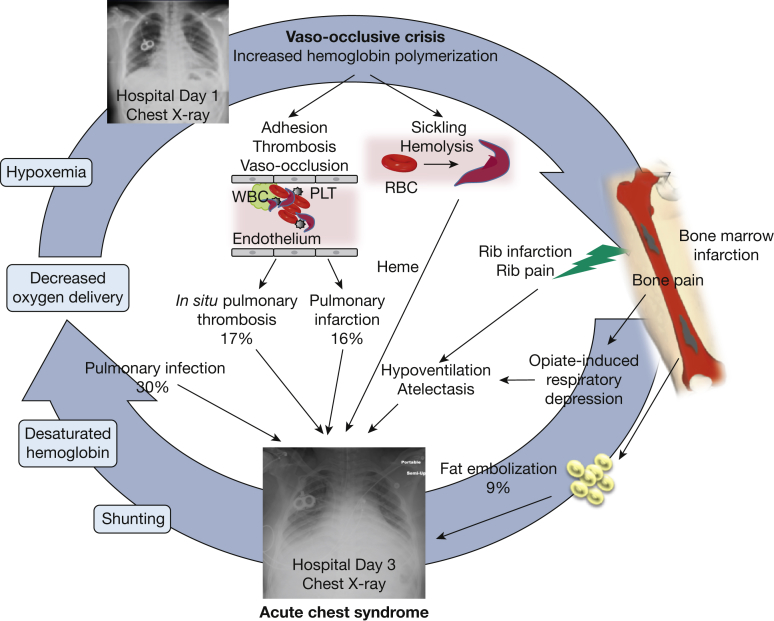
Figure 1.
Causes and mechanisms of acute chest syndrome (ACS). Vaso-occlusive crises precede ACS in 80% of cases and are characterized by red blood cell sickling, cellular hyperadhesion, hemolysis, and vaso-occlusion. These processes are responsible for acute pain and bone marrow necrosis. ACS typically occurs 2.5 days after hospitalization for a vaso-occlusive episode, and radiographically presents as new infiltrates on a chest radiograph. Common causes include fat embolization from necrotic marrow (9% of cases), pulmonary infection (30% of cases), pulmonary infarction (16%), and hypoventilation. In situ pulmonary thrombosis has been identified in 17% of patients with ACS and may also be responsible for infarction. Animal models have shown that by-products of hemolysis, such as heme, cause experimental ACS. As a result of lung injury, ventilation-perfusion mismatches and shunting ensue, with subsequent hemoglobin desaturation and hypoxemia. Tissue hypoxia in turn triggers further sickling in a vicious cycle. The chest radiographs are those of a patient with SCD who received chronic exchange transfusions (note the presence of a double-lumen “port”) on hospital day 1 (top) and day 3 (bottom). By day 3 extensive infiltrates had developed in the patient, who required endotracheal intubation for respiratory failure. PLT = platelet.
Adapted with permission from Bope and Kellerman.27a