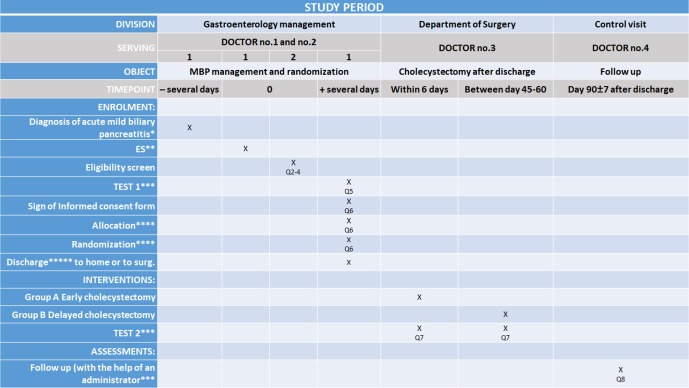
Figure 3.
Schedule of enrolment, interventions and assessments according to the SPIRIT 2013 statement.15 *Diagnosis of acute biliary pancreatitis (any of the following three definitions): diagnosis of gallstones on imaging, and alanine aminotransferase level >2 times higher than normal values with ALT >AST. In the first 24 hours of admission, all patients will undergo either an ultrasonography or a contrast-enhanced CT to detect if the gallbladder contains gallstones and to determinate the diameter of the common bile duct. ABP is mild, when there is no pancreatic necrosis or no transient or persistent organ failure (>48 hours). **If it is necessary to perform endoscopic sphincterotomy during the current admission or ES in the medical history also acceptable. ***Data will be collected in a personalised database and follow-up will consist of questionnaires. The patient will be asked to note every biliary event during the follow-up period and will be contacted in person within the 90 days after discharge to collect information. After data collection, we can draw conclusions about the treatment strategy. Improperly completed datasheets and incorrect data upload will be avoided and controlled by the administrator. (Q5, Q7, Q8, Q=question) **** The patient can be randomised by using a randomisation module with sealed envelope. Patient data will be uploaded to the data base, which will be followed by the randomisation. This randomisation module will allocate the participants to the two different groups. This method makes it impossible for researchers to predict the allocation of the patients involved in the study. It is impossible to conceal the distribution of the patients in this study because the patients need to be scheduled for either an early cholecystectomy or a delayed cholecystectomy. Allocation will be carried out based on predefined randomisation lists created separately for each recruiting centre. The allocation sequence will be prepared with a variable block size and with an allocation ratio 1:1 by the IDMB. *****The criteria are the following: (1) anticipation on the part of the treating physician that the patient can be discharged within 1 or 2 days; (2) no need for analgesics; (3) declining C reactive protein levels and <150 mg/L; (4) no evidence of local or systemic complications (eg, no fever); (5) oral feeding is tolerated for 24 hours and (6) ERCP/ES either during the index admission or in the medical history without complication. Before discharge or transfer to surgery department. ES, endoscopic sphincterotomy; IDMB, Independent Data Management Board.