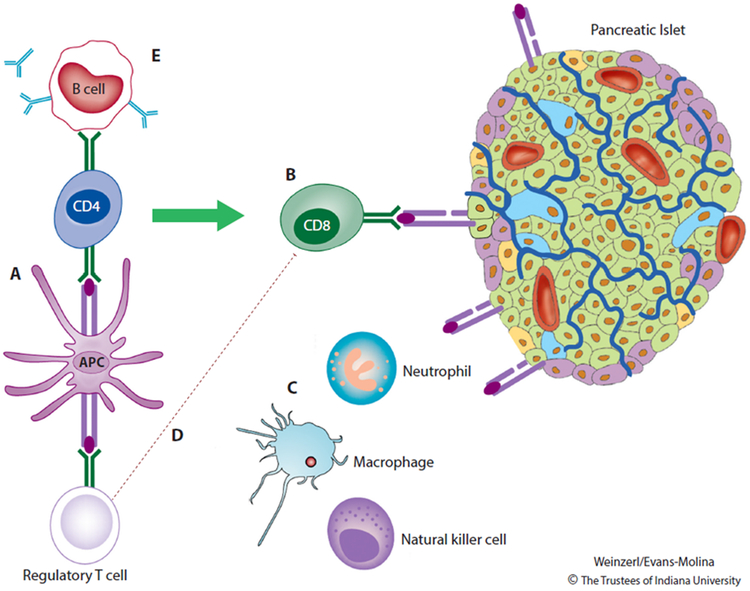
Figure 1. Type 1 Diabetes Pathogenesis.
During the development of Type 1 diabetes, antigen-presenting cells (APCs) residing within the pancreas process and present β-cell peptides on MHC class I molecules. APCs bearing these peptides travel to the pancreatic lymph nodes, where they initiate an immune response that includes activation of autoreactive CD8 T cells and autoantibody production by B lymphocytes. Pancreatic β cells expressing immunogenic peptides on MHC class I surface molecules are targeted for destruction by autoreactive CD8 T cells. Cells of the innate immune system (macrophages, natural killer cells, and neutrophils) exacerbate β-cell death and inflammation through local release of cytokines, chemokines, and reactive oxygen species. β cells participate in this process by releasing chemokines and by up-regulating MHC class I molecules and the associated machinery for antigen presentation. The immune reaction is amplified by impairments in the ability of T regulatory cells to effectively suppress autoimmunity. Autoantibodies against β cells are important markers of immune activation but are not known to play a direct role in disease pathogenesis. Reprinted from The Lancet, Vol. 391, DiMeglio LA, Evans-Molina C, Oram RA, Type 1 diabetes, Pages 2449-2462, Copyright (2018) [4], with permission from Elsevier.