Abstract
Functional dyspepsia (FD) is a common upper gastrointestinal disorder globally, but the current treatments for FD are still unsatisfactory. This study was aimed at investigating the effects of comfort care on symptoms, gastric motility, and mental state of patients with FD.
One hundred consecutive patients with FD treated at the Wuhan Union Hospital (Wuhan, China) between 03/2016 and 02/2018 were randomized to routine nursing and comfort care on the basis of routine nursing (50 patients/group), all for 8 weeks. The primary endpoint was FD symptom score. The secondary endpoint included gastric emptying rate, gastric motility parameters, and depression and anxiety scores. The endpoints were assessed at baseline and after 8 weeks.
There were no significant differences between the 2 groups for gender, age, body mass index, types of FD, and course of disease (P > .05). The symptom score in the comfort care group at week 8 was lower than in the routine nursing group (8.3 ± 2.4 vs 10.2 ± 2.4, P < .001). The gastric emptying rate in the comfort care group at week 8 was higher than in the routine nursing group (28.6 ± 5.1 vs 24.3 ± 5.5, P < .001). The fasting and postprandial dominant frequencies of electrogastrogram in the comfort care group at week 8 were higher than in the routine nursing group (1.9 ± 0.9 vs 1.8 ± 1.0, P = .004; 3.1 ± 1.0 vs 2.1 ± 0.9, P < .001). The postprandial dominant power of electrogastrogram in the comfort care group at week 8 was higher than in the routine nursing group (55.7 ± 11.5 vs 42.3 ± 12.5, P < .001). The cases of abnormal electrogastrogram rhythm in the comfort care group at week 8 were significantly less than in the routine nursing group (P = .003). The self-rating depression scale and self-rating anxiety scale in the comfort care group at week 8 were significantly lower than in the routine nursing group (42.5 ± 6.9 vs 47.3 ± 6.4, P = .001; 41.1 ± 7.2 vs 46.3 ± 6.9, P < .001).
Comfort care reduces the symptoms of patients with FD, increases gastric emptying rate, improves gastric motility, relieves patient's depression and anxiety, and promotes the rehabilitation of the disease.
Keywords: comfort care, functional dyspepsia, gastric motility, mental state
1. Introduction
Functional dyspepsia (FD) is a functional gastrointestinal disorder and is very common in clinical practice, with a global prevalence of 5% to 11%[1] and seriously affecting the patients’ quality of life. According to Rome III criteria,[2] FD refers to the existence of 1 or more symptoms of dyspepsia that originate in the gastroduodenal region and lack a group of clinical syndromes of any organic, systemic, or metabolic disease that can explain these symptoms.
The pathogenesis of FD is still unclear, but it is considered to be closely related to several pathophysiological mechanisms such as gastroduodenal dysfunction and visceral hypersensitivity, but also firmly associated with socio-psychological factors (eg, anxiety, depression, introversion, stressful interpersonal relationship, stress, etc),[3] leading to nonstandard and inefficient treatment strategies for FD. About half of the patients diagnosed with FD still have dyspepsia symptoms after a 5-year follow-up, affecting their quality of life over the long-term.[4,5]
Previous studies have pointed out that high-quality nursing service could effectively control the disease and adjust the therapeutic effects. The comfort theory, a nursing theory developed in the 1990s by Katharine Kolcaba, emphasizes on patients as the center and the nurses critical thinking to find the best comfort care program, give patients proper care, enable patients to achieve the most pleasant state in physiological, mental, psychological, social, and environmental aspects, or shorten and reduce patient's unpleasant degree.[6,7]
Nevertheless, the application of the comfort theory for the management of FD is still poorly understood. Therefore, the purpose of this study was to apply comfort care to the FD clinical nursing process, to observe the effects on the symptoms, gastric motility, and patients’ mental state in order to improve the patients’ quality of life.
2. Methods
2.1. Subjects
A prospective randomized controlled single-blind study was conducted. A total of 100 consecutive patients with FD treated at the Department of Gastroenterology of Wuhan Union Hospital (Wuhan, China) between March 2016 and February 2018 were prospectively enrolled at the outpatient clinic. This study was approved by the ethics committee of Wuhan Union Hospital, and all the patients signed informed content.
The inclusion criteria were:
-
(1)
18 to 75 years of age, no gender limitation;
-
(2)
according to the Rome III Questionnaire for diagnosis of FD, patient who met the diagnostic criteria of Rome III (in May 2016, the Rome Committee promulgated functional gastrointestinal disorders, but the present study began earlier than the promulgation of the diagnostic criteria of Rome IV; compared with Rome III, Rome IV had generally little adjustment to FD[8]; in combination with the China consensus on FD (2015, Shanghai)[9] and the results of the present researches in China, and in order to ensure the consistency of the study, the diagnostic criteria of Rome III was adopted in this study);
-
(3)
least 1 item of the dyspepsia severity score with >2 points; and
-
(4)
voluntarily participated in the study and signed the informed consent form.
The exclusion criteria were:
-
(1)
pregnant or lactating women;
-
(2)
history of gastrointestinal surgery;
-
(3)
gastrointestinal organic diseases;
-
(4)
any other gastrointestinal functional diseases;
-
(5)
any other internal diseases (eg, liver and kidney diseases, chronic severe infections, diabetes, or autoimmune diseases); or
-
(6)
mental disease.
2.2. Randomization
All patients were randomly divided into comfort care group and routine nursing group according to a random number table (50 patients in each group). The table was prepared by an independent biostatistician.
2.3. Blinding
Due to the nature of the intervention, the patients and nurses could not be blind to grouping. On the other hand, the professionals who applied the scoring scales and performed the various tests were all blind to grouping.
2.4. Methods
2.4.1. Comfort care theory and behavioral skills training
Comfort care was implemented by trained primary nurses in a ward. Training methods included theoretical and behavioral skills. The specific contents of the theoretical training involved Kolcaba's Comfort Theory, Betty Neuman's system model, and other related knowledge. The specific contents of behavioral skills training included the evaluation of stressor, the intervention for stressor, nursing care for alleviating stress response, active psychological intervention, and nursing professional social support. Duration of nurse training was from December 2015 to February 2016, 2 hours per week, 12 weeks, and a total of 24 hours. Trainers were trained by lectures, study, and discussion, as well as demonstration exercises.
2.4.2. Nursing method
Nurses performed routine drug treatment according to doctor's advice for the patients of 2 groups; according to the patients’ symptoms, proton pump inhibitors or H2 receptor antagonists, gastrointestinal motility agents, digestive enzyme preparations, or traditional Chinese medicines were given according to their type of syndrome and willingness: Sanjiu Weitai granule (6 and 8 patients), Zhizhu Kuanzhong capsule (3 and 5 patients), Qizhi Weitong granule (4 and 5 patients), Jianwei Xiaoshi oral liquid (2 and 3 patients), and Shenling Baizhu granule (2 and 1 patients). The course of treatment was 8 weeks. The patients of the 2 groups were given FD routine nursing, including providing related health education, helping patients establish good eating habits,[10] and observing the changes of the disease, the adverse reactions and curative effect of the drugs. Accordingly, primary nurses daily carried out comfort care intervention to the patients in the comfort care group. Hospitalization, examinations, and nursing were provided free of charge. The patients received the intervention once a day during hospitalization for a total of 7 days. Then, they were discharged with doctor's advices and the follow-up intervention was conducted every 3 days for a total study duration of 8 weeks. All interventions were routinely implemented.
2.4.2.1. Physical comfort care
2.4.2.1.1. Assessing the patients’ stressors
After admission, the nurses comprehensively assessed patient's physical and mental state, and determined their actual stressors such as economic problems, marital conflicts, work problems, interpersonal tension, family member's death, and traumatic diseases. During the period of hospitalization, according to the patient's condition, the nurses determined the potential stressors in time such as the aggravation of symptoms, the diagnosis of disease, the change of role, and the influence of iatrogenic diseases.
2.4.2.1.2. Intervention for stressor
The nurses helped patients weaken or eliminate actual stressors, explained the effects of various stress factors on disease, guided patients to strengthen their own mental and physical exercise, enhanced patient's adaptability to various negative life events in order to reduce patient's negative emotions and to make patient's good mood state and synchronously develop the effect of intervention. For potential stressors, highlight was put on the prevention of diseases. The nurses helped patients adapt to the change in the hospital environment and role. The communication between nurses and patients was strengthened, a good relationship between nurses and patients was established, and the origin of iatrogenic stress caused by the behavior of nurses and the poor communication between nurses and patients was prevented.
2.4.2.1.3. Nursing care activities for relieving stress reaction
Patients often had physiological responses to stress such as weight loss, insomnia, pain, fatigue, lack of appetite, and so on. Thus, the nurses carried out symptoms management and strengthened nursing from medicine, diet, nutrition, sleep, and pain management. For psychological responses to stresses such as anxiety and depression, nurses performed cognitive intervention on patients from the aspects of disease impact, determination of the nature of disease, treatment control, personal control, course of disease, emotional reaction, disease understanding, pathogeny, and so on.[11] Some patients required antidepressant drugs. Some of them had misunderstandings about the drugs, such as fear of drug dependence and adverse reactions, or lack of understanding of the disease, which led to the misunderstanding that they have been cured and there was a poor medication compliance.[12] The nurses should strengthen the guidance of patient's medication, explain the nature, function and possible adverse reactions of the drugs as well as the preventive measures to the patients and their families, so that patients could actively cooperate with medication and improve the compliance of intervention.
2.4.2.2. Nursing care for mental and psychological comfort
2.4.2.2.1. Attributable intervention
Nurses helped patients make positive attributions, guided patients to attribute the disease to external, temporary, and controllable factors, and encouraged patients to look at problems with an optimistic attitude. For instance, although the cost of treatment created a great burden on family economy; however, “Where there is life, there is hope” and so on to keep patients in harmony and balance in mind.
2.4.2.2.2. Gratitude intervention
Nurses instructed patients to record 2 cases that they felt they needed to thank each day, and to daily record their overall feelings and expectations; to help patients recall if he/she had been grateful to someone, but never has clearly expressed it to him/her, and to help patients write a letter of thanks and read it to him/her face-to-face; nurses instructed patients to spend 20 to 30 minutes every day to meditate or record a positive life experience in the past. There were a variety of positive psychological interventions. Nurses could implement different interventions for the actual situation of patients and help them fight negative emotions by establishing their own positive resources.
2.4.2.3. Nursing care for social comfort
-
(1)
Establishment of a therapeutic communication system. The nurses established a proper relationship with patients through communication, then they carried out evaluative communication. In order to ensure the correct assessment and analysis of the physical, psychological, and social problems of the patients, the nurses accurately grasped the differences among patients’ conditions, psychological characteristics and the degree of demand for information, burden of disease, social support, and other aspects. In addition, dynamic and personalized intervention communication was undertaken to help patients solve the most troubling problems.
-
(2)
The nurses provided information and technical support required to patients’ family members to assist the patients in enhancing their utilization of social support, explain physical, psychological, and social knowledge related to patient's disease to their family members, and make them realize that their negative emotion and stress response were due to the disease. Thus, the patients’ family members could fully understand patients and actively express care and strengthen care to the patients. The nurses informed patients’ family members with effective communication skills, which assisted family members in strengthening positive communication with the patients and helped harmonize the relationship between patients’ family members and patients, so as to reduce the occurrence of negative life events such as family conflicts. For example, when a patient talked about his/her inner thoughts, his/her family members should not stop the patient's emotional expression with a simple comfort such as “It does not matter, do not think about it,” they should listen and comfort more to the patient, help the patient with emotional catharsis through deep heart communication, so as to avoid negative emotional deterioration.
After the patients of the 2 groups were discharged from the hospital, they were followed up by nurses. Every 3 days, primary nurses were responsible to carry out nursing interventions by phone, or a short text or video message. The duration of the nursing intervention for the 2 groups was 8 weeks. At the end of 8th week, patients came to the hospital for re-examination.
2.4.3. Endpoints, assessment indexes, and methods
The primary endpoint was FD symptom score, the secondary endpoint included gastric emptying rate, gastric motility parameters, depression and anxiety scores. The above parameters were assessed and compared at baseline and the end of 8th week separately between the 2 groups.
-
(1)
Score of FD symptoms. The dyspepsia symptom score (DSS) was used to assess the severity of dyspepsia in patients.[2] The degree and frequency of 8 symptoms (postprandial satiety discomfort, early satiety, upper abdominal pain, upper abdominal distension, burning sensation in the upper abdomen, nausea, vomiting, and belching) were assessed. The degrees of symptoms were divided into: 0 = without symptom; 1 = mild: attention was required to be aware of symptoms, and symptoms did not affect patient's work and life; 2 = moderate: degree of symptoms were between mild and severe, and part of symptoms affected patient's work and life; 3 = severe: symptoms were obvious, symptoms were unbearable and significantly affected patient's work and life. Each option was scored as 0, 1, 2, and 3 points, respectively. Frequency was divided into: 0) none; 1) <1 day/month; 2) 1 d/mo; 3) 2 to 3 d/mo; 4) 1 to 2 d/wk; 5) 3 to 4 d/wk; or 6) 5 to 7 d/wk. Options 4, 5, and 6 were scored 1, 2, and 3 points, respectively; the others were scored 0. After fully clarifying the patients’ symptoms, each symptom was scored and the DSS was the sum of the degrees and frequencies of the symptoms. Total scores of FD symptom before intervention and 8 weeks after intervention were recorded.
-
(2)
Gastric emptying examination. The gastric emptying rate of solid food was detected by using a radiopaque X-ray marker. In this study, after 12 hours of fasting, on the next morning, patients were given a standard meal (instant noodle 80 g, ham 50 g, and water 400 ml, and consumed within 15 minutes). Twenty small barium strips (length of 10 mm, diameter of 1.0 mm, and weight of 25 mg) were uniformly swallowed during the meal. Then, water and food were prohibited after the meal and strenuous exercise was avoided. After 5 hours, an abdominal orthostatic plain film was taken, and the number of residual barium strips in the stomach was counted. The 5-hours gastric emptying rate (%) was calculated as (20 − No. of residual barium strips in the stomach)/20 × 100%. If the gastric emptying rate was <50%, it was considered that there was a delay in gastric emptying.
-
(3)
Electrogastrogram. A multi-channel electrogastrogram (POLYGRAM NETTM, Medtronic Functional Diagnostics A/S, Denmark) was used for detection. After 12 hours of fasting, the patients took a comfortable supine position. Four recording electrodes were placed on the projection area of the surface of gastric antrum, gastric body, lesser curvature, and greater curvature of the stomach. Then, 30 minutes after the collection of fasting gastric electrical signals, the patients were given a standard meal (whole milk 250 ml and whole wheat bread 100 g, consumed within 15 minutes). After 60 minutes, gastric electrical signals were collected. The observational parameters included: fasting and postprandial dominant frequency (the normal value is 2.88–2.92 cpm); fasting and postprandial dominant power (DP); the percentage of time of normal slow wave rhythm (2.4–3.7 cpm; the normal value is greater >65%); the incidence of abnormal gastric electrical rhythm involving bradygastria (<2.4 cpm), tachygastria (>3.7 cpm), and gastric dysrhythmia.
-
(4)
State of depression and anxiety. Zung's self-rating depression scale (SDS)[13] and self-rating anxiety scale (SAS)[14] were used to evaluate the improvement of patients’ depression and anxiety in the 2 groups before and after intervention. SDS score ≥53 indicated depressive symptoms. SAS score ≥50 indicated anxiety symptoms.
2.4.4. Statistical analysis
SPSS 19.0 (IBM, Armonk, NY) was used for statistical analysis. Continuous data were tested for normal distribution using the Kolmogorov–Smirnov test. Normally distributed continuous data are expressed as means ± standard deviation and were analyzed using the Student t test. Categorical data are expressed as frequencies and were analyzed using the chi-square test. P values <.05 was considered as statistically significant.
2.5. Results
2.5.1. Study population
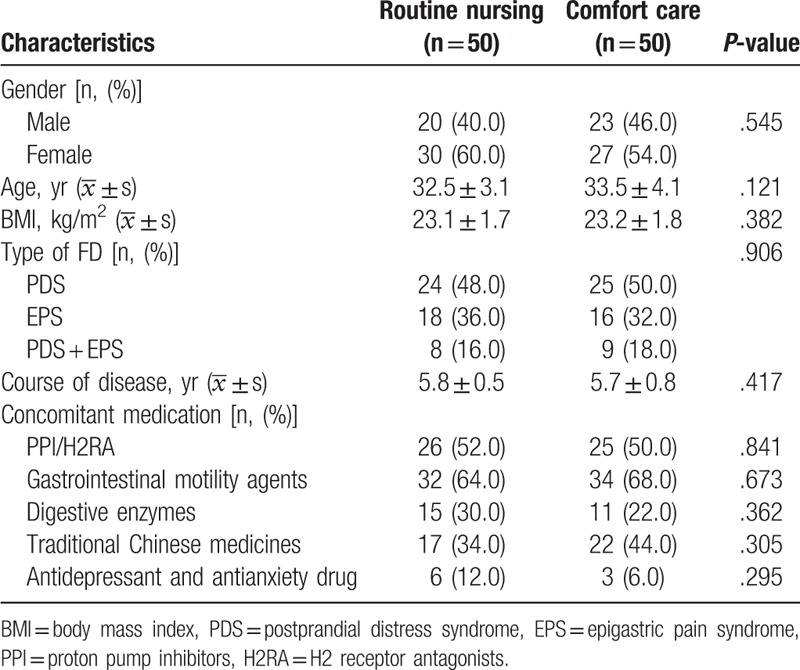
The patient flow chart is shown in Figure 1. There were no statistical differences in gender, age, body mass index, types of FD, course of disease, and concomitant medication between the routine nursing and comfort care groups (P > .05) (Table 1).
Figure 1.
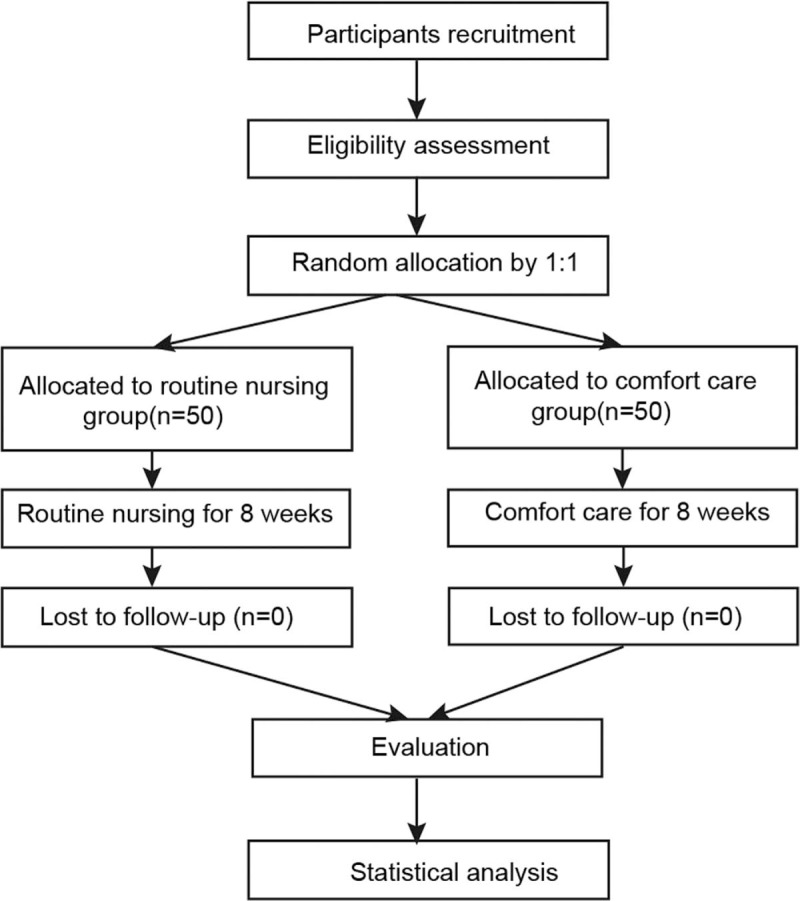
Patient flowchart.
Table 1.
Baseline characteristics of the study population.
2.5.2. Comparison of FD symptom score and gastric emptying rate
As shown in Table 2, the scores of FD symptoms in the routine nursing and comfort care groups before intervention were 14.0 ± 2.6 and 13.8 ± 3.2, respectively (P > .05). After intervention, the scores in 2 groups were decreased to 10.2 ± 2.4 and 8.3 ± 2.4, respectively (P < .001).
Table 2.
Comparison of FD symptom score and gastric emptying rate between the 2 groups before and after intervention  .
.
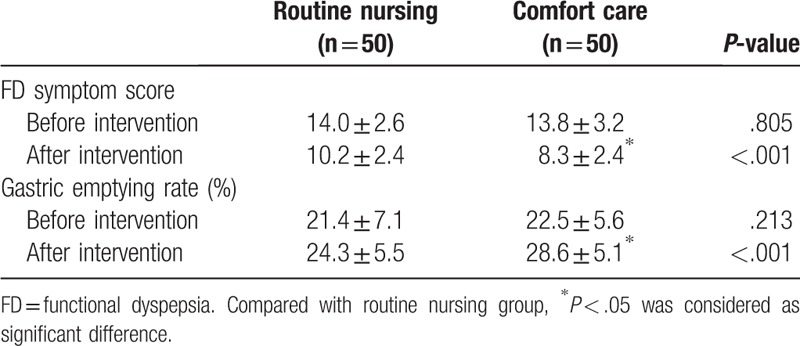
The gastric emptying rate is a common index for the detection rate of gastric motility. Before intervention, gastric emptying rates in the 2 groups were 21.4 ± 7.1% and 22.5 ± 5.6% (P > .05). After intervention, the gastric emptying rates in the 2 groups were increased to 24.3 ± 5.5% and 28.6 ± 5.1%, respectively, and that in comfort care group was significantly increased (P < .001).
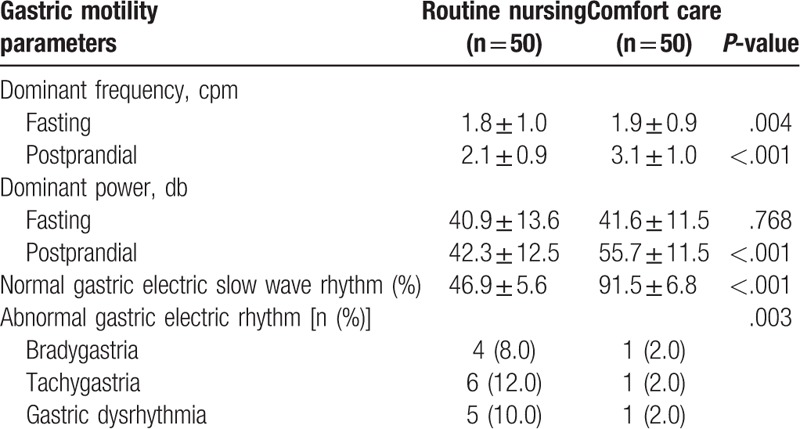
2.5.3. Gastric motility
As shown in Table 3, after intervention, the fasting and postprandial dominant frequencies of electrogastrogram in the routine nursing group were 1.8 ± 1.0 cpm and 2.1 ± 0.9 cpm, respectively, while those in the comfort care group were 1.9 ± 0.9 cpm and 3.1 ± 1.0 cpm, respectively (P < .01). After intervention, the fasting DP of electrogastrogram in the routine nursing group was 40.9 ± 13.6 db, while that in the comfort care group was 41.6 ± 11.5 db (P = .768). After intervention, the postprandial DP of electrogastrogram in the routine nursing group was 42.3 ± 12.5 db, while that in the comfort care group was 55.7 ± 11.5 db (P < .001). After intervention, the percentage of time of normal electrogastrogram slow wave rhythm in the routine nursing group was 46.9 ± 5.6%, while in the comfort care group it was 91.5 ± 6.8% (P < .001). After intervention, in the routine nursing group, there were 4 cases of bradygastria (8%), 6 cases of tachygastria (12%), and 5 cases of gastric dysrhythmia (10%). In the comfort care group, there were 1 case of bradygastria (2%), 1 case of tachygastria (2%), and 1 case of gastric dysrhythmia (2%) (P = .003).
Table 3.
Comparison of gastric motility between 2 groups after intervention  .
.
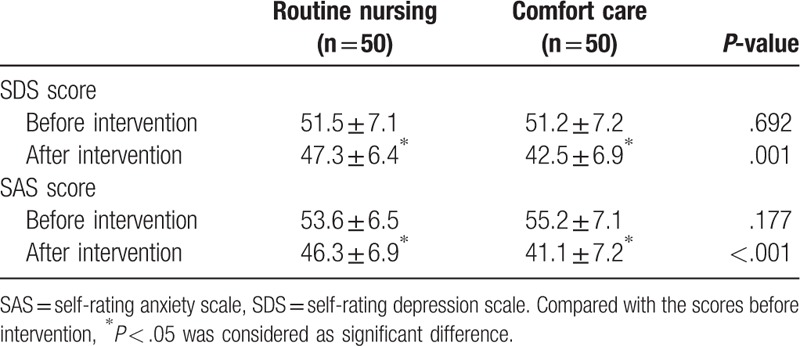
2.5.4. SDS and SAS scores
As shown in Table 4, before intervention, the SDS scores in the routine nursing and comfort care groups were 51.5 ± 7.1 and 51.2 ± 7.2, respectively (P > .05). The SAS scores in the 2 groups were 53.6 ± 6.5 and 55.2 ± 7.1, respectively (P > .05). After intervention, the scores of SDS and SAS in the 2 groups were significantly decreased: the SDS scores of the 2 groups were 47.3 ± 6.4 and 42.5 ± 6.9, respectively (P < .05 vs before intervention) and the SAS scores in the 2 groups were 46.3 ± 6.9 and 41.1 ± 7.2, respectively (P < .05 vs before intervention). After the intervention, the SDS and SAS scores in the comfortable nursing group were lower than those of the routine nursing group, and there were significant differences between the 2 groups (P = .001 and P < .001).
Table 4.
Comparison of SDS and SAS scores between 2 groups before and after intervention  .
.
3. Discussion
The etiology and pathogenesis of FD are complex and not fully clarified. At present, the “Biopsychosocial model” of the pathogenesis of FD is well recognized, that is, psychological factors, social factors, and physiological factors interact and affect each other through enteric nervous signals, which change gastrointestinal motility and sensory function.[8,15,16] The manifestations include gastrointestinal motility disorder and visceral hypersensitivity, leading to various dyspeptic symptoms in FD patients.[8] Due to the heterogeneity of FD, the drug effects of eradicating Helicobacter pylori, inhibiting gastric acid, improving gastrointestinal motility, and antidepressant are limited and the long-term use of the above-mentioned drugs might also lead to adverse effects.[17] In this study, comfort nursing intervention on FD patients was based on the patients as the center, starting from the biological and psychosocial mechanism of FD, and the professional knowledge and skills of nursing care were fully applied to seek and apply the best nursing program, so that patients could reach the most comfortable state in several aspects such as physiology, mental, and social, thereby helping optimize the efficacy of treatment, improve FD symptoms, gastric function and negative emotions, and promote rehabilitation.[6,7,18,19]
The occurrence and development of FD are closely associated with psychosocial factors.[8,15,16] FD patients have more depressive symptoms and stressful life events, and they have less social support. Their depressive symptoms are negatively correlated with interpersonal support.[20,21] FD patients do not effectively respond to stressful life events; when dealing with stressful events, they directly adopt more coping strategies, while coping styles such as transferring attention, acceptance, social support, and relaxation are less used.[20,21] Hartono et al[22] reported that FD patients are susceptible to anxiety, neuroticism, introversion, and other personality characteristics. They are easily stimulated by negative social and psychological factors that will lead to indigestion symptoms and negative emotional expression. Anxiety, depression, and other negative emotions can reduce the patients’ pain threshold, and patient's perception of normal physiological activity is a symptom of disease. Mason[19] pointed out that stressors are all threats that could be perceived, including physical, psychological, social, and cultural stressors. After psychological stressors act on the human brain, the hypothalamus pituitary adrenocortical axis is activated, so that stress hormones such as glucocorticoid and catecholamine are secreted in large quantities, and neurotransmitters in the brain such as serotonin, norepinephrine, and dopamine, or their receptors, decrease, leading to neurohormonal disorders acting on a targeted organ, such as stomach.[23,24] In addition, the blood flow of the gastric mucosa and the secretion of gastric glands are affected, resulting in the decrease of gastric hypersensitivity and pain threshold, as well as causing indigestion symptoms in FD patients.[23,24] When patients are excited, the sympathetic nervous system is excited as well, leading to gastric mucosa vasoconstriction, ischemia and anoxia, reduced secretion by the gastric glands, weakened gastric motility, and delayed gastric emptying; then, the symptoms of digestive tract (eg, the upper abdominal distention, reflux, belching, nausea, vomiting, and early satiety) appear. Conversely, when patients are depressed, the secretion of glucocorticoids is increased, the vagus nerve is excited, the secretion of gastric acid is increased, leading to damage to the gastric mucosa, and the symptoms of early satiety, postprandial upper abdominal pain, and heartburn appear.
The Comfort Theory suggests that nurses should enhance the comfort of patients by controlling environment and help patients adapt to the environment to achieve a relaxed, pleasant, and satisfied state.[19] In the present study, Betty Neuman's system model was applied to carry out nursing care for physiological comfort of FD patients. The system model is a nursing model that investigated the effects of stress on individuals, as well as the individual's regulatory response and the ability to re-establish balance. This model took the recovery of the best health status as a breakthrough point into account, and focused on stressors, stress responses, and the preventive measures against potential and actual stressors.[25] The model is made up of 4 parts, including human, stressor, reaction, and prevention. When the stimulation of the internal and external environment (ie, the stressors) act on the body, the body controls and deals with defense function, that is, elastic defense line, normal line of defense, resistance line, and basic structure. In order to improve the coping ability of the body, it is necessary to apply the mentioned 3-level prevention mechanism to control stressors and enhance the function of defense system, so as to help the patients maintain or restore the balance and stability of the system, and to achieve the best health state. By assessing the patients’ actual and potential stressors, a primary preventive measure is taken to reduce or avoid contact between patients and stressors, as well as to consolidate the elastic defense line and normal defense line. For patients who have been stressed, secondary prevention is taken to enhance the resistance line, reduce and eliminate stress response, and to assist the body to rebuild and restore. When the stress response of patients is gradually reduced, 3-level preventive measures (eg, nurse's professional social support) is provided to maximize the use of individual's internal and external resources to further maintain the patients’ stability and help patients restore to the maximum health until they reach or even exceed the health level that stressors do not break through the normal line of defense. The Betty Neuman's system model emphasizes on primary prevention.[25] In a certain period, nurses should pay attention to various stressors of the patients, sort out the extent of their impact on the body, and formulate corresponding preventive measures.
The Comfort Theory believes that the improvement of comfort is mutually promoted by the behavior of patient's seeking for health, including internal behavior such as the enhancement of confidence in the fight against the disease, and an external behavior (eg, actively cooperating with various treatments and nursing).[18] Depressive mood has the most significant negative effect on individual's confidence level, while coping style may have both positive and negative benefits on an individual's confidence.[26] Therefore, in this study, positive psychological intervention was applied to perform mental and psychological comfort nursing care to FD patients. Positive mental intervention means that the positive emotions of human can be induced by some actions or activities. Seligman[17] pointed out that the goal of positive psychology is to promote psychology to focus on repairing problems in life, and simultaneously, it is to devote to build good qualities in life. Even those with the most serious mental illness require more than just a simple pain relief. People in confusion need more satisfaction, pleasure, and happiness. People need to build strength rather than just correct defects. People need meaningful and purposeful life. Accordingly, these items will not be automatically generated by the relief of pain.[27] Attribution intervention belongs to the category of positive psychology, which is actually the training for the attribution style of patients. FD patients tend to have negative attribution style, that is, positive events are attributable to external, unstable, and specific reasons, and negative events are attributable to internal, stable, and overall reasons. Patients always tend to focus on negative news that is bad for their own health, sometimes they even magnify negative information, and think that the condition is uncontrollable. Self-acceptance is low, leading to psychological imbalance and negative emotions.[3,28] Through actively attributable intervention to patients, nurses can correct or improve the patients’ inappropriate attribution style, thus further correct patient's bad cognition and negative emotion. Gratitude intervention is a positive psychological intervention as well. Nurses often instruct FD patients to express their gratitude, which makes it more easy for patients to notice positive events that happen around them and to experience positive emotions. As patients regularly experience all kinds of positive emotions, the patients’ mood is better, so they are more able to experience happiness. Gratitude intervention could also improve patient's ability to deal with all kinds of negative emotional problems and expand their social communication network, thereby alleviating negative emotions such as depression.
According to the Comfort Theory,[6] a social support system is an intermediate variable that affects the comfort level of the patients. In this study, by providing nursing professional social support, social comfort nursing was implemented to FD patients and the results were consistent with the theoretical hypothesis. Social support is an individual's available external resource, satisfactory social support is beneficial to health, improves patient's ability to foresight ability and coping skill for disease prevention, and presents a lower state of depression and anxiety, which is beneficial to the improvement of prognosis.[29] The support provided by professional medical staff can reduce the degree of disease invasion, improve the patients’ self-health level with chronic diseases, and increase patients’ degree of trust toward medical staff.[30] As the most frequently contacted professional medical staff with patients during hospitalization, nurses are important human resource for patients to carry out professional social support.[31] According to the medical outcomes study social support survey,[32] in this study, through communicative and evaluative communication, nurses accurately grasped the size of FD patient's medical support network. Intervention communication helped patients obtain information and emotional support from nurses in addition to the practical support in living care and mass economy from family, relatives, units, and so on. Nurses gave patient's family members correct care methods to improve the coping ability of patient's family to the disease and helped patients gain more social interaction and emotional support, thus improved the ability of FD patients to cope with and adapt to the disease.
The results showed that the comfortable nursing group was superior to the routine nursing group regarding the relief of dyspepsia symptoms and recovery of gastric function. Because mental and psychological factors and stress can cause digestive dysfunction by affecting the brain-gut axis, the patients developed various symptoms of dyspepsia. The dyspeptic symptoms can also act on mental and psychological functions through the brain gut axis, causing or aggravating depression and anxiety of the patients, and thus inducing a vicious circle. In the present study, the symptoms of dyspepsia in both groups were alleviated after the intervention, and the adverse effects of the physiological abnormalities on mental health were alleviated to varying degrees. Therefore, the SDS and SAS scores in the 2 groups were significantly lower than those before the intervention. Nevertheless, the comfortable nursing group outperformed the routine nursing group in terms of improving mental state by further implementing targeted nursing interventions.
Limitations of this study include the relatively short (8 weeks) intervention time and follow-up time. This was a single center study and case selection bias might exist. Finally, some drugs had to be used in some patients to relieve depression and anxiety and they are known to affect FD[33]; however, these drugs could not be withdrawn to ensure the best patient health care. In the future, sample size will be expanded and long-term follow-up observation will be carried out in order to improve FD comfort care program and provide reference for other patients with functional diseases of digestive system.
In conclusion, this study aimed at the characteristics of “All diseases originate from the mind” in FD patients. Under the guidance of the Comfort Theory, the best nursing program was applied in the aspects of physiological, mental, and social comfort, which not only achieved the purposes of optimizing the treatment effects and improving the quality of FD patients’ life, but also expanded the practice scope of nursing specialty, and embodied the professional value of nurses.
Author contributions
Conceptualization: Yu Xiong, Hui Xing.
Data curation: Yu Xiong, Hui Xing, Lingzhi Hu, Jinzhi Xie.
Project administration: Lingzhi Hu, Jinzhi Xie.
Writing – original draft: Yu Xiong, Hui Xing, Yuan Liu, Deying Hu.
Footnotes
Abbreviations: DP = dominant power, DSS = dyspepsia symptom score, FD = functional dyspepsia, SAS = self-rating anxiety scale, SDS = self-rating depression scale.
This study was approved by the ethics committee of Wuhan Union Hospital, and all the patients signed informed content.
The study was supported by the National Natural Science Foundation of China (No. 71673100) and Hubei Natural Science Foundation Project (No. 2015CFB674).
The authors have no conflicts of interest to disclose.
References
- [1].Ford AC, Marwaha A, Sood R, et al. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut 2015;64:1049–57. [DOI] [PubMed] [Google Scholar]
- [2].Mertz H. Rome II: the functional gastrointestinal disorders. Gastroenterology 2001;121:1523–4. [Google Scholar]
- [3].Aro P, Talley NJ, Johansson SE, et al. Anxiety is linked to new-onset dyspepsia in the Swedish population: a 10-year follow-up study. Gastroenterology 2015;148:928–37. [DOI] [PubMed] [Google Scholar]
- [4].Olafsdottir LB, Gudjonsson H, Jonsdottir HH, et al. Natural history of functional gastrointestinal disorders: comparison of two longitudinal population-based studies. Dig Liver Dis 2012;44:211–7. [DOI] [PubMed] [Google Scholar]
- [5].Agreus L, Svardsudd K, Talley NJ, et al. Natural history of gastroesophageal reflux disease and functional abdominal disorders: a population-based study. Am J Gastroenterol 2001;96:2905–14. [DOI] [PubMed] [Google Scholar]
- [6].Kolcaba KY. A theory of holistic comfort for nursing. J Adv Nurs 1994;19:1178–84. [DOI] [PubMed] [Google Scholar]
- [7].Pinto S, Caldeira S, Martins JC, et al. Evolutionary analysis of the concept of comfort. Holist Nurs Pract 2017;31:243–52. [DOI] [PubMed] [Google Scholar]
- [8].Drossman DA, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology 2016;150:1257–61. [DOI] [PubMed] [Google Scholar]
- [9].Gastrointestinal Dynamics Group of Chinese Society of Gastroenterology. Cooperative group of functional gastrointestinal diseases of Chinese Society of Gastroenterology. China Consensus on functional dyspepsia (2015, Shanghai). Chin J Dig 2016;36:217–29. [Google Scholar]
- [10].Keshteli AH, Feizi A, Esmaillzadeh A, et al. Patterns of dietary behaviours identified by latent class analysis are associated with chronic uninvestigated dyspepsia. Br J Nutr 2015;113:803–12. [DOI] [PubMed] [Google Scholar]
- [11].Jitske T, Erin G, Maarten V, et al. Illness perceptions and coping determine quality of life in COPD patients. Int J Chron Obstruct Pulmon Dis 2016;11:2001–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cassell B, Gyawali CP, Kushnir VM, et al. Beliefs about GI medications and adherence to pharmacotherapy in functional GI disorder outpatients. Am J Gastroenterol 2015;110:1382–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zung WW. A self-rating depression scale. Arch Gen Psychiatry 1965;12:63–70. [DOI] [PubMed] [Google Scholar]
- [14].Zung WW. A rating instrument for anxiety disorders. Psychosomatics 1971;12:371–9. [DOI] [PubMed] [Google Scholar]
- [15].Talley NJ, Ford AC. Functional dyspepsia. N Engl J Med 2015;373:1853–63. [DOI] [PubMed] [Google Scholar]
- [16].Moayyedi PM, Lacy BE, Andrews CN, et al. ACG and CAG clinical guideline: management of dyspepsia. Am J Gastroenterol 2017;112:988–1013. [DOI] [PubMed] [Google Scholar]
- [17].Lacy BE, Talley NJ, Locke GR, 3rd, et al. Review article: current treatment options and management of functional dyspepsia. Aliment Pharmacol Ther 2012;36:3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kolcaba K. Evolution of the mid range theory of comfort for outcomes research. Nurs Outlook 2001;49:86–92. [DOI] [PubMed] [Google Scholar]
- [19].Kolcaba KY. A taxonomic structure for the concept comfort. Image J Nurs Sch 1991;23:237–40. [DOI] [PubMed] [Google Scholar]
- [20].De la Roca-Chiapas JM, Solis-Ortiz S, Fajardo-Araujo M, et al. Stress profile, coping style, anxiety, depression, and gastric emptying as predictors of functional dyspepsia: a case-control study. J Psychosom Res 2010;68:73–81. [DOI] [PubMed] [Google Scholar]
- [21].Fang YJ, Liou JM, Chen CC, et al. Distinct aetiopathogenesis in subgroups of functional dyspepsia according to the Rome III criteria. Gut 2015;64:1517–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hartono JL, Mahadeva S, Goh KL. Anxiety and depression in various functional gastrointestinal disorders: do differences exist? J Dig Dis 2012;13:252–7. [DOI] [PubMed] [Google Scholar]
- [23].Mayer EA. The neurobiology of stress and gastrointestinal disease. Gut 2000;47:861–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jing FC, Zhang J, Feng C, et al. Potential rat model of anxiety-like gastric hypersensitivity induced by sequential stress. World J Gastroenterol 2017;23:7594–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Fawcett J, Foust JB. Optimal aging: a Neuman systems model perspective. Nurs Sci Q 2017;30:269–76. [DOI] [PubMed] [Google Scholar]
- [26].Lakey CE, Hirsch JK, Nelson LA, et al. Effects of contingent self-esteem on depressive symptoms and suicidal behavior. Death Stud 2014;38:563–70. [DOI] [PubMed] [Google Scholar]
- [27].Duckworth AL, Steen TA, Seligman ME. Positive psychology in clinical practice. Annu Rev Clin Psychol 2005;1:629–51. [DOI] [PubMed] [Google Scholar]
- [28].Adibi P, Keshteli AH, Daghaghzadeh H, et al. Association of anxiety, depression, and psychological distress in people with and without functional dyspepsia. Adv Biomed Res 2016;5:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Samorinha C, Fraga S, Alves E, et al. Self-reported psychosocial factors among in vitro fertilization patients interviewed alone or with the partner. Psychol Health Med 2016;21:1–8. [DOI] [PubMed] [Google Scholar]
- [30].Absolom K, Holch P, Pini S, et al. The detection and management of emotional distress in cancer patients: the views of health-care professionals. Psychooncology 2011;20:601–8. [DOI] [PubMed] [Google Scholar]
- [31].Neri L, Brancaccio D, Rocca Rey LA, et al. Social support from health care providers is associated with reduced illness intrusiveness in hemodialysis patients. Clin Nephrol 2011;75:125–34. [DOI] [PubMed] [Google Scholar]
- [32].Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705–14. [DOI] [PubMed] [Google Scholar]
- [33].Jackson JL, O’Malley PG, Tomkins G, et al. Treatment of functional gastrointestinal disorders with antidepressant medications: a meta-analysis. Am J Med 2000;108:65–72. [DOI] [PubMed] [Google Scholar]


