant prostate cancer. Nat. Med. 2016;22:488–496. doi: 10.1038/nm.4070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Y., Wu X., Xue X., Li C., Wang J., Wang R., Zhang C., Wang C., Shi Y., Zou L., et al. Discovery and characterization of XY101, a potent, selective, and orally bioavailable RORγ inverse agonist for treatment of castration-resistant prostate cancer. J. Med. Chem. 2019;62:4716–4730. doi: 10.1021/acs.jmedchem.9b00327. [DOI] [PubMed] [Google Scholar]
- 51.Moretti R.M., Montagnani Marelli M., Motta M., Limonta P. Role of the orphan nuclear receptor ROR α in the control of the metastatic behavior of androgen-independent prostate cancer cells. Oncol. Rep. 2002;9:1139–1143. [PubMed] [Google Scholar]
- 52.Park S.C., Park I.G., Kim H., Lee J.M. N-terminal domain mediated regulation of RORα1 inhibits invasive growth in prostate cancer. Int. J. Mol. Sci. 2019;20:1684. doi: 10.3390/ijms20071684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Han C.Y. Update on FXR biology: Promising therapeutic target? Int. J. Mol. Sci. 2018;19:2069. doi: 10.3390/ijms19072069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu J., Tong S.J., Wang X., Qu L.X. Farnesoid X receptor inhibits LNcaP cell proliferation via the upregulation of PTEN. Exp. Ther. Med. 2014;8:1209–1212. doi: 10.3892/etm.2014.1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu N., Zhao J., Wang J., Teng H., Fu Y., Yuan H. Farnesoid X receptor ligand CDCA suppresses human prostate cancer cells growth by inhibiting lipid metabolism via targeting sterol response element binding protein 1. Am. J. Transl. Res. 2016;8:5118–5124. [PMC free article] [PubMed] [Google Scholar]
- 56.Choi Y.H., Im E.O., Suh H., Jin Y., Yoo Y.H., Kim N.D. Apoptosis and modulation of cell cycle control by synthetic derivatives of ursodeoxycholic acid and chenodeoxycholic acid in human prostate cancer cells. Cancer Lett. 2003;199:157–167. doi: 10.1016/S0304-3835(03)00351-3. [DOI] [PubMed] [Google Scholar]
- 57.Schulman I.G. Liver X receptors link lipid metabolism and inflammation. FEBS Lett. 2017;591:2978–2991. doi: 10.1002/1873-3468.12702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Viennois E., Esposito T., Dufour J., Pommier A., Fabre S., Kemeny J.L., Guy L., Morel L., Lobaccaro J.M., Baron S. Lxrα regulates the androgen response in prostate epithelium. Endocrinology. 2012;153:3211–3223. doi: 10.1210/en.2011-1996. [DOI] [PubMed] [Google Scholar]
- 59.Chuu C.P., Hiipakka R.A., Kokontis J.M., Fukuchi J., Chen R.Y., Liao S. Inhibition of tumor growth and progression of LNCaP prostate cancer cells in athymic mice by androgen and liver X receptor agonist. Cancer Res. 2006;66:6482–6486. doi: 10.1158/0008-5472.CAN-06-0632. [DOI] [PubMed] [Google Scholar]
- 60.Chuu C.P., Chen R.Y., Hiipakka R.A., Kokontis J.M., Warner K.V., Xiang J., Liao S. The liver X receptor agonist T0901317 acts as androgen receptor antagonist in human prostate cancer cells. Biochem. Biophys. Res. Commun. 2007;357:341–346. doi: 10.1016/j.bbrc.2007.03.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tsui K.H., Chung L.C., Feng T.H., Lee T.Y., Chang P.L., Chen W.T., Juang H.H. Divergent effect of liver X receptor agonists on prostate-specific antigen expression is dependent on androgen receptor in prostate carcinoma cells. Prostate. 2015;75:603–615. doi: 10.1002/pros.22944. [DOI] [PubMed] [Google Scholar]
- 62.Pommier A.J., Dufour J., Alves G., Viennois E., De Boussac H., Trousson A., Volle D.H., Caira F., Val P., Arnaud P., et al. Liver x receptors protect from development of prostatic intra-epithelial neoplasia in mice. PLoS Genet. 2013;9:e1003483. doi: 10.1371/journal.pgen.1003483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fukuchi J., Kokontis J.M., Hiipakka R.A., Chuu C.P., Liao S. Antiproliferative effect of liver X receptor agonists on LNCaP human prostate cancer cells. Cancer Res. 2004;64:7686–7689. doi: 10.1158/0008-5472.CAN-04-2332. [DOI] [PubMed] [Google Scholar]
- 64.Chuu C.P., Kokontis J.M., Hiipakka R.A., Liao S. Modulation of liver X receptor signaling as novel therapy for prostate cancer. J. Biomed. Sci. 2007;14:543–553. doi: 10.1007/s11373-007-9160-8. [DOI] [PubMed] [Google Scholar]
- 65.Pommier A.J., Alves G., Viennois E., Bernard S., Communal Y., Sion B., Marceau G., Damon C., Mouzat K., Caira F., et al. Liver X receptor activation downregulates AKT survival signaling in lipid rafts and induces apoptosis of prostate cancer cells. Oncogene. 2010;29:2712–2723. doi: 10.1038/onc.2010.30. [DOI] [PubMed] [Google Scholar]
- 66.Fu W., Yao J., Huang Y., Li Q., Li W., Chen Z., He F., Zhou Z., Yan J. LXR agonist regulates the carcinogenesis of PCa via the SOCS3 pathway. Cell. Physiol. Biochem. 2014;33:195–204. doi: 10.1159/000356662. [DOI] [PubMed] [Google Scholar]
- 67.Youlin K., Li Z., Weiyang H., Jian K., Siming L., Xin G. Liver X receptor activation inhibits PC-3 prostate cancer cells via the β-catenin pathway. Pathol. Res. Pract. 2017;213:267–270. doi: 10.1016/j.prp.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 68.Bousset L., Rambur A., Fouache A., Bunay J., Morel L., Lobaccaro J.A., Baron S., Trousson A., de Joussineau C. New insights in prostate cancer development and tumor therapy: Modulation of nuclear receptors and the specific role of Liver X receptors. Int. J. Mol. Sci. 2018;19:2545. doi: 10.3390/ijms19092545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Silvagno F., Pescarmona G. Spotlight on vitamin D receptor, lipid metabolism and mitochondria: Some preliminary emerging issues. Mol. Cell. Endocrinol. 2017;450:24–31. doi: 10.1016/j.mce.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 70.Hendrickson W.K., Flavin R., Kasperzyk J.L., Fiorentino M., Fang F., Lis R., Fiore C., Penney K.L., Ma J., Kantoff P.W., et al. Vitamin D receptor protein expression in tumor tissue and prostate cancer progression. J. Clin. Oncol. 2011;29:2378–2385. doi: 10.1200/JCO.2010.30.9880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gupta D., Lammersfeld C.A., Trukova K., Lis C.G. Vitamin D and prostate cancer risk: A review of the epidemiological literature. Prostate Cancer Prostatic Dis. 2009;12:215–226. doi: 10.1038/pcan.2009.7. [DOI] [PubMed] [Google Scholar]
- 72.McCullough M.L., Bostick R.M., Mayo T.L. Vitamin D gene pathway polymorphisms and risk of colorectal, breast, and prostate cancer. Annu. Rev. Nutr. 2009;29:111–132. doi: 10.1146/annurev-nutr-080508-141248. [DOI] [PubMed] [Google Scholar]
- 73.Chen L., Davey Smith G., Evans D.M., Cox A., Lawlor D.A., Donovan J., Yuan W., Day I.N., Martin R.M., Lane A., et al. Genetic variants in the vitamin d receptor are associated with advanced prostate cancer at diagnosis: Findings from the prostate testing for cancer and treatment study and a systematic review. Cancer Epidemiol. Biomark. Prev. 2009;18:2874–2881. doi: 10.1158/1055-9965.EPI-09-0544. [DOI] [PubMed] [Google Scholar]
- 74.Lin V.C., Huang S.P., Ting H.J., Ma W.L., Yu C.C., Huang C.Y., Yin H.L., Huang T.Y., Lee C.H., Chang T.Y., et al. Vitamin D receptor-binding site variants affect prostate cancer progression. Oncotarget. 2017;8:74119–74128. doi: 10.18632/oncotarget.18271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mordan-McCombs S., Brown T., Wang W.L., Gaupel A.C., Welsh J., Tenniswood M. Tumor progression in the LPB-Tag transgenic model of prostate cancer is altered by vitamin D receptor and serum testosterone status. J. Steroid Biochem. Mol. Biol. 2010;121:368–371. doi: 10.1016/j.jsbmb.2010.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Trump D.L., Aragon-Ching J.B. Vitamin D in prostate cancer. Asian J. Androl. 2018;20:244–252. doi: 10.4103/aja.aja_14_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Beer T.M., Ryan C.W., Venner P.M., Petrylak D.P., Chatta G.S., Ruether J.D., Redfern C.H., Fehrenbacher L., Saleh M.N., Waterhouse D.M., et al. Double-blinded randomized study of high-dose calcitriol plus docetaxel compared with placebo plus docetaxel in androgen-independent prostate cancer: A report from the ASCENT Investigators. J. Clin. Oncol. 2007;25:669–674. doi: 10.1200/JCO.2006.06.8197. [DOI] [PubMed] [Google Scholar]
- 78.Scher H.I., Jia X., Chi K., de Wit R., Berry W.R., Albers P., Henick B., Waterhouse D., Ruether D.J., Rosen P.J., et al. Randomized, open-label phase III trial of docetaxel plus high-dose calcitriol versus docetaxel plus prednisone for patients with castration-resistant prostate cancer. J. Clin. Oncol. 2011;29:2191–2198. doi: 10.1200/JCO.2010.32.8815. [DOI] [PubMed] [Google Scholar]
- 79.Watanabe M., Kakuta H. Retinoid X receptor antagonists. Int. J. Mol. Sci. 2018;19:2354. doi: 10.3390/ijms19082354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Krężel W., Rühl R., de Lera A.R. Alternative retinoid X receptor (RXR) ligands. Mol. Cell. Endocrinol. 2019 doi: 10.1016/j.mce.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 81.Zhong C., Yang S., Huang J., Cohen M.B., Roy-Burman P. Aberration in the expression of the retinoid receptor, RXRα, in prostate cancer. Cancer Biol. Ther. 2003;2:179–184. doi: 10.4161/cbt.2.2.281. [DOI] [PubMed] [Google Scholar]
- 82.Mao G.E., Reuter V.E., Cordon-Cardo C., Dalbagni G., Scher H.I., DeKernion J.B., Zhang Z.F., Rao J. Decreased retinoid X receptor-α protein expression in basal cells occurs in the early stage of human prostate cancer development. Cancer Epidemiol. Biomark. Prev. 2004;13:383–390. [PubMed] [Google Scholar]
- 83.Huang J., Powell W.C., Khodavirdi A.C., Wu J., Makita T., Cardiff R.D., Cohen M.B., Sucov H.M., Roy-Burman P. Prostatic intraepithelial neoplasia in mice with conditional disruption of the retinoid X receptor α allele in the prostate epithelium. Cancer Res. 2002;62:4812–4819. [PubMed] [Google Scholar]
- 84.Yen W.C., Lamph W.W. A selective retinoid X receptor agonist bexarotene (LGD1069, Targretin) prevents and overcomes multidrug resistance in advanced prostate cancer. Prostate. 2006;66:305–316. doi: 10.1002/pros.20347. [DOI] [PubMed] [Google Scholar]
- 85.Liu B., Lee K.W., Li H., Ma L., Lin G.L., Chandraratna R.A., Cohen P. Combination therapy of insulin-like growth factor binding protein-3 and retinoid X receptor ligands synergize on prostate cancer cell apoptosis in vitro and in vivo. Clin. Cancer Res. 2005;11:4851–4856. doi: 10.1158/1078-0432.CCR-04-2160. [DOI] [PubMed] [Google Scholar]
- 86.Lin S.J., Yang D.R., Yang G., Lin C.Y., Chang H.C., Li G., Chang C. TR2 and TR4 orphan nuclear receptors: An overview. Curr. Top. Dev. Biol. 2017;125:357–373. doi: 10.1016/bs.ctdb.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 87.Lin S.J., Lee S.O., Lee Y.F., Miyamoto H., Yang D.R., Li G., Chang C. TR4 nuclear receptor functions as a tumor suppressor for prostate tumorigenesis via modulation of DNA damage/repair system. Carcinogenesis. 2014;35:1399–1406. doi: 10.1093/carcin/bgu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yang D.R., Ding X.F., Luo J., Shan Y.X., Wang R., Lin S.J., Li G., Huang C.K., Zhu J., Chen Y., et al. Increased chemosensitivity via targeting testicular nuclear receptor 4 (TR4)-Oct4-interleukin 1 receptor antagonist (IL1Ra) axis in prostate cancer CD133+ stem/progenitor cells to battle prostate cancer. J. Biol. Chem. 2013;288:16476–16483. doi: 10.1074/jbc.M112.448142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen B., Yu S., Ding X., Jing C., Xia L., Wang M., Matro E., Rehman F., Niu Y., Li G., et al. The role of testicular nuclear receptor 4 in chemo-resistance of docetaxel in castration-resistant prostate cancer. Cancer Gene Ther. 2014;21:411–415. doi: 10.1038/cgt.2014.41. [DOI] [PubMed] [Google Scholar]
- 90.Yu S., Wang M., Ding X., Xia L., Chen B., Chen Y., Zhang Z., Niu Y., Li G., Chang C. Testicular orphan nuclear receptor 4 is associated with the radio-sensitivity of prostate cancer. Prostate. 2015;75:1632–1642. doi: 10.1002/pros.23044. [DOI] [PubMed] [Google Scholar]
- 91.Ding X., Yang D.R., Lee S.O., Chen Y.L., Xia L., Lin S.J., Yu S., Niu Y.J., Li G., Chang C. TR4 nuclear receptor promotes prostate cancer metastasis via upregulation of CCL2/CCR2 signaling. Int. J. Cancer. 2015;136:955–964. doi: 10.1002/ijc.29049. [DOI] [PubMed] [Google Scholar]
- 92.Zhu J., Yang D.R., Sun Y., Qiu X., Chang H.C., Li G., Shan Y., Chang C. TR4 nuclear receptor alters the prostate cancer CD133+ stem/progenitor cell invasion via modulating the EZH2-related metastasis gene expression. Mol. Cancer Ther. 2015;14:1445–1453. doi: 10.1158/1535-7163.MCT-14-0971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Qiu X., Zhu J., Sun Y., Fan K., Yang D.R., Li G., Yang G., Chang C. TR4 nuclear receptor increases prostate cancer invasion via decreasing the miR-373-3p expression to alter TGFβR2/p-Smad3 signals. Oncotarget. 2015;6:15397–15409. doi: 10.18632/oncotarget.3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tang K., Tsai S.Y., Tsai M.J. COUP-TFs and eye development. Biochim. Biophys. Acta. 2015;1849:201–209. doi: 10.1016/j.bbagrm.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Perets R., Kaplan T., Stein I., Hidas G., Tayeb S., Avraham E., Ben-Neriah Y., Simon I., Pikarsky E. Genome-wide analysis of androgen receptor targets reveals COUP-TF1 as a novel player in human prostate cancer. PLoS ONE. 2012;7:e46467. doi: 10.1371/journal.pone.0046467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Song C.H., Lee H.J., Park E., Lee K. The chicken ovalbumin upstream promoter-transcription factor II negatively regulates the transactivation of androgen receptor in prostate cancer cells. PLoS ONE. 2012;7:e49026. doi: 10.1371/journal.pone.0049026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang W., Liu J., Qiu J., Fu X., Tang Q., Yang F., Zhao Z., Wang H. MicroRNA-382 inhibits prostate cancer cell proliferation and metastasis through targeting COUP-TFII. Oncol. Rep. 2016;36:3707–3715. doi: 10.3892/or.2016.5141. [DOI] [PubMed] [Google Scholar]
- 98.Shiota M., Yokomizo A., Naito S. Increased androgen receptor transcription: A cause of castration-resistant prostate cancer and a possible therapeutic target. J. Mol. Endocrinol. 2011;47:R25–R41. doi: 10.1530/JME-11-0018. [DOI] [PubMed] [Google Scholar]
- 99.Shiota M., Yokomizo A., Naito S. Oxidative stress and androgen receptor signaling in the development and progression of castration-resistant prostate cancer. Free Radic. Biol. Med. 2011;51:1320–1328. doi: 10.1016/j.freeradbiomed.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 100.Ikeda K., Horie-Inoue K., Inoue S. Functions of estrogen and estrogen receptor signaling on skeletal muscle. J. Steroid Biochem. Mol. Biol. 2019 doi: 10.1016/j.jsbmb.2019.105375. [DOI] [PubMed] [Google Scholar]
- 101.Bonkhoff H., Fixemer T., Hunsicker I., Remberger K. Estrogen receptor expression in prostate cancer and premalignant prostatic lesions. Am. J. Pathol. 1999;155:641–647. doi: 10.1016/S0002-9440(10)65160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shaw G.L., Whitaker H., Corcoran M., Dunning M.J., Luxton H., Kay J., Massie C.E., Miller J.L., Lamb A.D., Ross-Adams H., et al. The early effects of rapid androgen deprivation on human prostate cancer. Eur. Urol. 2016;70:214–218. doi: 10.1016/j.eururo.2015.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bonkhoff H. Estrogen receptor signaling in prostate cancer: Implications for carcinogenesis and tumor progression. Prostate. 2018;78:2–10. doi: 10.1002/pros.23446. [DOI] [PubMed] [Google Scholar]
- 104.Ricke W.A., McPherson S.J., Bianco J.J., Cunha G.R., Wang Y., Risbridger G.P. Prostatic hormonal carcinogenesis is mediated by in situ estrogen production and estrogen receptor α signaling. FASEB J. 2008;22:1512–1520. doi: 10.1096/fj.07-9526com. [DOI] [PubMed] [Google Scholar]
- 105.Gasent Blesa J.M., Alberola Candel V., Giner Marco V., Giner-Bosch V., Provencio Pulla M., Laforga Canales J.B. Experience with fulvestrant acetate in castration-resistant prostate cancer patients. Ann. Oncol. 2010;21:1131–1132. doi: 10.1093/annonc/mdq010. [DOI] [PubMed] [Google Scholar]
- 106.Fujimura T., Takahashi S., Kume H., Urano T., Takayama K., Yamada Y., Suzuki M., Fukuhara H., Nakagawa T., Inoue S., et al. Toremifene, a selective estrogen receptor modulator, significantly improved biochemical recurrence in bone metastatic prostate cancer: A randomized controlled phase II a trial. BMC Cancer. 2015;15:836. doi: 10.1186/s12885-015-1871-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fixemer T., Remberger K., Bonkhoff H. Differential expression of the estrogen receptor β (ERβ) in human prostate tissue, premalignant changes, and in primary, metastatic, and recurrent prostatic adenocarcinoma. Prostate. 2003;54:79–87. doi: 10.1002/pros.10171. [DOI] [PubMed] [Google Scholar]
- 108.Chang W.Y., Prins G.S. Estrogen receptor-β: Implications for the prostate gland. Prostate. 1999;40:115–124. doi: 10.1002/(SICI)1097-0045(19990701)40:2<115::AID-PROS7>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 109.Wu W.F., Maneix L., Insunza J., Nalvarte I., Antonson P., Kere J., Yu N.Y., Tohonen V., Katayama S., Einarsdottir E., et al. Estrogen receptor β, a regulator of androgen receptor signaling in the mouse ventral prostate. Proc. Natl. Acad. Sci. USA. 2017;114:E3816–E3822. doi: 10.1073/pnas.1702211114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gehrig J., Kaulfuß S., Jarry H., Bremmer F., Stettner M., Burfeind P., Thelen P. Prospects of estrogen receptor β activation in the treatment of castration-resistant prostate cancer. Oncotarget. 2017;8:34971–34979. doi: 10.18632/oncotarget.16496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Misawa A., Inoue S. Estrogen-related receptors in breast cancer and prostate cancer. Front. Endocrinol. 2015;6:83. doi: 10.3389/fendo.2015.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cheung C.P., Yu S., Wong K.B., Chan L.W., Lai F.M., Wang X., Suetsugi M., Chen S., Chan F.L. Expression and functional study of estrogen receptor-related receptors in human prostatic cells and tissues. J. Clin. Endocrinol. Metab. 2005;90:1830–1844. doi: 10.1210/jc.2004-1421. [DOI] [PubMed] [Google Scholar]
- 113.Fujimura T., Takahashi S., Urano T., Kumagai J., Ogushi T., Horie-Inoue K., Ouchi Y., Kitamura T., Muramatsu M., Inoue S. Increased expression of estrogen-related receptor α (ERRα) is a negative prognostic predictor in human prostate cancer. Int. J. Cancer. 2007;120:2325–2330. doi: 10.1002/ijc.22363. [DOI] [PubMed] [Google Scholar]
- 114.Fujimura T., Takahashi S., Urano T., Ijichi N., Ikeda K., Kumagai J., Murata T., Takayama K., Horie-Inoue K., Ouchi Y., et al. Differential expression of estrogen-related receptors β and γ (ERRβ and ERRγ) and their clinical significance in human prostate cancer. Cancer Sci. 2010;101:646–651. doi: 10.1111/j.1349-7006.2009.01451.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fradet A., Bouchet M., Delliaux C., Gervais M., Kan C., Benetollo C., Pantano F., Vargas G., Bouazza L., Croset M., et al. Estrogen related receptor α in castration-resistant prostate cancer cells promotes tumor progression in bone. Oncotarget. 2016;7:77071–77086. doi: 10.18632/oncotarget.12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Audet-Walsh É., Yee T., McGuirk S., Vernier M., Ouellet C., St-Pierre J., Giguère V. Androgen-dependent repression of ERRγ reprograms metabolism in prostate cancer. Cancer Res. 2017;77:378–389. doi: 10.1158/0008-5472.CAN-16-1204. [DOI] [PubMed] [Google Scholar]
- 117.Yu S., Wong Y.C., Wang X.H., Ling M.T., Ng C.F., Chen S., Chan F.L. Orphan nuclear receptor estrogen-related receptor-β suppresses in vitro and in vivo growth of prostate cancer cells via p21(WAF1/CIP1) induction and as a potential therapeutic target in prostate cancer. Oncogene. 2008;27:3313–3328. doi: 10.1038/sj.onc.1210986. [DOI] [PubMed] [Google Scholar]
- 118.Ijichi N., Shigekawa T., Ikeda K., Horie-Inoue K., Fujimura T., Tsuda H., Osaki A., Saeki T., Inoue S. Estrogen-related receptor γ modulates cell proliferation and estrogen signaling in breast cancer. J. Steroid Biochem. Mol. Biol. 2011;123:1–7. doi: 10.1016/j.jsbmb.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 119.Hu J., Chen Q. The role of glucocorticoid receptor in prostate cancer progression: From bench to bedside. Int. Urol. Nephrol. 2017;49:369–380. doi: 10.1007/s11255-016-1476-8. [DOI] [PubMed] [Google Scholar]
- 120.Ide H., Inoue S., Miyamoto H. The role of glucocorticoid receptor signaling in bladder cancer progression. Cancers. 2018;10:484. doi: 10.3390/cancers10120484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mohler J.L., Chen Y., Hamil K., Hall S.H., Cidlowski J.A., Wilson E.M., French F.S., Sar M. Androgen and glucocorticoid receptors in the stroma and epithelium of prostatic hyperplasia and carcinoma. Clin. Cancer Res. 1996;2:889–895. [PubMed] [Google Scholar]
- 122.Denayer S., Helsen C., Thorrez L., Haelens A., Claessens F. The rules of DNA recognition by the androgen receptor. Mol. Endocrinol. 2010;24:898–913. doi: 10.1210/me.2009-0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sahu B., Laakso M., Pihlajamaa P., Ovaska K., Sinielnikov I., Hautaniemi S., Jänne O.A. FoxA1 specifies unique androgen and glucocorticoid receptor binding events in prostate cancer cells. Cancer Res. 2013;73:1570–1580. doi: 10.1158/0008-5472.CAN-12-2350. [DOI] [PubMed] [Google Scholar]
- 124.Davies P., Rushmere N.K. Association of glucocorticoid receptors with prostate nuclear sites for androgen receptors and with androgen response elements. J. Mol. Endocrinol. 1990;5:117–127. doi: 10.1677/jme.0.0050117. [DOI] [PubMed] [Google Scholar]
- 125.Isikbay M., Otto K., Kregel S., Kach J., Cai Y., Vander Griend D.J., Conzen S.D., Szmulewitz R.Z. Glucocorticoid receptor activity contributes to resistance to androgen-targeted therapy in prostate cancer. Horm. Cancer. 2014;5:72–89. doi: 10.1007/s12672-014-0173-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Arora V.K., Schenkein E., Murali R., Subudhi S.K., Wongvipat J., Balbas M.D., Shah N., Cai L., Efstathiou E., Logothetis C., et al. Glucocorticoid receptor confers resistance to antiandrogens by bypassing androgen receptor blockade. Cell. 2013;155:1309–1322. doi: 10.1016/j.cell.2013.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tesch G.H., Young M.J. Mineralocorticoid receptor signaling as a therapeutic target for renal and cardiac fibrosis. Front. Pharmacol. 2017;8:313. doi: 10.3389/fphar.2017.00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dovio A., Sartori M.L., De Francia S., Mussino S., Perotti P., Saba L., Abbadessa G., Racca S., Angeli A. Differential expression of determinants of glucocorticoid sensitivity in androgen-dependent and androgen-independent human prostate cancer cell lines. J. Steroid Biochem. Mol. Biol. 2009;116:29–36. doi: 10.1016/j.jsbmb.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 129.Kim W., Jones J.O., Diamond M., Haqq C., Molina A., Small E.J., Ryan C.J. Inhibition of the androgen receptor by mineralocorticoids at levels physiologically achieved in serum in patients treated with abiraterone acetate. Prostate Cancer Prostatic Dis. 2014;17:292–299. doi: 10.1038/pcan.2014.27. [DOI] [PubMed] [Google Scholar]
- 130.Richards J., Lim A.C., Hay C.W., Taylor A.E., Wingate A., Nowakowska K., Pezaro C., Carreira S., Goodall J., Arlt W., et al. Interactions of abiraterone, eplerenone, and prednisolone with wild-type and mutant androgen receptor: A rationale for increasing abiraterone exposure or combining with MDV3100. Cancer Res. 2012;72:2176–2182. doi: 10.1158/0008-5472.CAN-11-3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shiota M., Fujimoto N., Higashijima K., Imada K., Kashiwagi E., Takeuchi A., Inokuchi J., Tatsugami K., Kajioka S., Uchiumi T., et al. Mineralocorticoid receptor signaling affects therapeutic effect of enzalutamide. Prostate. 2018 doi: 10.1002/pros.23661. [DOI] [PubMed] [Google Scholar]
- 132.Bedussi F., Galli D., Fragni M., Valcamonico F., Rossini E., Dalla Volta A., Vezzoli S., Roca E., Ferrari V., Lazzari B., et al. Amiloride is effective in the management of abiraterone-induced mineralocorticoid excess syndrome without interfering with its antineoplastic activity. Pharmacology. 2017;100:261–268. doi: 10.1159/000477547. [DOI] [PubMed] [Google Scholar]
- 133.Flynn T., Guancial E.A., Kilari M., Kilari D. Case report: Spironolactone withdrawal associated with a dramatic response in a patient with metastatic castrate-resistant prostate cancer. Clin. Genitourin. Cancer. 2017;15:e95–e97. doi: 10.1016/j.clgc.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 134.Shiota M., Fujimoto N., Imada K., Kashiwagi E., Takeuchi A., Inokuchi J., Tatsugami K., Kajioka S., Uchiumi T., Eto M. Prognostic impact of genetic polymorphism in mineralocorticoid receptor and comorbidity with hypertension in androgen-deprivation therapy. Front. Oncol. 2018;8:635. doi: 10.3389/fonc.2018.00635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jacobsen B.M., Horwitz K.B. Progesterone receptors, their isoforms and progesterone regulated transcription. Mol. Cell. Endocrinol. 2012;357:18–29. doi: 10.1016/j.mce.2011.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Grimm S.L., Hartig S.M., Edwards D.P. Progesterone receptor signaling mechanisms. J. Mol. Biol. 2016;428:3831–3849. doi: 10.1016/j.jmb.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 137.Chen R., Yu Y., Dong X. Progesterone receptor in the prostate: A potential suppressor for benign prostatic hyperplasia and prostate cancer. J. Steroid Biochem. Mol. Biol. 2017;166:91–96. doi: 10.1016/j.jsbmb.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 138.Yu Y., Yang O., Fazli L., Rennie P.S., Gleave M.E., Dong X. Progesterone receptor expression during prostate cancer progression suggests a role of this receptor in stromal cell differentiation. Prostate. 2015;75:1043–1050. doi: 10.1002/pros.22988. [DOI] [PubMed] [Google Scholar]
- 139.Yu Y., Lee J.S., Xie N., Li E., Hurtado-Coll A., Fazli L., Cox M., Plymate S., Gleave M., Dong X. Prostate stromal cells express the progesterone receptor to control cancer cell mobility. PLoS ONE. 2014;9:e92714. doi: 10.1371/journal.pone.0092714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bonkhoff H., Fixemer T., Hunsicker I., Remberger K. Progesterone receptor expression in human prostate cancer: Correlation with tumor progression. Prostate. 2001;48:285–291. doi: 10.1002/pros.1108. [DOI] [PubMed] [Google Scholar]
- 141.Grindstad T., Andersen S., Al-Saad S., Donnem T., Kiselev Y., Nordahl Melbø-Jørgensen C., Skjefstad K., Busund L.T., Bremnes R.M., Richardsen E. High progesterone receptor expression in prostate cancer is associated with clinical failure. PLoS ONE. 2015;10:e0116691. doi: 10.1371/journal.pone.0116691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Grindstad T., Richardsen E., Andersen S., Skjefstad K., Rakaee Khanehkenari M., Donnem T., Ness N., Nordby Y., Bremnes R.M., Al-Saad S., et al. Progesterone receptors in prostate cancer: Progesterone receptor B is the isoform associated with disease progression. Sci. Rep. 2018;8:11358. doi: 10.1038/s41598-018-29520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lewis S.R., Hedman C.J., Ziegler T., Ricke W.A., Jorgensen J.S. Steroidogenic factor 1 promotes aggressive growth of castration-resistant prostate cancer cells by stimulating steroid synthesis and cell proliferation. Endocrinology. 2014;155:358–369. doi: 10.1210/en.2013-1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Xiao L., Wang Y., Xu K., Hu H., Xu Z., Wu D., Wang Z., You W., Ng C.F., Yu S., et al. Nuclear receptor LRH-1 functions to promote castration-resistant growth of prostate cancer via its promotion of intratumoral androgen biosynthesis. Cancer Res. 2018;78:2205–2218. doi: 10.1158/0008-5472.CAN-17-2341. [DOI] [PubMed] [Google Scholar]
- 145.Mathieu R., Evrard B., Fromont G., Rioux-Leclercq N., Godet J., Cathelineau X., Guillé F., Primig M., Chalmel F. Expression screening of cancer/testis genes in prostate cancer identifies NR6A1 as a novel marker of disease progression and aggressiveness. Prostate. 2013;73:1103–1114. doi: 10.1002/pros.22659. [DOI] [PubMed] [Google Scholar]