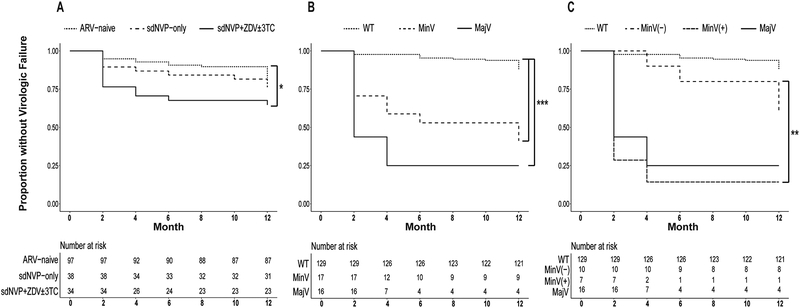
Figure 2. Kaplan-Meier survival analysis.
Survival probabilities (i.e., proportion without virologic failure) during 12 months of non-nucleoside reverse transcriptase inhibitor-based ART (NNRTI-ART) of all women stratified by history of antiretroviral (ARV) treatment for prevention-of-mother-to-child-transmission (PMTCT) (Panel A), and by pre-ART drug-resistance category (wild-type (WT), minority variants (MinV), majority variants (MajV)) (Panel B). Women with minority variants were further stratified into those with (MinV(+)) and without (MinV(−)) exposure to sdNVP+ZDV±3TC. Benjamini-Hochberg-adjusted P values denote levels of significance for pairwise log-rank comparisons between survival curves: ‘*’ 0.05, ‘**’ 0.01, ‘***’ <0.0001. Risk tables denote total number of participants with outcome at each timepoint below survival plots.
Panel A: Increased virologic failure was observed in women with a history of sdNVP+ZDV±3TC for PMTCT compared to ARV-naïve women (P=0.05).
Panel B: next-generation-sequencing analyses found that minority variants (MinV) (1–9% of one or more mutant variants within an individual’s HIV quasispecies) and majority variants (MajV) (10–100% mutant) were associated with increased virologic failure compared to wild-type (WT) (<1% mutant) (both P<0.0001).
Panel C: Next-generation-sequencing analyses found that among women with minority variants, increased virologic failure was associated with sdNVP+ZDV±3TC-experience (MinV(+)) compared to ARV-naïve and sdNVP-only-experienced women (MinV(−)), (P=0.01).