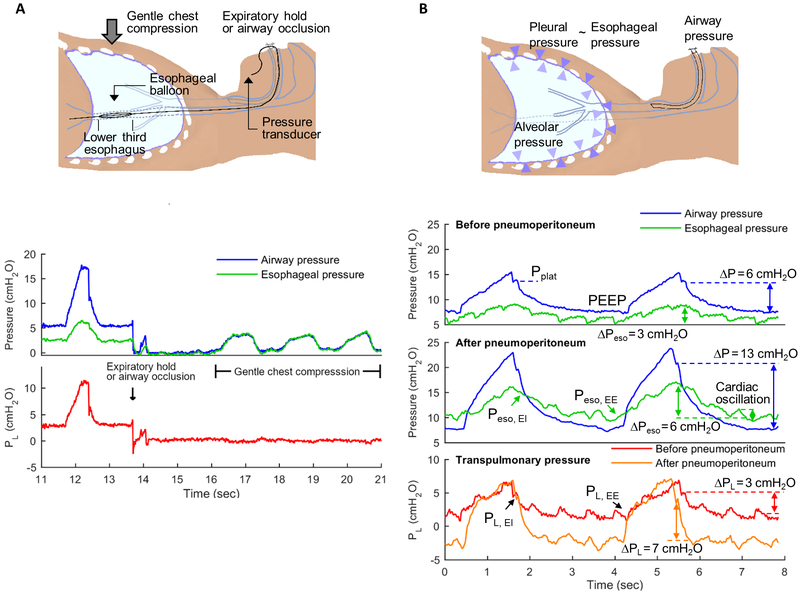
Fig.2.
Airway opening, esophageal (Peso) and transpulmonary pressures (PL) measurements. PL is defined as the difference between airway opening pressure (blue lines) and pleural pressure. Pleural pressure is frequently estimated from esophageal balloon pressure measurements (Peso). Using a specific protocol, the esophageal balloon is placed in the lower third of the esophagus (2A). Cardiac oscillations in Peso (2B, green lines) indicate accurate placement of the balloon, which can be confirmed by observation of similar airway pressure and Peso measurements as gentle chest compressions are performed during expiratory pause or with occluded airway opening (2A). PL can be estimated as the difference between airway and esophageal pressures (red and orange lines). Interventions such as pneumoperitoneum (2B, mid panel) produce a marked change in driving pressures (ΔP = plateau pressure, PPlat, minus positive end-expiratory pressure, PEEP). In this example, ΔP increased by 7 cmH2O. Yet, delta PL (end-inspiratory PL, PL EI, minus end-expiratory PL, PL EE) does not increase to the same degree as ΔP and PPlat. The change in delta PL in this example was 4 cm H2O. This demonstrates that part of the increase in ΔP and PPlat are due to the chest wall component and not to pressures applied to the lung parenchyma. This contribution of the chest wall is evidenced by the increased end-inspiratory (EI) to end-expiratory (EE) oscillation in Peso after as compared to before pneumoperitoneum. In addition, the esophageal pressure at end-expiration (Peso EE, at ~4 seconds on time scale) is positive before pneumoperitoneum while it is negative after pneumoperitoneum. This implies mechanical conditions consistent with lung collapse after pneumoperitoneum. Indeed, while PL did not increase by the same magnitude as ΔP, it also increased, indicating loss of lung compliance. Such conditions could prompt use of higher PEEP to prevent lung derecruitment.