Abstract
Background:
The Knee Injury and Osteoarthritis Outcome Score (KOOS) has demonstrated inferior psychometric properties when compared to the International Knee Documentation Committee Subjective Knee Form (IKDC). The KOOS, Joint Replacement (KOOS,JR) is a validated short-form instrument to assess patient-reported outcome measures (PROs) after knee arthroplasty, and the purpose of this study was to determine if augmenting the KOOS,JR with additional KOOS items would allow for the creation of a short-form KOOS-based global knee score for patients undergoing anterior cruciate ligament (ACL) reconstruction with psychometric properties similar to that of the IKDC.
Hypothesis:
We hypothesized that an augmented version of the KOOS,JR could be created that would demonstrate convergent validity with the IKDC but avoid the ceiling effects and limitations previously noted with several of the KOOS subscales.
Study Design:
Cohort study. Level of Evidence: Diagnostic, Level II.
Methods:
Using pre- and 2-year postoperative responses to the KOOS questionnaires from a sample of 1,904 primary ACL reconstruction patients, an aggregate score combining the KOOS,JR and the 4 KOOS Quality of Life questions, termed the KOOSglobal, was developed. Again using the pre- and postoperative responses from the 1,904 ACL reconstruction patients, psychometric properties of the KOOSglobal were compared to the IKDC Subjective Score. Convergent validity between the KOOSglobal and IKDC was assessed with a Spearman correlation (rho). Responsiveness of the 2 instruments was assessed by calculating the pre- to effect size (ES) and relative efficiency (RE). Finally, the presence of a preoperative floor or postoperative ceiling effect was defined using the threshold of 15% of patients reporting either the worst possible (0 for both KOOSglobal and IKDC) or best possible scores (100 for both KOOSglobal and IKDC), respectively.
Results:
The newly developed KOOSglobal was responsive after ACL reconstruction and demonstrated convergent validity with the IKDC. The KOOSglobal significantly correlated with IKDC scores (rho=.91, p<.001), explained 83% of the variability in IKDC scores, and was similarly responsive (RE=.63). While there was a higher rate of perfect postoperative scores with the KOOSglobal (213/1904, 11%) than IKDC (6%), KOOSglobal was still below the 15% ceiling effect threshold.
Conclusions:
The large ceiling effect limits the ability to use of several of the KOOS subscales in the younger, more active ACL patient population. However, by creating an aggregate score from the KOOS,JR and the 4 KOOS Quality of Life questions, the 11-item KOOSglobal offers a responsive PRO tool after ACL reconstruction that converges with the information captured with the IKDC. Also, by offering the ability to calculate multiple scores from a single questionnaire, the 11-item KOOSglobal may potentially provide the orthopedic community a single PRO platform to be used across knee-related subspecialties.
Keywords: knee, anterior cruciate ligament, outcome, responsiveness
Introduction
Patient-reported outcomes measures, such as the Knee Injury and Osteoarthritis Outcome Score (KOOS), have provided invaluable information to researchers about the relative success of orthopedic interventions.3, 21, 31, 32 However, while important research tools, to date these tools have not been practical for clinicians to incorporate into their daily practices due to the number of questions and both the time required of the patient to complete as well as the time of the clinic staff to record. In anticipation of mandatory physician quality reporting for arthroplasty surgeons and the ensuing burden that will create, Lyman et al. recently validated the KOOS Joint Replacement, or KOOS,JR.24 The KOOS,JR is a global score generated from a subset of seven questions from the full version of the 42-question KOOS that provides clinicians with an efficient and responsive tool to evaluate postoperative patient-reported outcomes (PROs) following total knee arthroplasty (TKA) procedures.24
There are clear advantages of a valid and responsive outcome measure that can be generated from a limited number of questions. Meaningful clinical data can be generated but with less burden to the patient, surgeon, and clinical staff. This also creates the potential for PROs to more easily be incorporated into electronic medical records systems. Despite these advantages, the logistical challenges of using multiple PRO tools across knee-related subspecialties continues to be a barrier to widespread collection of PROs in the clinical setting.
The ideal scenario would be a single PRO platform that could be used across knee-related subspecialties to reduce logistical barriers to PRO collection. The KOOS,JR has been demonstrated to be a valid and efficient measure of patient-reported outcomes after knee arthroplasty; however, it is unlikely the KOOS,JR would be a valid and responsive PRO tool when administered to a younger, more active population of patients undergoing anterior cruciate ligament (ACL) reconstruction since the KOOS,JR was developed with knee arthroplasty patients. Therefore, the purpose of this study was to determine if augmenting the KOOS,JR with additional KOOS items would allow for the creation of a short-form KOOS-based global knee score for patients undergoing anterior cruciate ligament (ACL) reconstruction with psychometric properties similar to that of the IKDC. We hypothesized that an augmented version of the KOOS,JR could be created that would demonstrate convergent validity with the IKDC but avoid the ceiling effects and limitations previously noted with several of the KOOS subscales.
Methods
The study included 2,020 patients that underwent unilateral primary ACL reconstruction between 2002 and 2008 that had consented to participate in a multi-center, IRB-approved prospective cohort (Vanderbilt University IRB protocol #990426). All patients were included with the exception of patients undergoing revision ACL reconstruction or those that incurred a subsequent graft failure or additional ipsilateral reoperation at the time of their 2-year follow-up. Patients were not excluded based on age, sex, race, or the presence of concomitant injury. There was a subset of 116 patients with incomplete IKDC information that were excluded leaving a total sample of 1,904 patients in the current analysis (1904/2020 = 94% of the available sample).
Methods similar to the original KOOS,JR validation study were employed to determine if an augmented version of the KOOS,JR could be created that would demonstrate similar psychometric properties as the IKDC.24 First, the specific KOOS subscales that did not correlate well with the KOOS,JR were identified. This was done on the premise that questions from these subscales would provide unique information not already provided by questions already included in the KOOS,JR as evidenced by the lower correlations with the KOOS,JR score. Individual questions within the identified subscale(s) were then selected if > 67% of patients had preoperative responses of “moderate” or greater.24 Once additional questions were identified, an aggregate score of the seven KOOS,JR questions and any additional questions, termed the KOOSglobal, was calculated using methods similar to a recent study involving the Hip disability and Osteoarthritis Outcome Score.13 We applied a Rasch measurement model29 to the pre-operative and post-operative data using both the KOOS,JR and KOOSglobal. The data were stacked35, 36 in order to examine the entire range of patient outcomes rather than examine pre-operative and post-operative separately, and the analysis was conducted using the Rasch Partial Credit model26, 38 available in Winsteps Rasch Measurement Software version 3.81.0 (Winsteps, Beaverton, OR) These analyses can be performed with missing values, and as such, we were able to include all 2,020 patients. Details regarding the methods used in the Rasch analysis, item inclusion and exclusion, and comparative results of the KOOS,JR and KOOSglobal can be found in the accompanying electronic Supplemental files.1, 20, 33, 37
Both the convergent validity and responsiveness of the KOOSglobal in relation to the IKDC were assessed.10, 11, 16, 17, 25, 27, 34 The convergent validity and equivalence of the KOOSglobal were examined using the IKDC Subjective Score as the “gold standard.” In order to be considered to be equivalent to the IKDC, the KOOSglobal must demonstrate a Spearman correlation > 0.90 with the IKDC.10, 16, 25 The correlation was then squared (rho2) to determine the percentage of the variability in the IKDC that was explained by the KOOSglobal.
The pre- to postoperative responsiveness of the KOOSglobal was assessed and compared to the IKDC by calculating effect size (ES) and relative efficiency (RE).16, 18, 27 ES represents the average pre- to postoperative change divided by the standard deviation of the preoperative scores. Large ES are defined as those > 0.8, and ES differences between the KOOSglobal and IKDC < 0.3 were considered to be representative of similar responsiveness.8, 16 RE is a ratio of the pre- to postoperative t-statistics of the KOOSglobal and IKDC [RE = (tKOOSglobal/tIKDC)2].17, 18 RE values > 0.6 were considered to be indicative of the KOOSglobal being similarly responsive as the IKDC.16 The presence of a preoperative floor or postoperative ceiling effect was defined using the threshold of 15% of patients reporting either the worst possible (0 for both KOOSglobal and IKDC) or best possible scores (100 for both KOOSglobal and IKDC), respectively.19
Results
One additional question from the KOOS Sport/Recreation subscale and four questions from the KOOS Quality of Life subscales were identified due to the low correlations between the KOOS,JR and these items. More than 67% of patients had preoperative responses of “moderate” or worse to all four questions from the Quality of Life subscale, thus all four items met the threshold for inclusion. While 71% of patients reported at least moderate difficulty when responding to the Sport/Recreation question regarding twisting and pivoting, consistent with the methods of Lyman et al.,24 this question was not added to the KOOSglobal as the KOOS,JR already included a question related to pain during this specific task.
Pre- and postoperative KOOSglobal scores were then calculated by combining the responses from the four Quality of Life questions with the seven KOOS,JR questions. Similar to the scoring of the KOOS,JR, the responses to the 11 KOOSglobal were summed to generate a raw score, and the raw score was then converted using a logit transformation. The KOOSglobal questionnaire, scoring instructions, and details related to the logit transformation used to transform raw scores can be found in Figures 1 and 2. For the KOOSglobal score, the lowest possible raw score which would be indicative of no pain or dysfunction (0/44) was scaled to 100 and the highest possible raw score (44/44), which is indicative of extreme pain and dysfunction was scaled to 0.
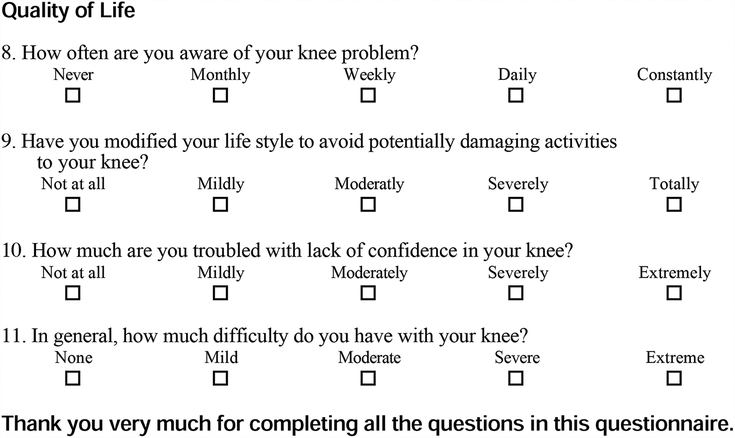
Figure 1.
KOOSglobal questionnaire. Questions identified with an asterisk are those that would be scored to calculate the KOOS,JR.
Figure 2.
KOOSglobal scoring instructions.
The KOOSglobal met the thresholds for both convergent validity and responsiveness to be considered sufficiently equivalent to the IKDC. The KOOSglobal significantly correlated with IKDC scores (rho = 0.91, p < 0.001), and explained 83% of the variability in IKDC scores. KOOSglobal scores significantly increased between the preoperative and 2-year postoperative follow-ups (Preoperative = 53.3 ± 9.7, Postoperative = 73.3 ± 14.6, p < 0.001, ES = 2.1). Furthermore, the responsiveness of the KOOSglobal did not dramatically differ from that of the IKDC (RE = 0.63). While there was a higher rate of perfect postoperative scores with the KOOSglobal (213/1904, 11%) than IKDC (6%), KOOSglobal was still below the 15% ceiling effect threshold. There was no evidence of a ceiling effect preoperatively (4/1904, <1%), or a floor effect either prior to (0/1904) or following surgery (0/1904) with KOOSglobal (Table 1).
Table 1.
Pre- and 2-year postoperative KOOS, JR, KOOSglobal, and IKDC scores (mean ± standard deviation) from 1,904 ACL reconstruction patients
| KOOSglobal | IKDC | |
|---|---|---|
| Preoperative | 53.3 ± 9.7 | 51.7 ± 17.0 |
| Scores of 0 (n, %) | 0 (0%) | 1 (<1%) |
| Scores of 100 (n, %) | 4 (<1%) | 4 (<1%) |
| Postoperative | 73.3 ± 14.6 | 83.2 ± 15.3 |
| Scores of 0 (n, %) | 0 (0%) | 0 (0%) |
| Scores of 100 (n, %) | 213 (11%) | 122 (6%) |
| Pre/post t statistic | 59.71 | 74.96 |
| Effect size | 2.1 | 1.8 |
Discussion
By creating an aggregate score of the KOOS,JR and KOOS Quality of Life questions, the 11-item KOOSglobal demonstrated convergent validity with the 19-item IKDC and was responsive in a population of ACL reconstruction patients. The current results have implications both for those implementing PROs into their clinical practice but also for groups that have collected KOOS questionnaires from large volumes of ACL patients. For example, several national ACL reconstruction registries utilize the KOOS to assess patient-reported outcomes. As indicated in Part I of this two-part series, the KOOS ADL, Sports, and Symptom subscales have psychometric limitations when administered in the ACL reconstruction patient population. In addition, the traditional KOOS scoring does not allow for a single score to be calculated to represent the overall condition of the knee. The KOOSglobal appears to avoid the psychometric limitations of the ADL, Sports, and Symptoms subscales while providing information that is substantially similar to that provided by the IKDC. As a result, groups or registries that have utilized the KOOS for a number of years may now have an efficient method to compare their results to those that have utilized the IKDC, while avoiding the ceiling effects and large minimal detectable change values previously demonstrated by some of the KOOS subscales when administered after ACL reconstruction.
In 2016, the American Academy of Orthopaedic Surgeons’ Quality Outcomes Data Work Group released a list of recommended PRO tools based on anatomical region and diagnosis.14 The IKDC was identified as the consensus recommended tool to assess outcomes for ACL-injured or reconstructed patients, whereas the KOOS and KOOS,JR were recommended for those with knee osteoarthritis.14 The Work Group stated that the initial list was intended to steer data collection and reporting, but further stated that they anticipated that the list could change over time.14 While these recommendations provided initial guidance, barriers to implementation arise if clinically adopting these recommendations to longitudinally follow ACL reconstruction patients over time when we know many ACL patients will progressively transition into the osteoarthritis patient population.6 This issue arises when one asks the question, “When does an ACL patient become and osteoarthritis patient?” Similarly then, when is it appropriate to transition from one tool to the other? This designation has historically been based on radiographic changes or degenerative defects noted on MRI.6 However, one of the advantages of longitudinal PRO collection is that it can be done remotely and without the need for additional imaging. As such, it is simply not feasible to tie the decision of whether to use the IKDC or KOOS based on imaging results. In the absence of a clear definition of when to stop the use of the IKDC and begin using the KOOS or KOOS,JR with a given patient, the KOOSglobal could seamlessly bridge the gap as patients transition from being considered an ACL patient to being considered an osteoarthritis patient. Furthermore, this can be accomplished in an efficient manner with the 11-item KOOSglobal compared to 19-item IKDC or 42-item KOOS. Longer PRO questionnaires have been associated with reduced patient response rates when compared to shorter questionnaires provided that both tools provide similar content.30 The brevity of the KOOSglobal does not appear to come at a cost in terms of lost information as the KOOSglobal converged with the IKDC and showed similar responsiveness. An added bonus of a validated KOOSglobal that is only 11 questions in length is the possibility of alternative platforms for soliciting short, intermediate, and long-term follow-up such as text messaging. Anthony et al. evaluated text messaging for delivery of the patient questionnaires in the early postoperative period, and reported > 85% follow-up at virtually no cost.2 Similarly, Blocker et al. utilized text messaging to follow arthroplasty patients at greater than two years follow-up and concluded that text messaging is viable avenue for following patients long-term.4
It is important to note that we are in no way suggesting that the KOOSglobal platform be considered a stand-alone replacement for the full KOOS in the research arena, nor do we believe that the KOOSglobal should somehow supplant the KOOS,JR as a PRO tool in the arthroplasty patient population. The volume of TKAs has continued to rise in the United States, with more than 700,000 patients undergoing the procedure on an annual basis.5, 15 This patient volume, combined with potential mandated reporting of PROs as part of the CMS pay-for-performance measures,7 may place a significant burden on orthopedic practices in terms of both the costs and resources necessary to collect this information.9 The KOOS,JR was developed to provide arthroplasty surgeons with an efficient method to capture clinically-meaningful PROs.24 While not as prevalent as osteoarthritis, ACL injuries are common, affecting approximately 250,000 people in the United States each year.12 ACL injury appears to initiate the cascade of post-traumatic osteoarthritis, with more than 50% demonstrating arthritic changes five to 15 years after injury.22, 23, 28 As ACL injury appears to be a possible first step down the path towards osteoarthritis, few global PRO assessment tools allow for evaluation across the spectrum of disease progression.
The 11 questions identified in the current study allow the clinician to independently calculate a KOOSglobal (scored using all 11 questions), KOOS,JR score (7 questions) and KOOS-Quality of Life subscale (4 questions). The principal advantage of using the KOOSglobal questionnaire as a PRO platform is the versatility to be used across a variety of knee patient populations. In addition, the KOOSglobal potentially alleviates some of the logistical barriers to routine PRO collection. These 11 questions take less than five minutes to complete, minimizing the burden to the patient. A single PRO questionnaire may also reduce the burden to the orthopedic practice. Front office staff would not need to differentiate which PRO questionnaire to give each patient when compared to a scenario in which multiple PRO tools were being used to evaluate different patient populations. For example, the front office staff for a clinician that normally sees both sports and osteoarthritis patients during the course of clinic day would not have to determine which PRO tool to give each knee patient, but rather, could use the KOOSglobal questionnaire for adult knee patients. Similarly, for a multi-subspecialty practice in which surgeons of different subspecialties utilize the same staff and clinic space on different days, the front office staff would not have to remember which PRO tool to use on Monday versus Tuesday, but again, could use the KOOSglobal questionnaire for adult knee patients. A single questionnaire can be given to adult knee patients, and then scored differently based on whether the patient had an ACL reconstruction (scored using all 11 KOOSglobal questions) or had a total knee arthroplasty (scored using the 7 KOOS,JR questions within the KOOSglobal questionnaire).
Furthermore, KOOSglobal may allow information technology personnel to incorporate a single PRO platform within a practice’s electronic medical records system. If found to be a valid instrument with other common knee diagnoses, all knee patients could complete the 11 KOOSglobal questions with three potential scores being created (KOOS,JR, KOOS Quality of Life, and KOOSglobal). As pay-for-performance reporting mandates are implemented, the selection of which score to calculate and report for a given patient would not fall on the surgeon or orthopedic staff, but could be programmatically tied to procedure or diagnosis codes. This could allow for the same series of 11 questions to be scored differently for an ACL reconstruction (KOOSglobal) and arthroplasty patient (KOOS,JR).
This study was not without limitations. The use of the KOOSglobal has been validated in an ACL patient population and allows for the calculation of the KOOS,JR, which has been validated in the TKA population. While these validation studies include the “anchors” on the continuum of post-traumatic osteoarthritis (i.e. ACL injury and TKA), future studies are necessary to determine if the current results are generalizable to those with mild to moderate knee osteoarthritis or other common knee diagnoses.
Conclusions
By creating an aggregate score from the KOOS,JR and KOOS Quality of Life questions, the KOOSglobal offers a responsive PRO tool after ACL reconstruction that converges with the information captured with the IKDC. Also, by offering the ability to calculate multiple scores from a single questionnaire, the 11-item KOOSglobal may potentially provide the orthopedic community a single PRO platform to be used across knee-related subspecialties.
Supplementary Material
What is known about the subject:
Marked ceiling effects have been noted in some of the KOOS subscales following ACL reconstruction.
What this study adds to the existing knowledge:
By creating an aggregate score from the KOOS,JR and the 4 KOOS Quality of Life questions, the KOOSglobal offers a responsive PRO tool after ACL reconstruction that converges with the information captured with the IKDC.
Contributor Information
Cale A. Jacobs, Department of Orthopedic Surgery, University of Kentucky, Lexington, Kentucky, USA.
Michael R. Peabody, American Board of Family Medicine, Lexington, Kentucky, USA.
Christian Lattermann, Department of Orthopedic Surgery, Brigham & Women's Hospital, Harvard Medical School, Chestnut Hill, Massachusetts, USA.
Jose F. Vega, Cleveland Clinic Sports Health Center, Garfield Heights, Ohio, USA.
Laura J. Huston, Vanderbilt Orthopaedic Institute, Nashville, Tennessee, USA.
Kurt P. Spindler, Cleveland Clinic Sports Health Center, Garfield Heights, Ohio, USA.
References
- 1.Andrich D Measurement criteria for choosing among models for graded responses In: von Eye A, Clogg CC, eds. Analysis of Categorical Variables in Developmental Research. Orlando, FL: Acadmic Press; 1996:3–35. [Google Scholar]
- 2.Anthony CA, Lawler EA, Ward CM, Lin IC, Shah AS. Use of an automated mobile phone messaging robot in postoperative patient monitoring. Telemed J E Health. 2017;Epub ahead of print(doi: 10.1089/tmj.2017.0055). [DOI] [PubMed] [Google Scholar]
- 3.Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB. Validation of the Knee Injury and Osteoarthritis Outcome Score (KOOS) for the treatment of focal cartilage lesions. Osteoarthritis Cartilage. 2009;17(11):1434–1439. [DOI] [PubMed] [Google Scholar]
- 4.Blocker O, Bullock A, Morgan-Jones R, Ghandour A, Richardson J. Using text messaging in long-term arthroplasty follow-up: a pilot study. JMIR Res Protoc. 2017;6(5):e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC.gov. National Hospital Discharge Survey: 2010 table, procedures by selected patient characteristics - number by procedure category and age. Available at: http://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf. Accessed May 6, 2016. [Google Scholar]
- 6.Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967–1976. [DOI] [PubMed] [Google Scholar]
- 7.CMS.org. Centers for Medicare & Medicaid Services. Measure Methodology.
- 8.Cohen J Statistical power analysis for the behavioral sciences. Vol 2nd Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 9.Duncan ST, Jacobs CA, Christensen CP, Nunley RM, Macaulay WB. Is physician quality reporting system worth the cost to report to Center for Medicare and Medicaid Services? J Arthroplasty. 2017;32(4):1055–1057. [DOI] [PubMed] [Google Scholar]
- 10.Faucher M, Poiraudeau S, Lefevre-Colau M, Rannou F, Fermanian J, Revel M. Algo-functional assessment of knee osteoarthritis: comparison of the test-retest reliability and construct validity of the Womac and Lequesne indexes. Osteoarthritis Cartilage. 2002;10:602–610. [DOI] [PubMed] [Google Scholar]
- 11.Golicki D, Niewada M, Karlinska A, et al. Comparing responsiveness of the EQ-5D-5L, EQ-5D-3L, EQ-VAS in stroke patients. Qual Life Res. 2015;24:1555–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries. A review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–1532. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs CA, Peabody MR, Duncan ST, et al. Development of the HOOSglobal to assess patient-reported outcomes in patients undergoing hip preservation procedures. Am J Sports Med. 2018;46(4):940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jevsevar DS, Bozic KJ, Group QODW. Patient Reported Outcome Measures. Available at: http://www.aaos.org/Quality/Performance_Measures/Patient_Reported_Outcome_Measures/?ssopc=1. Accessed 3/6/2017.
- 15.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg (Am). 2007;89-A(4):780–785. [DOI] [PubMed] [Google Scholar]
- 16.Lam ETP, Lam CLK, Fong DYT, Huang WW. Is the SF-12 version 2 health survey a valid and equivalent substitute for the SF-36 version 2 health survey for the Chinese? J Eval Clin Pract. 2013;19:200–208. [DOI] [PubMed] [Google Scholar]
- 17.Liang MH. Longitudinal construct validity: establishment of clinical meaning in patient evaluative instruments. Medical Care. 2000;38:1184–1190. [PubMed] [Google Scholar]
- 18.Liang MH, Larson MG, Cullen KE, Schwartz JA. Comparative measurement efficiency and sensitivity of five health status instruments for arthritis research. Arthritis Rheum. 1985;28(5):542–547. [DOI] [PubMed] [Google Scholar]
- 19.Lim CR, Harris K, Dawson J, Beard D, Fitzpatrick R, Price AJ. Floor and ceiling effects in the OHS: an analysis of the NHS PROMs data set. BMJ Open. 2015;5:e007765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linacre JM. Optimizing rating scale category effectiveness. J Appl Meas. 2002;3(1):85–106. [PubMed] [Google Scholar]
- 21.Lind M, Lund B, Fauno P, Said S, Miller LL, Christiansen SE. Medium to long-term follow-up after ACL revision. Knee Surg Sports Traumatol Arthrosc. 2012;20:166–172. [DOI] [PubMed] [Google Scholar]
- 22.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–1769. [DOI] [PubMed] [Google Scholar]
- 23.Lohmander LS, Roos H. Knee ligament injury, surgery, and osteoarthritis. Truth or consequences? Acta Orthop. 1994;65(6):605–609. [DOI] [PubMed] [Google Scholar]
- 24.Lyman S, Lee Y-Y, Franklin PD, Li W, Cross MB, Padgett DE. Validation of the KOOS, JR: A short-form knee arthroplasty outcomes survey. Clin Orthop Related Res. 2016;epub ahead of print(DOI 10.1007/s11999-016-4719-1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manolarakis GE, Kontodimopoulos N, Sifaki-Pistolla D, Niakas D. Establishing the psychometric properties of the ICOAP questionnaire through intra-articular treatment of osteoarthritic pain: implementation for the Greek version. Arthritis. 2016;Article ID 6201802( 10.1155/2016/6201802). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masters GN. A Rasch Model for partial credit scoring. Psychometrika. 1982;47(2):149–174. [Google Scholar]
- 27.Nilsdotter A-K, Roos EM, Westerlund JP, Roos HP, Lohmander LS. Comparative responsiveness of measures of pain and function after total hip replacement. Arthritis Care & Research. 2001;45:258–262. [DOI] [PubMed] [Google Scholar]
- 28.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]
- 29.Rasch G Probabilistic Models for Some Intelligence and Attainment Tests. Copenhagen, Denmark: Danish Institute for Educational Research; 1960. [Google Scholar]
- 30.Rolstad S, Adler J, Ryden A. Response burden and questionnaire length: Is shorter better? A review and meta-analysis Value in Health. 2011;14:1101–1108. [DOI] [PubMed] [Google Scholar]
- 31.Roos EM. Effectiveness and practice variation of rehabilitation after joint replacement. Curr Op in Rheumatol. 2003;15:160–162. [DOI] [PubMed] [Google Scholar]
- 32.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orhtop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 33.Smith EV. Evidence for the reliability of measures and validity of measure interpretation: A Rasch measurement perspective In: Smith EV, Smith RM, eds. Introduction to Rasch Measurement. Maple Grove, MN: JAM Press; 2004:93–122. [PubMed] [Google Scholar]
- 34.Theiler R, Sangha O, Schaeren S, et al. Superior responsiveness of the pain and function sections of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) as compared to the Lequesne-algofunctional Index in patients with osteoarthritis of the lower extremities. Osteoarthritis Cartilage. 1999;7:515–519. [DOI] [PubMed] [Google Scholar]
- 35.Wright BD. Time 1 to Time 2 (Pre-test to Post-test) comparison: Racking and Stacking. Rasch Measurement Transactions. 1996;10(1):478. [Google Scholar]
- 36.Wright BD. Rack and Stack: Time 1 vs. Time 2 or Pre-Test vs. Post-Test. Rasch Measurement Transactions. 2003;17(1):905–906. [Google Scholar]
- 37.Wright BD, Linacre JM. Reasonable mean square fit values. Rasch Measurement Transactions. 1994;8(3):370. [Google Scholar]
- 38.Wright BD, Masters GN. Rating Scale Analysis. Chicago, IL: MESA Press; 1982. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.