Abstract
Older adults are more likely to report problem sleep, but little is known about how the economic challenges of old age affect sleep. Using data from the Disability and Use of Time from the Panel Study of Income Dynamics (N=1693), this study applied propensity score methods and the marginal structural model to estimate the associations between exposure to poverty and two measures of problem sleep: risky sleep duration and difficulty falling asleep. Poverty, irrespective of duration of exposure, had little impact on short sleep duration. Exposure to poverty, however, was associated with increased likelihood of long sleep duration and having difficulty falling asleep on both weekdays and weekends, especially for older adults who were exposed to poverty for five or more years. Findings suggest that economic hardship of old age may be a social structural obstacle for healthy sleep.
Not getting a good night’s sleep is increasingly being recognized as a critical behavioral risk factor for chronic diseases and mortality among older adults: poor sleep has been linked to declines in cognitive function (Cricco, Simonsick, and Foley 2001) and increases in diabetes (Gangwisch et al. 2007), heart disease (Phillips and Mannino 2007) and mortality (Cappuccio et al. 2010b). In recent years, a growing number of studies have investigated how social factors shape the elderly’s sleep. Although a few scholars have pointed to the consequences of poverty on children’s sleep (e.g., Sheehen et al., 2018), the role of economic well-being in older adults’ sleep has not been carefully studied. This study builds on this growing literature by considering exposure to poverty as an influential factor on sleep problems in old age. Poverty does not affect merely the material well-being of older adults, it also changes individuals’ life styles and everyday routines, creates stress, and generates conflicts and disorder in the household (Conger et al., 1990; Fox et al., 2002; Halliday, Hardie, & Lucas 2010; Haushofer & Fehr, 2014; Newman & Massengill, 2006). The very experience of living in poverty coupled with the increasing frailty of sleep architecture puts older adults who are poor at high risk for having sleep problems. In this sense, sleep problems are less a behavior of choice and are instead rooted in the social and structural disadvantages that these older adults live with (Hale & Hale, 2009).
Specifically, this study asks two key questions concerning sleep problems in older adults: 1) whether and how poverty affects their sleep and 2) whether enduring poverty has greater consequences than short-term poverty. The empirical analysis takes advantage of rich income data from the Panel Study of Income Dynamics (PSID) and sleep data from the Disability and Use of Time Supplement (DUST). Taken together, the findings help illuminate the role of social structures and processes in causing sleep problems in old age, which is an important insight into an emerging health risk for older adults and sheds light on public health interventions that might promote sleep health in later life.
BACKGROUND
Extant Studies of Economic Well-Being and Problem Sleep
Sleep is one of the most important restorative behaviors for an individual’s health, well-being, and daily activities in mid and later life. Poor sleep has been linked to an increased chance of developing chronic diseases and of excessive mortality (Cappuccio et al. 2010b, Gangwisch et al. 2007, Phillips and Mannino 2007). Of particular importance is the fact that older adults have a higher prevalence of problem sleep. Recent national data shows that approximately one-fourth of older adults reported having insufficient sleep (Liu 2016) and approximately 40 percent older adults reported having trouble falling asleep (Lauderdale et al. 2006). This makes older adults’ sleep health a critical concern, not only for health scholars but also for federal policymakers. The U.S. Department of Health and Human Services’ Healthy People 2020 initiative is, for the very first time, considering improvements to sleep health and the elimination of disparities in sleep as one of the central goals for the agency (U.S. Department of Health and Human Services et al. 2010).
A large volume of the extant studies investigating older adults’ problem sleep do so from a biomedical perspective. That said, researchers do not completely ignore social factors. An increasing number of studies have investigated income or economic hardship and sleep in mid and later life. For example, using data from Coronary Artery Risk Development in Young Adults (CARDIA) study, researchers found that high-income individuals take less time to fall asleep compared to their low-income counterparts (Lauderdale et al. 2006). Friedman and colleagues (2009) used data from a convenient sample of 94 older women and found a negative association between income and time to fall asleep. Using five waves of cross-sectional data, Stamatakis, Kaplan, & Roberts (Stamatakis, Kaplan, and Roberts 2007) found that individuals in the lowest household income quintile consistently had a higher prevalence of short sleep duration, defined as less than six hours of sleep.
Although important, these studies are limited because they are weak in research design and theory. First, the studies rely on crude measures of income and poverty: some use total household income as reported in categories and some use income only at the individual level. Furthermore, many of the studies lack information on household size, which means they cannot accurately calculate poverty status and therefore cannot measure individuals’ exposure to poverty. Second, the studies measure poverty at only one time point, which means they do not investigate the relationship between duration of exposure to poverty and problem sleep. Third, none of the studies carefully consider the non-random distribution of poverty within the population. This is important because characteristics that lead to poverty may also cause problem sleep. If these characteristics are not controlled for in the statistical analysis, estimates of the associations between poverty and sleep are likely to be biased. Finally, these studies lack a conceptual framework that explains why poverty is an influential factor in problem sleep. To foster a better understanding of the role of poverty in individuals’ sleep, research needs to address the aforementioned methodological limitations and synthesize insights from biomedical studies and social science research.
Numerous studies have demonstrated how poverty significantly changes individuals’ behaviors and lifestyles in ways that have huge ramifications for psychological well-being and physical health (i.e., Abramson, 2015; Edin & Lein 1997; Farmer, 2004). Although some recent research suggests that health, particularly early childhood health, can affect socioeconomic attainment (Case, Fertig, & Paxson, 2005; Palloni, 2006), there is still very strong evidence, drawn from studies using data from diverse populations and countries and different health measures, that poverty affects health (Crimmins, Kim, & Seeman, 2009; Marmot, 2002). Likewise, this study recognizes that while poor sleep may increase the chance of living in poverty, a social causation perspective is equally, if not more important, for understanding how poverty affects sleep for older adults who are retired or near the retirement age. Examining poverty means recognizing that an individual’s sleep goes beyond having a comfortable mattress and a clean and quiet home environment that is conducive for a good night’s sleep. Insights from sociology suggest that poverty may be a social structural obstacle that affects older adults’ ability to get a good night’s sleep.
Furthermore, sleep is not a single dimension concept. Poor sleep may mean non-optional sleep duration (i.e., either short sleep duration or long sleep duration), not being able to fall asleep, waking up at nights, or not feeling rested in the morning (Lauderdale et al., 2014). As such, in order to theorize about poverty and sleep, social scientists must use a conceptual model that considers the pathways and mechanisms through which poverty affects different aspects of sleep. With this understanding, the following section develops a conceptual model of poverty and sleep that focuses on two key aspects of problem sleep: risky sleep duration and difficulty falling asleep.
Poverty and Risky Sleep Duration.
Insights from time-use studies suggest that individuals’ bedtime and wakeup time, and thus their sleep duration, is determined by complex social processes through which people allocate and negotiate their sleep time relative to their social status, social roles, and resources (i.e., Burgard, 2011; Burgard & Ailshire, 2013; Venn et al., 2008). In short, an individual’s economic standing affects how one negotiates sleep with oneself and others. First, individuals make decisions about the amount of time they should spend in activities based on each activity’s relative cost (Becker 1965). To determine how much time to allocate to sleep, individuals weigh it in terms of cost (Antillón, Lauderdale, and Mullahy 2014, Biddle and Hamermesh 1989). Here, cost refers to the economic cost and the opportunity cost. In this calculus, a decrease in income reduces the cost of sleep. Individuals who are poor or in mid and later life may have few resources for other activities, and thus choose longer sleep times because it is less costly. In this way, poverty status may increase an individual’s chance of having long sleep duration.
In addition, sleep time is affected by the demands of individuals’ social roles and their social relationships (Meadows 2005). Living in poverty may bring about challenges in social relationships and social roles that make individuals less likely to obtain enough sleep. For example, demographic research has shown that older adults who are poor are more likely to live with other adults and young children who are not their spouses or grandchildren (Kim & Waite, 2016). As such, older adults who are poor may face additional challenges, trying to negotiate sleep time in complex households with non-family members present. It is clearly more difficult to reconcile sleep habits and schedules when multiple other people are present, i.e., older adults who are poor may not be able to sleep at their desired times or in their desired sleeping environment. This, in turn could increase older adults’ chances of having short sleep duration.
Poverty and Difficulty Sleeping.
Living in poverty is usually a very stressful experience. Individuals with few financial resources may be constantly worried about how to afford nutritious food, obtain medications and healthcare services, and pay their monthly rent and utility bills. Other kinds of stress also stem from living in poverty, some of which particularly affect older adults. For example, poverty may affect family processes. Prior research suggests that poverty often leads to a decline in marital quality and greater family conflict and violence (Conger et al. 1990, Fox et al. 2002, Halliday Hardie and Lucas 2010). Thus, individuals who live in poverty are more likely to be exposed to stresses and strains in their family relationships. Older adults who are poor may also be forced to live in disadvantaged neighborhoods with high crime rates. Concerns about safety may mean that older adults have to be vigilant and attentive to the outside environment, which can generate additional stress for them at night (Steptoe & Feldman, 2001).
Not surprisingly, research finds that high levels of stress undermine sleep (Âkerstedt, 2006). Stress challenges the homeostasis and induces physiological responses in the body (Day, 2005). These responses, or stress reactivity, can change circadian rhythms and sleep architecture which lead to sleep abnormalities. The animal model has shown that stress alters sleep physiology. For example, experiments find that stressed rats demonstrate decreases in deep sleep and sleep duration, and more fragmented sleep (Cheeta et al., 1997; Gronli et al., 2004; Pawlyk et al., 2008). In humans, clinical and psychological studies also find that exposure to stress is related to problem sleep (Fuller et al., 1997; Morin, Rodrigue, & Ivers, 2003; Ross et al., 1989). Because poverty is stressful (Abramson, 2015; Edin & Lein, 1997) and evidence clearly points to stress as a catalyst of problem sleep, it is expected that exposure to poverty will lead to a higher chance of problem sleep, such as difficulty falling sleep.
Duration of Exposure and Problem Sleep.
Because the challenges of living in poverty often compound and accumulate over time, older adults who have been poor for longer periods may be continually exposed to stress. This suggests that long-term poverty is more likely to damage individuals’ sleep physiology than short-term exposure to poverty. Indeed, sleep researchers argue that continuously worrying and ruminating about life stress is a critical factor that contributes to patients developing clinically significant insomnia (Harvey, 2002). Thus, individuals who are exposed to long-term poverty have a greater likelihood of showing problem sleep, that is, the longer a poverty spell lasts, the more likely it is to have an effect. For this reason, this paper examines how duration of exposure to poverty relates to risky sleep duration and difficulty falling sleep.
METHODS
The PSID Data
This study used the 2013 wave of data from the PSID’s DUST Supplement. The PSID is a longitudinal study that began in 1968 with a nationally representative sample of approximately 5,000 families. The PSID interviewed members of core families annually from 1968 to 1997 and biennially thereafter. When properly weighted, the design of the PSID produces a nationally representative cross-section of families each year.
In 2013, the PSID conducted a supplementary study that included innovative time-use modules to examine the daily activities of older adults and their allocation of time (Duffy et al. 2013). All the PSID households were eligible for the DUST 2013 if either the household head or the spouse was 60 years of age or older by December 31, 2012. If the household head was married or cohabitating, his or her partner was also eligible. In other words, all older adults aged 60 or older were included in the DUST 2013 sample. If these individuals had spouses at the time of interview, the spouses were also included in the survey, regardless of age. In this study, older adults who were not household heads, such as those who were identified as spouses, were eliminated from the final sample because accurate household income was not available for them. For the same reason, this study eliminated older adults from the sample who were in households where there was no information about whether they were or were not the household head. These exclusions led to a sample size of 1,693. Because the DUST 2013 restricted its sample to individuals who were 60 years old or more (and their spouses) in the main PSID survey, the final sample for this study is a nationally representative sample of families with at least one adult that is 60 years old or older in 2013. When properly weighted, the results of this study can be generalized to families with at least one adult who was 60 years old or older in 2013.
Measures of Sleep Problems
This study measured sleep problems in two ways: 1) risky sleep duration and 2) difficulty falling asleep. First, the duration of nighttime sleep in older adults was calculated. Duration of nighttime sleep was defined as the total length of time for the longest sleep; this measurement follows the approach used in a previous time-use study (Antillón, Lauderdale, and Mullahy 2014). This measure excluded naps and short sleeps. Naps were excluded because clinical and medical recommendations for sleep duration and previous studies of risky sleep duration among older adults all focus only on nighttime sleep (Cappuccio et al., 2010b; Hirshkowitz et al., 2015; Knutson, 2010; Kurnia et al., 2013). And, naps were excluded because the focus of this paper is on risky sleep duration instead of total sleep duration. To check on whether excluding naps has an impact, the author conducted a sensitivity analysis that examined the associations between poverty exposure and sleep duration, with and without naps included. The results were similar regardless of whether naps were included.
After nighttime sleep duration was obtained, an indicator of risky sleep duration was created. Older adults who slept less than six hours were considered to have short sleep duration and older adults who slept more than ten hours were considered to have long sleep duration (Krueger and Friedman 2009, Hirshkowitz et al. 2015). Because it is difficult for time use data to distinguish “time in bed” from “actual sleep duration”, this study followed the approach of previous studies and used a liberal definition of risky sleep duration by focusing sleep durations that were ‘not recommended’ (Hirshkowitz et al. 2015). Because each older adult completed two time diaries, there were two indicators for risky sleep duration: one for weekdays and one for weekends.
In addition, for any respondent who reported sleep as either the first or last activity of the day, the DUST questionnaire also asked a question about difficulty falling asleep. For the question “Did it take you more than half an hour to fall asleep?” respondents answered “yes” or “no.” This question captures a key insomnia symptom, i.e., the ability to initiate sleep, as described in the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013) and International Classification of Diseases (World Health Organization, 2018). Not being able to initiate sleep within a half an hour is also considered an indicator of sleep disturbance in the widely-used Pittsburgh Sleep Quality Index (Buysse et al., 1989). A study of older adults’ sleep patterns also reports that older adults with insomnia took an average of more than 30 minutes to fall asleep, while older adults without insomnia only took 15 minutes (Morin & Gramling, 1989). The DUST’s “difficulty falling asleep” question, though simple, provides important information about a key aspect of older adults’ sleep problems that is of concern in diagnostic criteria and other sleep quality scales.
Measures of Poverty Experience
The main PSID survey includes a full history of each family’s income (Duffy et al. 2013). Using information about total family income, binary indicators were created for each family’s poverty status for each survey year, based on the federal poverty line that uses total pretax family income, and adjusted for family size. The cutoff point for poverty was defined as being below 133 percent of the federal poverty line because families below that threshold are considered to be economically disadvantaged and are eligible for social welfare benefits. Present poverty was defined as being classified in the poverty category for the 2013 survey year. Because the PSID includes data over time, it is possible to trace households’ poverty history. Although it would be ideal to trace poverty trajectories for all older adults back to 1968 when the PSID survey began, in reality only a very small number of the 1,693 older adults in the analytical sample were consistently living in poverty for more than five years. As such, it is difficult to estimate the effects of exposure to poverty for more than five years. Furthermore, because prior demographic research suggests that the majority of poor older adults experience spells of poverty that last less than five years (Sandoval, Rank, and Hirschl 2009), a variable was created that grouped exposure over five years into one category. Thus, the duration of exposure variable included four categories: no exposure, one-year exposure, two to four years exposure, and five or more years exposure.
Covariates
This study included a rich set of covariates that may confound the associations between poverty and sleep. The time-invariant covariates included gender, race, years of education, and the season of the interviews. The time-varying covariates included age, marital status, years of education, employment status, hours of work, homeownership, self-rated health, residential location, and state of residence. In addition, several family-level characteristics were included: age, gender, and race of the household head; type of household (i.e., single, married couple only, others); number of adults in the family unit; number of children under 18 in the family unit; number of older adults employed in the family unit; number of older adults with a high level of psychological distress in the family unit; number of older adults with a functional limitation; and residential area of the family unit (i.e., an eight-category indicator of rural-urban residential location). The 2013 DUST also included a set of six functional limitation questions that were developed for the U.S. Census (Weathers, 2005). Functional limitation, in particular, is important in this study because it may drain economic resources for healthcare and also be associated with older adults’ sleep (Goldman et al., 2007). In other words, functional limitation may confound the association between poverty and sleep and, as such, was controlled for in the statistical analysis. The respondents were asked if they had serious difficulty with the following actions: seeing, even when wearing glasses; concentrating; remembering or making decisions; walking or climbing stairs; dressing or bathing; and doing errands alone. A dichotomous indicator was created for the presence of any functional limitation and added up the number of older adults with functional limitations living in the same family unit. This module was available only in the 2013 DUST, making it equivalent to a time-invariant covariate. Beginning in 2005, the PSID added the K6 psychological distress scale to the main survey. This study used a cut-off point of 19 to distinguish between high-level and low-level psychological distress (Kessler et al. 2003) and added up the number of older adults with a high level of psychological distress in the same family unit.
Statistical Approach
This study started with a multilevel model that links poverty to sleep to account for the nested nature of the data. The first level was individual and the second level was family. However, the simple multilevel model is vulnerable to several problems and could produce biased estimates. First, the estimates from both models are vulnerable to the threat of confounders. Second, when estimating the duration effects, there is an additional problem of over control of the indirect pathways through which long-term exposure to poverty affects sleep, a problem known in the statistics literature as the collider problem (Cole et al. 2010). This study used propensity score methods and a marginal structural model to address these issues.
Propensity Score Methods.
Propensity scores represent the conditional probability of receiving a treatment, given observable characteristics. This study calculated the conditional probability of being in the poverty category, given the observed individual- and family-level characteristics. To reduce the chance of model misspecification, the author used the machine learning, (i.e., classification and regression trees, CART), approach to calculate the propensity score (Lee, Lessler, & Stuart, 2010). Next, the author calculated the inverse probability treatment weight (IPTW), which is the inverse of the estimated conditional probability. Regression-adjustment was combined with propensity score weighting to estimate the effects of present poverty on the sleep of older adults. This approach, known as the “doubly robust estimator,” reduces the chance of biased estimates and model misspecification compared to a situation in which only regression or propensity score weighting is used (Funk et al. 2011).
Marginal Structural Model.
The collider problem refers to the fact that a traditional regression model may over-control time-varying covariates. Figure 1 illustrates this issue. In the diagram, Y is the outcome, X is a time-varying control variable, and T is the treatment. Subscript 1 represents variables at time 1 and subscript 2 represents the subsequent time period. U is an unobserved variable that affects T2 and Y. It is important to note that X2 is a confounder because it predicts not only treatment T2 but also outcome Y, both directly and through U. X2 is also affected by prior treatment T1. The presence of X2 poses a challenge. On the one hand, since X2 is a confounder, it should be controlled in the regression. On the other hand, since earlier treatment T1 affects X2, controlling it may eliminate the effect of earlier treatment on the outcome. Either way, we have biased estimates of longitudinal exposure to poverty.
Figure 1.
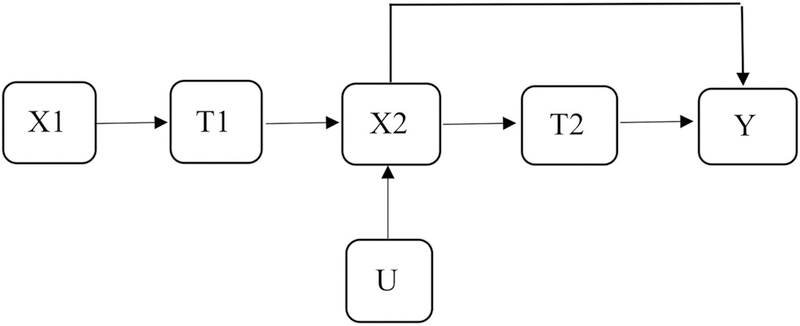
Graph for illustration of two periods of exposure to poverty.
Using the marginal structural model (MSM) allowed the author to generate a pseudo-population in which exposures to poverty were sequentially independent of, but not confounded by, prior observed covariates. This approach simultaneously solved the issue of confounding and over-controlling for the observable time-varying covariates. The MSM approach started by calculating the probability that a family was exposed to poverty at different times, conditional on past treatment and confounders. Then, the inverse probability treatment weight for each time period was calculated. Note, however, that the weights obtained by this procedure may be imprecise estimates. To improve the statistical properties, the author followed the standard practice in MSM literature and used stabilized weights. The stabilized weights are centered around one, have smaller variance, and have approximately normal distribution (Robins, Hernan, & Brumback, 2000). These properties help improve the efficiency of the estimates. In addition, the author bottom-coded the 1st percentile and top-coded the 99th percentile of the stabilized weights, which further improves efficiency in the estimation and minimizes the influence of outliers (Lauen and Gaddis 2013, Wodtke, Harding, and Elwert 2011).
RESULTS
Summary Statistics
Table 1 shows the summary statistics for selected social, demographic, and health characteristics of older adults in 2013, by duration of exposure to poverty. As expected, the longer the exposure to poverty, the more disadvantaged the older adults were. Table 2 provides summary statistics for sleep among older adults in 2013, by duration of exposure to poverty. Panel A shows statistics for the weekday diaries and Panel B shows statistics for the weekend diaries. Table 2 suggests that sleep problems (i.e., short sleep duration, long sleep duration, and difficulty falling asleep) were quite prevalent in old age, particularly for older adults who experienced poverty. In addition, there were no significant differences between the prevalence of sleep problems on weekdays and on weekends, suggesting that problem sleep may not be due to schedule differences between weekends and weekdays.
Table 1:
Summary Statistics of Selected Time-Invariant and Time-Dependent Characteristics in 2013 by Duration of Exposure to Poverty
| No Exposure | One Year Exposure |
2–4 Years Exposure |
5 Years or More Exposure |
|
|---|---|---|---|---|
| (Mean or Proportion) |
(Mean or Proportion) |
(Mean or Proportion) |
(Mean or Proportion) |
|
| Time-Invariant Characteristics | ||||
| Present poverty | 0 | 0.43 | 0.71 | 1 |
| Male | 0.46 | 0.37 | 0.33 | 0.23 |
| Race and ethnicity | ||||
| White | 0.81 | 0.57 | 0.47 | 0.31 |
| African-American | 0.13 | 0.37 | 0.39 | 0.65 |
| Hispanic | 0.05 | 0.02 | 0.06 | 0.04 |
| Other | 0.01 | 0.04 | 0.08 | 0.01 |
| Years of education | 14.06 | 13.22 | 12.13 | 10.92 |
| DUST interview season | ||||
| Fall | 0.38 | 0.35 | 0.46 | 0.41 |
| Winter | 0.14 | 0.14 | 0.08 | 0.10 |
| Spring | 0 | 0 | 0 | 0 |
| Summer | 0.48 | 0.50 | 0.46 | 0.49 |
| Functional limitations | 0.43 | 0.50 | 0.71 | 0.73 |
| Time-Dependent Characteristics | ||||
| Age in 2013 | 66.06 | 66.38 | 66.72 | 68.89 |
| Married in 2013 | 0.77 | 0.48 | 0.40 | 0.20 |
| Hours of work per week | 18.18 | 11.61 | 6.64 | 3.31 |
| Self-rated health | ||||
| Excellent | 0.12 | 0.15 | 0.06 | 0.02 |
| Very good | 0.37 | 0.26 | 0.19 | 0.15 |
| Good | 0.33 | 0.32 | 0.31 | 0.27 |
| Fair | 0.15 | 0.19 | 0.33 | 0.36 |
| Poor | 0.03 | 0.09 | 0.11 | 0.20 |
| K6 scale | 8.14 | 8.82 | 9.37 | 9.84 |
| Number of adults | 1.96 | 1.81 | 1.88 | 1.47 |
| Number of children | 0.16 | 0.27 | 0.28 | 0.43 |
| Sample size | 1311 | 160 | 89 | 133 |
Table 2:
Summary Statistics of Problem Sleep by Duration of Exposure to Poverty (N=1693)
| No Exposure (Proportion) |
One Year Exposure (Proportion) |
2–4 Years Exposure (Proportion) |
5 Years or More Exposure (Proportion) |
|
|---|---|---|---|---|
| A: Weekday Diary | ||||
| Short sleep duration | 0.18 | 0.18 | 0.21 | 0.25 |
| Long sleep duration | 0.08 | 0.13 | 0.15 | 0.17 |
| Difficulty falling asleep | 0.15 | 0.17 | 0.20 | 0.32 |
| B: Weekend Diary | ||||
| Insufficient sleep | 0.14 | 0.19 | 0.16 | 0.20 |
| Long sleep duration | 0.05 | 0.08 | 0.15 | 0.17 |
| Difficulty falling asleep | 0.12 | 0.18 | 0.25 | 0.24 |
| Sample size | 1311 | 160 | 89 | 133 |
Regression Results of Exposure to Poverty on Sleep
Table 3 shows the effects of present poverty on risky sleep duration and difficulty falling asleep using three methods: a basic model that adjusts only for age, gender, and race/ethnicity; a fully regression-adjusted model that adjusts for all aforementioned covariates; and a stabilized IPTW model. Each number in Table 3 represents a result from one regression or analysis. Coefficients for the covariates were omitted for brevity and to facilitate comparison of the estimated effects of different models. Panel A shows results for the weekday diaries and Panel B displays results for the weekend diaries. The results from the basic model show that present poverty strongly predicted long sleep duration and difficulty falling asleep in older adults, both on weekdays and on weekends. The inclusion of the full set of covariates reduced these effects. However, present poverty remained a significant predictor of long sleep duration on weekdays, and difficulty falling asleep on both weekdays and weekend days, even after controlling for a wide range of covariates. For the stabilized IPTW model, the effects were slightly changed, but the patterns remained similar. Difficulty falling asleep remained marginally significant on weekend days; specifically, the estimates showed that present poverty was associated with increased odds of having difficulty falling asleep on weekdays by approximately 71 percent and on weekends by 49 percent. Present poverty was also associated with increased odds of long sleep duration on weekends, specifically by 70 percent. Together, the results from Table 3 suggest that present poverty was associated with an increased chance of having difficulty falling asleep. Yet, at the same time, results for risky sleep duration were mixed. Present poverty was associated with increased odds of long sleep duration but not short sleep duration, and the association was significant for weekend days only.
Table 3:
Associations between Present Poverty on Risky Sleep Duration and Difficulty Falling Asleep (N=1693)
| Risky Sleep Duration Relative risk ratio (S.E.) |
Difficulty Falling Asleep Odds ratio (S.E.) |
||
|---|---|---|---|
| Short Sleep Duration |
Long Sleep Duration |
||
| A: Weekday Diary | |||
| Basic demographics-adjusted model | 1.244 (0.852. 1.815) |
1.795** (1.180. 2.730) |
1.887*** (1308. 2.722) |
| Regression-adjusted model | 1.059 (0.692. 1.620) |
1.413 (0.866. 2.307) |
1.696* (1.104. 2.604) |
| Stabilized IPT weighted | 0.972 (0.639 1.479) |
1.350 (0.835. 2.182) |
1.709* (1.085. 2.693) |
| B: Weekend Diary | |||
| Unadjusted model | 1.327 (0.936. 1.881) |
2.250*** (1.417. 3.574) |
1.839*** (1.295. 2.611) |
| Regression-adjusted model | 1.339 (0.903. 1.986) |
1.974* (1.145. 3.404) |
1.564* (1.044 2.341) |
| Stabilized IPT weighted | 1.380 (0.938 2.030) |
1.696* (0.991. 2.900) |
1.490† (0.956. 2.160) |
Note.
P<.1,
P<.05,
P<.01,
P<.001.
The regression-adjusted model controlled for the full set of covariates. The stabilized IPT weighted results employed the doubly robust estimator by weighting the regression using the stabilized weights and including the full set of covariates. For sleep duration, appropriate sleep duration (6–10 hours) is the reference category.
Table 4 shows the effects that years of exposure to poverty have on risky sleep duration and difficulty falling asleep. Similar to Table 3, for brevity and ease of comparison, results are presented only for the effects of poverty exposure. The reference category is no poverty exposure and results for one-year exposure, two-to-four years exposure to poverty, and five or more years exposure are presented. The results from the basic model show that two-to-four years exposure to poverty and five or more years of exposure to poverty were associated with a higher likelihood of long sleep duration and difficulty falling asleep among older adults. However, when adjusted for the full set of covariates in the regression, most of the associations were reduced. When the MSM is applied to adjust the dynamic nature of the time-varying covariates, the results changed slightly. For five or more years of exposure to poverty, the results for long sleep duration and difficulty falling asleep were both marginally significant. Specifically, Table 4 shows that exposure to five or more years of poverty was associated with an increase of approximately 78 percent in difficulty falling asleep on weekdays and an increase of approximately 63 percent on weekends. In short, the results showed that longer duration of exposure to poverty was associated with an increased probability of long sleep duration on weekend days and difficulty falling asleep. Although theory predicts an increasing effect with increased duration of exposure, such gradients were not found in Table 4, probably because the relatively small sample sizes for older adults in each poverty category made it impossible to detect differences between categories.
Table 4:
Associations between Years of Exposure to Poverty and Risky Sleep Duration and Difficulty Falling Asleep (N=1693)
| Risky Sleep Duration Relative risk ratio (95% CI) |
Difficulty Falling Asleep Odds ratio (95% CI) |
||
|---|---|---|---|
| Short Sleep Duration |
Long Sleep Duration |
||
| Basic demographics-adjusted model | |||
| No exposure (reference) | |||
| 1 year exposure | 1.392 (0.896. 2.164) |
1.502 (0.882. 2.560) |
1.357 (0.841. 2.189) |
| 2–4 years exposure | 1.049 (0.565. 1.949) |
1.624† (0.977. 3.113) |
1.919 * (1.100 3.349) |
| 5 years or more exposure | 1.449 (0.877. 2.394) |
1.950* (1.120. 3.392) |
1.766 * (1.076. 2.900) |
| Regression-adjusted model | |||
| No exposure (reference) | |||
| 1 year exposure | 1.278 (0.794. 2.057) |
1.696 (0.962. 2.988) |
1.185 (0.725 1.939) |
| 2–4 years exposure | 1.019 (0.533. 1.950) |
1.409 (0.689 2.882) |
1.030 (0.548. 1.937) |
| 5 years or more exposure | 1.058 (0.596. 1.878) |
1.220 (0.633. 2.353) |
1.923* (1.124. 3.291) |
| Stabilized IPT weighted | |||
| No exposure (reference) | |||
| 1 year exposure | 1.256 (0.799. 1.975) |
1.240 (0.711. 2.163) |
1.470 (0.764. 2.828) |
| 2–4 years exposure | 1.279 (0.708. 2.312) |
0.925 (0.449. 1.906) |
1.644 (0.851 3.176) |
| 5 years or more exposure | 1.148 (0.653. 2.019) |
0.937 (0.490. 1.793) |
1.782† (0.950. 3.344) |
| Basic demographics-adjusted model | |||
| No exposure (reference) | |||
| 1 year exposure | 0.872 (0.558 1.363) |
1.224 (0.643. 2.328) |
1.119 (0.706 1.773) |
| 2–4 years exposure | 1.181 (0.678 2.056) |
2.484** (1.261 4.894) |
1.292 (0.730 2.285) |
| 5 years or more exposure | 1.331 (0.833 2.126) |
2.686**
(1.483. 4.864) |
2.239*** (1.412 3.548) |
| Regression-adjusted model | |||
| No exposure (reference) | |||
| 1 year exposure | 0.927 (0.581 1.478) |
1.495 (0.762 2.934) |
1.303 (0.769 2.208) |
| 2–4 years exposure | 1.110 (0.603 2.041) |
2.399* (1.139 5.052) |
1.597 (0.861 2.961) |
| 5 years or more exposure | 1.213 (0.712 2.067) |
2.042* (0.999 4.176) |
1.539 (0.870 2.722) |
| Stabilized IPT weighted | |||
| No exposure (reference) | |||
| 1 year exposure | 1.108 (0.723. 1.699) |
1.467 (0.771. 2.790) |
1.319 (0.730. 2.384) |
| 2–4 years exposure | 1.140 (0.632. 2.056) |
1.956† (0.922. 4.152) |
1.070 (0.519. 2.206) |
| 5 years or more exposure | 1.355 (0.803. 2.287) |
1.927† (0.944. 3.933) |
1.686†
(0.990. 3.003) |
Note.
P<.1,
P<.05,
P<.01,
P<.001.
The regression-adjusted model controlled for the full set of covariates. The stabilized IPT weighted results employed the doubly robust estimator by weighting the regression using the stabilized weights and including the full set of covariates. For sleep duration, appropriate sleep duration (6–10 hours) is the reference category.
Finally, in addition to the main analysis, the author performed a sensitivity analysis that examined the effects of poverty on sleep duration, instead of using the binary indicator of insufficient sleep. The results (presented in Appendix A) show that present poverty and longer duration of exposure to poverty were not associated with total sleep duration slightly. The author also performed another sensitivity analysis by defining long sleep duration as 9 hours of sleep or longer. Patters were similar.
DISCUSSION
The prevalence of sleep problems increases with age, which makes it an important topic of study for older adults. Various estimates show that 30–50 percent of older adults report some type of sleep problem. Because older adults’ sleep has traditionally been understood from a biomedical perspective, whether and how social and family processes lead to sleep problems in old age remains a relatively unexplored topic in the aging and health literature. Using unique time-use data from the 2013 DUST and rich information from the core PSID, this study examined the relationship between poverty and sleep in the general population of older adults. The results show that poverty, both present exposure and for five or more years of exposure, was associated with a higher likelihood of long sleep duration and difficulty falling asleep. For difficulty falling asleep, the patterns and effect sizes were consistent for weekdays and weekend days, suggesting that the challenges of living in poverty affect the ability to fall asleep all week long. Results for risky sleep duration were somewhat mixed. Poverty was not associated with short sleep duration but was associated with long sleep duration, but only on weekend days.
The mostly non-effect of sleep duration may indicate that older adults successfully strive to maintain normal sleep routines in the face of poverty, i.e., older adults have coping strategies that are somewhat effective. Indeed, the exercise of human agency in adapting to adverse events has been widely observed in sociological studies (Mendenhall et al. 2008). However, the negative effect that poverty has on the difficulty they experience falling asleep indicates that older adults are not as autonomous with respect to sleep as sleep researchers have assumed (Patlak 2005). If older adults were fully able to adopt the sleep-promoting behaviors they wish, we would not expect to observe that poverty has a negative effect on sleep. The relationship between poverty and difficulty falling asleep, however, implies that the abilities of older adults to exercise human agency are socially and culturally constrained (Thoits 2006). Not all coping strategies will be successful (Thoits 2006). Older adults who live in poverty may find it relatively easy to maintain their bedtimes and wake-up times, but other behaviors that facilitate getting to sleep are more difficult for them to maintain. For example, although physicians recommend that individuals slow down and relax prior to going to bed (Patlak 2005), this may not be easy to do when older adults are consistently exposed to the stresses of poverty. Furthermore, these issues may be exacerbated by the declines in social networks and support that occur when people age (Cornwell, Laumann, and Schumm 2008). Older adults have fewer social resources to draw on to enhance their ability to cope successfully with stress and to facilitate getting to sleep. Findings from this study reveal the complex processes through which poverty and the aging process constrain sleep-enhancing behaviors in different ways.
By exploring how poverty affects the different aspects of sleep in older adults, this study provides new insight into an understudied behavioral risk factor that is connected to chronic diseases and mortality. Biological evidence has linked shorter sleep duration to higher risks for diabetes and heart disease (Gangwisch et al. 2007, Phillips and Mannino 2007). Epidemiological research has observed associations between shorter sleep durations and higher rates of diabetes, coronary heart disease, and mortality (Cappuccio et al. 2010a, King et al. 2008). In this respect, it is possible that poverty affects the physical health of older adults through its influence on sleep outcomes. The results from this study provide the very first evidence for this hypothesis. This study found evidence that both present poverty and five or more years of exposure to poverty increased the probability of experiencing difficulty falling asleep, which implies that the relationships between poverty and physical health in old age may operate through the decline of good sleep. Nevertheless, since this mechanism was not tested directly, future studies with longitudinal data on economic well-being, sleep, and morbidity/mortality are needed to provide additional empirical evidence.
Although the study used innovative data and advanced statistical techniques for causal inference, it still has several limitations that should be noted. First, the non-random mortality selection of impoverished older adults may bias the estimates downward. Impoverished individuals, especially those exposed to poverty for a longer period of time, were more likely to get lost in the sample due to deaths or attrition. As such, for the most impoverished individuals, it might not be possible to observe the association between poverty exposure and sleep. This may lead to conservative estimates of the association between poverty and sleep. The application of propensity score methods and an MSM helps, but it is still difficult to establish a causal relationship between poverty and sleep measures. As such, the results of this study remain associational. Second, although the PSID interviews have been conducted biennially since 1997, income information for the year between the two interview years was not available. As a result, the analysis did not capture potential changes in poverty status between two waves, which means the number of older adults who were exposed to poverty may have been overestimated. Third, recent studies suggest that more complex duration variables may better capture the age-related changes in sleep duration (Klerman & Dijk, 2008; Skeldon, Derks, & Dijk, 2016). This study was not able to demonstrate how poverty in old age affects sleep physiology, circadian rhythm, and/or the need for sleep. Recall that in this study, poverty exposure had a non-significant effect on likelihood of having risky sleep duration, but this does not rule out the possibility that using these more complex duration variables would demonstrate that effect. That said, this study did use self-reported sleep duration from time-use data and thresholds that are recommended by the National Sleep Foundation (Hirshkowitz et al., 2015), and in doing so, revealed important insights about poverty and habitual sleep duration among the elderly. In this way, this study is a foundation for future research on the relationships between poverty exposure and age-related changes in sleep for older adults. Also, note that measurement error may affect the estimations. Older adults’ sleep durations may be overestimated because, in time-use data, it is difficult to distinguish time in bed from actual sleep time and it is difficult to obtain accurate wake times after sleep onset. The effects of poverty on sleep may be stronger if future studies adopt objective measures of sleep that capture older adults’ actual sleep durations more accurately. Finally, the study is limited because, although the 2013 DUST provided data on sleep initiation and duration, it did not capture all the important aspects of sleep, such as sleep architecture, that may be affected by poverty.
Limitations notwithstanding, this is one of the very first systematic studies that examines the relationship between poverty and sleep in old age. The findings reveal that sleep, like other health behaviors, is regulated by the household socioeconomic context. Furthermore, since older adults’ sleep health is increasingly recognized as a critical public health issue, the findings from this study offer a different solution for improving sleep health in older adults (Thoits 2010). In addition to medication and psychotherapy, programs and initiatives that help to alleviate poverty in old age may also benefit older adults’ sleep outcomes. In short, social justice is good for older adults’ sleep (Hale & Hale, 2009), which is a finding that has the potential to inform policy for the estimated over 4.2 million older adults in the U.S. who are poor (DeNavas-Walt and Proctor 2014).
Appendix
Appendix A:
Results from Doubly Robust Estimator with Stabilized IPT weights that Show Associations between Poverty Exposure and Total Sleep Duration (N=1693)
| Total Sleep Duration Excluding Naps Coefficient (S.E.) |
Total Sleep Duration Including Naps Coefficient (S.E.) |
|
|---|---|---|
| A: Weekday Diary | ||
| Analysis 1: Present Poverty | 16.63 (10.31) |
0.74 (18.49) |
| Analysis 2: Years of Exposure (reference: no exposure) | ||
| 1 year exposure | −1.80 (11.55) |
−2.71 (20.69) |
| 2–4 years exposure | 14.71 (15.28) |
36.00 (27.72) |
| 5 years or more exposure | 17.27 (14.69) |
10.19 (26.01) |
| B: Weekend Diary | ||
| Analysis 1: Present Poverty | −3.19 (11.18) |
−25.80 (16.92) |
| Analysis 2: Years of Exposure (reference: no exposure) | ||
| 1 year exposure | 10.52 (12.49) |
−11.68 (19.26) |
| 2–4 years exposure | 12.12 (16.87) |
−6.27 (25.79) |
| 5 years or more exposure | 16.08 (15.80) |
−15.29 (24.21) |
Note.
P<.1,
P<.05,
P<.01,
P<.001.
The regression-adjusted model controlled for the full set of covariates. The stabilized IPT weighted results employed the doubly robust estimator by weighting the regression using the stabilized weights and including the full set of covariates.
References
- Abramson CM (2015) The End Game: How Inequality Shapes Our Final Years. Cambridge, MA: Harvard University Press. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5). American Psychiatric Pub. [Google Scholar]
- Antillón Marina, Lauderdale Diane S, and Mullahy John. 2014. “Sleep behavior and unemployment conditions.” Economics & Human Biology 14:22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker Gary S. 1965. “A Theory of the Allocation of Time.” The economic journal:493–517. [Google Scholar]
- Biddle Jeff E, and Hamermesh Daniel S. 1989. Sleep and the Allocation of Time. National Bureau of Economic Research. [Google Scholar]
- Buysse DJ, Reynolds CF III, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- Cappuccio Francesco P, D’Elia Lanfranco, Strazzullo Pasquale, and Miller Michelle A. 2010a. “Quantity and quality of sleep and incidence of type 2 diabetes a systematic review and meta-analysis.” Diabetes care 33 (2):414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio Francesco P, D’Elia Lanfranco, Strazzullo Pasquale, and Miller Michelle A. 2010b. “Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies.” Sleep 33 (5):585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Fertig A, & Paxson C (2005). The lasting impact of childhood health and circumstance. Journal of health economics, 24(2), 365–389. [DOI] [PubMed] [Google Scholar]
- Cole Stephen R, Platt Robert W, Schisterman Enrique F, Chu Haitao, Westreich Daniel, Richardson David, and Poole Charles. 2010. “Illustrating bias due to conditioning on a collider.” International journal of epidemiology 39 (2):417–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger Rand D, Elder Glen H Jr, Lorenz Frederick O, Conger Katherine J, Simons Ronald L, Whitbeck Les B, Huck Shirley, and Melby Janet N. 1990. “Linking economic hardship to marital quality and instability.” Journal of Marriage and the Family:643–656. [Google Scholar]
- Benjamin Cornwell, Laumann Edward O, and Schumm L Philip. 2008. “The social connectedness of older adults: A national profile.” American sociological review 73 (2):185–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cricco Meredith, Simonsick Eleanor M, and Foley Daniel J. 2001. “The impact of insomnia on cognitive functioning in older adults.” Journal of the American Geriatrics Society 49 (9):1185–1189. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, & Seeman TE (2009). Poverty and biological risk: the earlier “aging” of the poor. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 64(2), 286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeNavas-Walt Carmen, and Proctor Bernadette D. 2014. “Income and Poverty in the United States: 2013 Current Population Reports.” Washington, DC: US Department of Commerce, US Census Bureau. [Google Scholar]
- Duffy Denise, Leissou Eva, McGonagle Katherine, and Schlegel Jay. 2013. “PSID Main Interview User Manual: Release 2013.” [Google Scholar]
- Fox Greer Litton, Benson Michael L, DeMaris Alfred A, and Wyk Judy. 2002. “Economic distress and intimate violence: Testing family stress and resources theories.” Journal of Marriage and Family 64 (3):793–807. [Google Scholar]
- Funk, Michele Jonsson, Westreich Daniel, Wiesen Chris, Stürmer Til, Brookhart M Alan, and Davidian Marie. 2011. “Doubly robust estimation of causal effects.” American journal of epidemiology 173 (7):761–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, Rundle AG, Zammit GK, and Malaspina D. 2007. “Sleep du-ration as a risk factor for diabetes incidence in a large US sample.” Sleep 30 (12):1667–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Boudreau R, … & Newman AB (2007). Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep, 30(10), 1317–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale B, & Hale L (2009). Is justice good for your sleep?(And therefore, good for your health?). Social Theory & Health, 7(4), 354–370. [Google Scholar]
- Halliday Hardie Jessica, and Lucas Amy. 2010. “Economic factors and relationship quality among young couples: Comparing cohabitation and marriage.” Journal of Marriage and Family 72 (5):1141–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, and Adams Hillard PJ. 2015. “National Sleep Foundation’s sleep time duration recommendations: methodology and results summary.” Sleep Health 1 (1):40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C, Barker Peggy R, Colpe Lisa J, Epstein Joan F, Gfroerer Joseph C, Hiripi Eva, Howes Mary J, Normand Sharon-Lise T, Manderscheid Ronald W, and Walters Ellen E. 2003. “Screening for serious mental illness in the general population.” Archives of general psychiatry 60 (2):184–189. [DOI] [PubMed] [Google Scholar]
- King Christopher Ryan, Knutson Kristen L, Rathouz Paul J, Sidney Steve, Liu Kiang, and Lauderdale Diane S. 2008. “Short sleep duration and incident coronary artery calcification.” Jama 300 (24):2859–2866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klerman EB, & Dijk DJ (2008). Age-related reduction in the maximal capacity for sleep—implications for insomnia. Current Biology, 18(15), 1118–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL (2010). Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best practice & research Clinical endocrinology & metabolism, 24(5), 731–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger Patrick M, and Friedman Elliot M. 2009. “Sleep duration in the United States: a cross-sectional population-based study.” American journal of epidemiology 169 (9):1052–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurina LM, McClintock MK, Chen JH, Waite LJ, Thisted RA, & Lauderdale DS (2013). Sleep duration and all-cause mortality: a critical review of measurement and associations. Annals of epidemiology, 23(6), 361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale Diane S, Knutson Kristen L, Yan Lijing L, Rathouz Paul J, Hulley Stephen B, Sidney Steve, and Liu Kiang. 2006. “Objectively measured sleep characteristics among early-middle-aged adults the CARDIA study.” American journal of epidemiology 164 (1):5–16. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS, Philip Schumm L, Kurina LM, McClintock M, Thisted RA, Chen JH, & Waite L (2014). Assessment of sleep in the national social life, health, and aging project. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(Suppl_2), S125–S133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauen Douglas Lee, and Gaddis S Michael. 2013. “Exposure to Classroom Poverty and Test Score Achievement: Contextual Effects or Selection? 1.” American Journal of Sociology 118 (4):943–979. [Google Scholar]
- Liu Yong. 2016. “Prevalence of healthy sleep duration among adults—United States, 2014.” MMWR. Morbidity and mortality weekly report 65. [DOI] [PubMed] [Google Scholar]
- Marmot M (2002). The influence of income on health: views of an epidemiologist. Health affairs, 21(2), 31–46. [DOI] [PubMed] [Google Scholar]
- Meadows Robert. 2005. “The ‘negotiated night’: an embodied conceptual framework for the sociological study of sleep.” The Sociological Review 53 (2):240–254. [Google Scholar]
- Mendenhall Ruby, Kalil Ariel, Spindel Laurel J, and Hart Cassandra MD. 2008. “Job loss at mid-life: Managers and executives face the “New Risk Economy”.” Social Forces 87 (1):185–209. [Google Scholar]
- Morin CM, & Gramling SE (1989). Sleep patterns and aging: comparison of older adults with and without insomnia complaints. Psychology and aging, 4(3), 290. [DOI] [PubMed] [Google Scholar]
- Palloni A (2006). Reproducing inequalities: Luck, wallets, and the enduring effects of childhood health. Demography, 43(4), 587–615. [DOI] [PubMed] [Google Scholar]
- Patlak Margie. 2005. Your guide to healthy sleep: US Department of Health and Human Services. [Google Scholar]
- Phillips Barbara, and Mannino David M. 2007. “Do insomnia complaints cause hypertension or cardiovascular disease.” J Clin Sleep Med 3 (5):489–494. [PMC free article] [PubMed] [Google Scholar]
- Robins JM, Hernan MA, & Brumback B (2000). Marginal Structural Models and Causal Inference in Epidemiology. Epidemiology, 11(5), 550–560 [DOI] [PubMed] [Google Scholar]
- Sandoval Daniel A, Rank Mark R, and Hirschl Thomas A. 2009. “The increasing risk of poverty across the American life course.” Demography 46 (4):717–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan C, Powers D, Margerison-Zilko C, McDevitt T, & Cubbin C (2018). Historical neighborhood poverty trajectories and child sleep. Sleep health, 4(2), 127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeldon AC, Derks G, & Dijk DJ (2016). Modelling changes in sleep timing and duration across the lifespan: changes in circadian rhythmicity or sleep homeostasis?. Sleep medicine reviews, 28, 96–107. [DOI] [PubMed] [Google Scholar]
- Stamatakis Katherine A, Kaplan George A, and Roberts Robert E. 2007. “Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up.” Annals of epidemiology 17 (12):948–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits Peggy A. 2006. “Personal agency in the stress process.” Journal of Health and Social Behavior 47 (4):309–323. [DOI] [PubMed] [Google Scholar]
- Thoits Peggy A. 2010. “Stress and health major findings and policy implications.” Journal of health and social behavior 51 (1 suppl):S41–S53. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services, Office of Disease Prevention, Health Promotion, US Department of Health, Human Services, Office of Disease Prevention, and Health Promotion. 2010. Healthy people 2020. [Google Scholar]
- Wodtke Geoffrey T, Harding David J, and Elwert Felix. 2011. “Neighborhood effects in temporal perspective the impact of long-term exposure to concentrated disadvantage on high school graduation.” American Sociological Review 76 (5):713–736. [DOI] [PMC free article] [PubMed] [Google Scholar]


