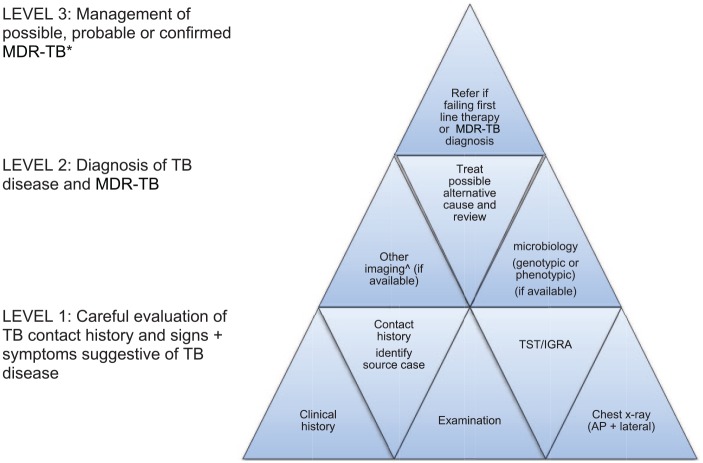
Figure 2.
A matrix approach to diagnose MDR-TB in children†.
AP, anteroposterior; IGRA, interferon gamma release assay; MDR-TB, multidrug resistant tuberculosis; TST, tuberculin skin test.
†Start at level 1 and obtain as much information as possible to fill the pieces. The more level 1 and 2 pieces that fit together, the more secure the MDR-TB diagnosis; concept adapted from Seddon J. International Child TB training course, Desmond Tutu TB centre Stellenbosch University, 2018.
*Provide treatment based on the drug susceptibility testing results of the likely source case, if no guidance is available from the child’s own specimens. The decision to treat should balance the likelihood of active disease and disease progression risk against the toxicity, cost and inconvenience of treatment. The following definitions apply.
Possible MDR-TB: TB symptoms and/or signs and/or radiology and child not improving after 2–3 months of first-line treatment or close contact with a patient who died from TB or failed TB treatment.
Probable MDR-TB: TB symptoms and/or signs and/or radiology with documented recent exposure to an infectious MDR-TB case.
Confirmed MDR-TB: MDR-TB strain isolated from a child.
^Computed tomography (CT), magnetic resonance imaging (MRI) and/or positron emission tomography (PET) depending on clinical symptoms and signs, as well as the cost, availability and radiation exposure of different modalities.