Abstract
Purpose
Alcohol and smoking play an important role in pancreatitis. This review will address the myths and evidences about alcohol and smoking with pancreatitis to help improve the approach of health care professionals when managing of these patients.
Recent Findings
There is a growing recognition that chronic pancreatitis is a multifactorial disease. Eliciting an accurate history of alcohol consumption and smoking from patients, and if necessary, family members, can help determine their contribution to the patient’s disease. In the absence of a convincing history, physicians should be open to consideration of other etiologies. The amount and duration of alcohol consumption is the most important determinant in increasing pancreatitis risk. Alcohol sensitizes the pancreas to other insults or injury and promotes disease progression. Smoking is an independent risk factor or chronic pancreatitis and has synergistic pathogenic effects with alcohol. The natural history of chronic pancreatitis is highly variable. A patient with alcoholic pancreatitis can have symptoms, recurrences or exacerbations from disease-related complications or non-pancreatic causes. Novel strategies are needed to enable patients quit smoking.
Summary
Obtaining accurate history, appropriate evaluation and management can help to achieve meaningful improvement in symptoms in patients with chronic pancreatitis. Abstinence from alcohol and smoking cessation, when applicable, should be recommended in all patients to prevent disease recurrences and progression.
Keywords: Pancreatitis, abstinence, cessation, drinking, risk
Introduction
The relationship between alcohol and pancreatitis is known for over a hundred years. While there was initial skepticism that smoking also contributed to chronic pancreatitis, the association between smoking and pancreatitis is now well-established. Despite these known associations, physician routinely come across patients who do not fit into the “typical clinical profile” of chronic pancreatitis. This review aims to highlight some of the prevailing myths about the association of alcohol and smoking with pancreatitis. We hope to dispel these myths with empiric data, where available, and suggest areas where further research is needed.
MYTH #1: Chronic Pancreatitis patients are all alcoholics.
This concept is the residual effects of the dogma of previous generations when alcohol was the only identifiable risk factor for chronic pancreatitis in the majority of patients. In many medical and surgical subspecialties this misperception prevails, with substantial negative consequences. Preconceived notions can affect a physician or healthcare professionals’ approach and interactions with patients, their ability to consider a thorough work up for other potential etiology or the cause of symptoms, and an opportunity to choose a therapy that may result in meaningful improvement in the condition. It is not uncommon to come across patients who are believed to be underreporting their drinking or are labeled as closet alcoholics.
The proportion of patients in whom alcohol was identified as the primary cause in several recent large cross-sectional studies from the US, Europe and Japan range from 44–68% (Table 1)1–7. In other words, in 32–56% patients, alcohol was not considered to be the major factor for the patient’s disease – of particular importance being that only a minority of all cases among women are explained by alcohol. In developing countries, although alcohol-related pancreatitis appears to be on the rise, the majority of cases are related to idiopathic or genetic causes8–10. Finally, there is growing recognition of pancreatitis as a distinct disease in children, in whom alcohol is rarely a factor in disease causation11, 12.
Table 1:
Alcohol etiology and prevalence of abdominal pain in recent cross-sectional studies from US, Europe and Japan
| Country | Study name | Time period | Sample size | Male (%) | Alcohol etiology (%) | Pain (%) | ||
|---|---|---|---|---|---|---|---|---|
| All | Male | Female | ||||||
| USA | NAPS22, 53 | 2000–2006 | 540 | 53 | 45 | 59 | 28 | 86 |
| USA | NAPS2-CV1, 46 | 2008–2011 | 521 | 55 | 46 | 58 | 30 | 84 |
| Italy | PanCroInAISP4 | 2000–2005 | 892 | 74 | 43 | 55 | 14 | 63 |
| Hungary | HPSG7 | 2012–2014 | 229 | 74 | 62 | N/A | N/A | 68 |
| Belgium | Belgian National Registry3 | 2014–2015 | 809 | 74 | 65 | N/A | N/A | N/A |
| Scandinavia | SBPC6 | As of 12/2016 | 910 | 67 | 59 | N/A | N/A | 69 |
| Japan | National survey5 | 2011 | 1,734 | 68 | 76 | 30 | N/A | N/A |
NAPS2: North American Pancreatitis Study; NAPS2-CV: NAPS2-continuation and validation study; SBPC: Scandinavian Baltic Pancreatic Club; NA – not available
The evolving conceptual framework is that chronic pancreatitis is a multifactorial disease – while alcohol is the most commonly identified risk factor, environmental factors other than alcohol, genetics and other known or yet unknown factors may be important in subsets of patients13.
Reality:
Pancreatitis is a multifactorial disease. Alcohol is the most commonly identified risk factor for chronic pancreatitis, but many cases of chronic pancreatitis may occur independent of any alcohol.
MYTH #2: Alcohol causes pancreatitis.
Interestingly, administration of alcohol alone, irrespective of dosage, is unable to elicit pancreatitis responses in experimental and animal models14. The most commonly used model is hyperstimulation with cholecystokinin or its analogue caerulein, where supraphysiologic doses of these agents are needed to initiate pancreatitis responses. However, in the presence of alcohol, these agents can initiate pancreatitis even with physiologic doses. This observation has led investigators to suggest that heavy alcohol consumption “sensitizes” the pancreas to another injury or insult15–17.
Effects of chronic alcohol consumption on the brainstem result in adaptive responses in the neurohormonal control of pancreatic secretion to maintain normal pancreatic enzyme output despite inhibitory effects of alcohol on neurohormonal reflexes. Sudden withdrawal of alcohol from rodents that have adapted to continuous elevated blood levels of alcohol can lead to sudden release of the inhibitory effects of alcohol on pancreatic secretion resulting in pancreatic hyperstimulation18, which can cause acute pancreatitis. In one well-conducted human epidemiologic study, 69% patients with first-attack of alcoholic pancreatitis were noted to have stopped drinking shortly before developing the first symptom – in 33% between 7–24 hours, and 28% more than 24 hours before the onset of symptoms19. Interestingly, 54% reported that they had stopped continuous drinking before the start of acute abdominal pain.
Alcohol also has effects on the pancreas at many other levels. Some of these include facilitation of pancreatic injury through signaling pathways, non-oxidative metabolism to form fatty acid ethyl esters which could lead to mitochondrial toxicity, activation of pancreatic stellate cells directly or through other mechanisms,the way pancreas responds to stress, and how alcohol alters the immune response to injury. These effects explain greater severity of alcohol-related acute pancreatitis, and its progression to chronic pancreatitis. A detailed discussion of these is beyond the scope of this article, and the reader is referred to excellent reviews on mechanisms of alcohol-related pancreatic disease and animal models of pancreatitis14, 20, 21.
Reality:
Alcohol does not cause pancreatitis directly. Heavy alcohol consumption has a variety of effect on the pancreas, brain and the immune system. These effects sensitize the pancreas to injury and promote disease progression after initiation of pancreatic injury.
MYTH #3: Most people who drink heavily develop pancreatitis.
The absolute risk of pancreatitis with alcohol consumption was evaluated in two studies using different study designs. In a study of 1,409 veterans who received care in the Veterans Administration System and attended an outpatient detoxification clinic for alcoholism, prevalence of pancreatitis diagnosis was used as a surrogate for lifetime risk. In these veterans, the prevalence of pancreatitis diagnosis at any time during their care was 5.9% for any, 4.7% for acute, and 3.0% for chronic pancreatitis. This prevalence was ~6 folds greater when compared with the prevalence of any (0.98%), acute (0.76%) and chronic (0.41%) pancreatitis diagnosis in 59,378 veterans treated in the same healthcare system who did not receive an alcoholism diagnosis22.
In a cohort study of 17,905 subjects who enrolled in the Copenhagen City Heart Study in Denmark from 1976 to 2007, during a mean of 20.1 years of follow-up, the overall risk of any pancreatitis was noted to be 1.3%23. Participants completed a detailed questionnaire at the time of ascertainment which included information about their drinking and smoking habits. The risk of pancreatitis increased with the amount of alcohol consumption – the absolute risk in subjects who reported drinking ≥5 drinks/day was ~2.9%, which was ~3 folds greater when compared to abstainers.
Two meta analyses have evaluated the risk of pancreatitis with the amount of alcohol consumption24, 25. Although a clear association is noted with higher amount of consumption, i.e. ≥4–5 drinks per day, the role of lower amounts of alcohol consumption is less clear and needs further study. One likely reason is an overall small increase in absolute risk of disease at lower levels of consumption, thereby limiting power to detect statistical significance. Moreover, in addition to the amount and intensity of drinking, i.e. drinks on a drinking day, pattern of consumption, e.g. regular vs. binge drinking may also be important determinants in increasing the risk. We consider regular drinking at lower levels to be a co-factor in disease development and progression.
A recent provocative epidemiologic study, supported by experimental data, reported that smaller amounts of alcohol may even be protective for incident acute pancreatitis26. Whether there truly is a safe limit for alcohol consumption with regard to incident pancreatitis or in patients who have suffered an episode of mild non-alcohol related acute pancreatitis needs further study. Individuals who have had an episode of alcohol-related pancreatitis, and those with recurrent acute or chronic pancreatitis from any cause should be cautioned to avoid alcohol consumption, as even smaller amounts of consumption result in disease progression27–29.
Since only a small fraction of heavy drinkers ever develop pancreatitis, there must be other co-factors that result in an individual’s susceptibility to pancreatitis. These likely vary between individuals, and include known factors, such as smoking30, hypertriglyceridemia31, genetic polymorphisms (e.g. CLDN2, alcohol or aldehyde dehydrogenase)32–34 or yet unknown factors. This concept is reinforced by findings that lifetime drinking habits and cumulative consumption do not differ significantly between alcoholics who do and do not develop pancreatitis35.
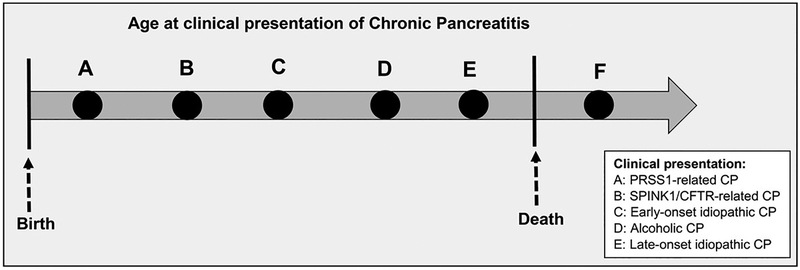
How does environmental and genetic factors impact the clinical presentation and phenotype of pancreatitis? We agree with the hypothesis proposed by DiMagno et al that alcohol and tobacco affect the expression of disease, and that genetic susceptibility underlies the development of chronic pancreatitis36. An earlier age of onset of alcoholic pancreatitis than late-onset idiopathic chronic pancreatitis, and acceleration of disease course by alcohol and smoking demonstrated by them and others provides empiric data to support this hypothesis36–39. The age at presentation for genetic, early-onset and late-onset idiopathic chronic pancreatitis reflect the strength of underlying genetic influence, in that mutations with stronger effects result in an earlier age at the onset of symptoms/diagnosis (e.g. PRSS1, SPINK1, CFTR)40 (Figure 1). Presence of environmental influences in these subjects will further reduce the age of presentation and accelerate disease course.
Figure 1:
Impact of alcohol, smoking and genetic factors on the clinical presentation and phenotype of pancreatitis.
The arrow represents time in years from birth and extends beyond death to represent a hypothetical scenario (F) for an inherent risk to develop chronic pancreatitis in all individuals. In subjects with no alcohol use (but may be presence of other environmental factors such as smoking and/or weak genetic effects), pancreatitis can manifest during lifetime which would otherwise not have manifested (E – late-onset idiopathic chronic pancreatitis). Exposure to alcohol (usually in combination of smoking) results in acceleration of late-onset idiopathic disease by several years (D – alcoholic chronic pancreatitis). Presence of genetic factors result in acceleration of disease expression depending on the strength of influence (e.g. C – early-onset idiopathic chronic pancreatitis; B – SPINK1 or CFTR gene mutations; A – PRSS1 gene mutations). Environmental influences in patients with more penetrant genetic factors will further impact disease expression (concepts elaborated from Ref. 36).
Reality:
Clinical pancreatitis develops in ~5% of individuals who drink heavily. Consumption of ≥4–5 drinks per day increases the risk of developing pancreatitis. Regular consumption of alcohol at lower levels is likely a co-factor in disease development. Safe limit of alcohol consumption for incident pancreatitis is currently not established. Alcohol consumption affects the clinical presentation and course of disease.
MYTH #4: The risk of pancreatitis is lower with beer (or wine) drinking.
Studies have used different designs to assess the impact of beverage type on the risk of pancreatitis. In a cohort study of ~85,000 Swedish subjects followed for a median of 10 years, Sadr-Azodi et al reported that, when compared with wine or beer, the risk of incident acute pancreatitis was 1.52-fold greater for each increment of 5 drinks of spirits consumed on a single occasion41. In another cohort study from Denmark, drinking 14 or more beers per week increased the risk of pancreatitis by 2-folds, but no association was noted with wine or spirits23. Similarly, case-control studies have also shown discordant results42, 43. In a Japanese study evaluating lifetime drinking habits among patients with alcoholic acute and chronic pancreatitis, beer drinking was less frequent among men when compared with women, and in patients with chronic pancreatitis when compared with those who had acute pancreatitis29. Epidemiology studies focusing on alcohol may also be confounded by diet, since in at least one study people who drank wine had a significantly healthier diet than people who drank beer44. Definitive studies on the relationship between beverage type with the risk of pancreatitis are awaited.
Alcohol consumption is universal and the type of alcoholic beverage consumed varies between and within geographic regions. However, occurrence of pancreatitis is not limited by geography. While beverage type may influence risk, we believe that the amount and duration of alcohol consumption is the most important determinant for the risk of pancreatitis.
Reality:
The role of beverage type on the risk of pancreatitis needs further study. The amount of alcohol consumed likely has a far greater impact in the risk of pancreatitis than beverage type.
MYTH #5: Patients with alcoholic acute pancreatitis either have or will progress to chronic pancreatitis.
Historically, it was believed that acute pancreatitis in alcoholics was the first manifestation of pre-existing alcoholic chronic pancreatitis and that progression from acute pancreatitis to chronic pancreatitis was extremely rare45. In 1999 the Sentinel Acute Pancreatitis Event (SAPE) hypothesis was proposed as an alternative, suggesting that acute pancreatitis was an important starting point in the process leading to chronic pancreatitis46. Since then several studies followed the natural course after the first attack of acute pancreatitis and observed that a subset of patients clearly develop recurrences or transition to clinical chronic pancreatitis, and this risk is greater in patients with alcohol etiology39. Taking one representative population-based study from Germany as an example, the risk of a subsequent attack after an attack of acute alcoholic pancreatitis was 33%, and the risk of progression to chronic pancreatitis after one recurrence was 42%47. Equally important is to recognize that the risk of disease progression is directly linked to continuation of alcohol consumption after the initial presentation27, 28.
Reality:
Progression to chronic pancreatitis after an episode of alcoholic pancreatitis occurs in a subset of patients. The risk of disease progression is directly linked to continuation of alcohol consumption (and smoking).
MYTH #6: A patient with alcoholic pancreatitis is unlikely to give up drinking.
Although physicians and other health care professionals regularly counsel for abstinence from alcohol, they often feel that patients will not follow their advice and continue to drink. However, in published studies, a significant fraction of patients are noted to have stopped or significantly reduced their drinking during follow up27, 48. The impact of continuing alcohol consumption on the natural history should be discussed with patients. It is important to offer structured services for counseling49 and other professional services for alcohol rehabilitation.
Reality:
Patients with alcoholic pancreatitis often stop or reduce their drinking, which is associated with a reduction in symptoms and disease progression.
MYTH#7. Most patients with chronic pancreatitis have chronic pain and are narcotic seeking.
The natural history of chronic pancreatitis is highly variable. Age at presentation or diagnosis, sex, etiology, genetic factors, and integrity of the pancreatic duct are important determinants of the natural history of disease. Patients may have episode(s) of acute pancreatitis interspersed with variable periods of pain or pain free intervals. The severity and temporal nature of pain can also be highly variable. Pain symptoms and acute pancreatitis attack(s) could be related to treatable causes, such as pancreatic ductal stricture and/or stones, local complications, etc. that can be addressed by available therapies. Therefore, an understanding of the natural history of disease is critical to making treatment decisions. It is also important to recognize that morphological findings may not always correlate with the presence, severity of temporal nature of pain50.
In recent cross-sectional studies, the proportion of patients who reported having pain ranges from 63 to 86%, suggesting that a subset of patients were pain free at the time of assessment2, 4, 6, 7, 50. Variability of pain experience was captured in a large multicenter US study of >500 patients – in the year preceding enrollment, 16% patients reported no pain, 53% reported constant and 32% intermittent pain; pain was mild-moderate in 18% and severe 67% patients. Narcotics was used intermittently by 23% and constantly by 36%. Interestingly, the proportion of patients treated with narcotics is much lower in Europe (stronger opioids used in 31%)6.
Reality:
Understanding the natural history can help in making management decisions (also see Myth #8).
MYTH #8: Pain, disease flares and hospitalizations in patients with alcoholic pancreatitis are always related to ongoing alcohol consumption.
A patient with established alcoholic pancreatitis can be symptomatic due to disease-related manifestations independent of alcohol consumption. In addition to counseling for behavior modification, evaluation and addressing potentially treatable causes should be considered, especially in a patient who reports significant reduction or abstinence from alcohol consumption.
Development of obstructive disease related to pancreatic ductal structure and/or stones, duct blowout due to obstructive disease, ductal disruption, inflammatory mass in the head of the pancreas, disconnected duct after an episode of acute pancreatitis, groove pancreatitis or nonpancreatic diseases such as symptomatic gallstone disease, peptic ulcer disease, gastroparesis and small bowel bacterial overgrowth are examples of conditions where appropriate management can lead to prolonged symptomatic improvement and quality of life.
Reality:
A patient with alcoholic pancreatitis can have symptoms from disease-related manifestations that may be independent of alcohol consumption or have non-pancreatic cause for symptoms. Appropriate evaluation and management may lead to meaningful improvement in symptoms and quality of life.
MYTH #9: Smoking has no relationship with pancreatitis.
Since patients with alcohol also have a high prevalence of tobacco smoking, for years, it used to be believed that the relationship between smoking with pancreatitis is spurious because one could not separate between the effects of alcohol from smoking. However, several well-conducted studies have confirmed conclusively that smoking is an independent risk factor for the risk of acute and chronic pancreatitis, as well as for disease progression39, 51. The risk of pancreatitis is greater with current smoking and the amount of smoking. While studies have primarily evaluated the relationship with cigarette smoking, it is reasonable to assume that the effects of smoking apply to all forms of tobacco exposure.
Reality
Smoking is a dose-dependent risk factor for susceptibility and progression of pancreatitis
MYTH #10: Counseling for smoking cessation in patients with pancreatitis can be effective.
Increasing awareness can improve physician recognition of smoking as a risk factor for pancreatitis. This will hopefully translate into increased counseling and facilitating enrollment of patients into smoking cessation programs. However, a recent small study found that such programs may have suboptimal results in terms of achieving smoking cessation52 highlighting the needs for novel strategies to achieve this goal.
Reality
Counseling for smoking cessation may have limited success in helping patients to quit. Innovative strategies are needed to promote smoking cessation in patient with pancreatitis.
Conclusion
Alcohol and smoking play an important role in increasing the risk as well as progression of pancreatitis. Eliciting an accurate history from patients, and if necessary, family members, can help to determine their contribution to the patient’s disease. In the absence of a convincing history, physicians should be open to consideration of other etiologies. A patient with alcoholic pancreatitis can have symptoms, recurrences or exacerbations from disease-related complications or non-pancreatic causes. Appropriate evaluation and management often helps to achieve a durable and meaningful improvement in symptoms. In addition to abstinence from alcohol, smoking cessation, when applicable, should be recommended in all patients to prevent disease recurrences and progression. Novel strategies are needed to enable patients quit smoking.
Keypoints.
Chronic Pancreatitis is a multifactorial disease. The natural course of chronic pancreatitis is highly variable.
Alcohol and smoking increase the risk and progression of pancreatitis. The amount and duration of alcohol consumption is the most important factor in increasing the risk of pancreatitis. Clinical pancreatitis develops in ~5% individual who drink heavily.
Alcohol sensitizes the pancreas to other insults or injury.
Pain, disease flares and hospitalizations may be disease-related manifestations independent of alcohol consumption or from non-pancreatic causes
Novel strategies are needed to enable patients quit smoking.
Acknowledgements
Dr. Yadav is supported by the National Institute of Health under award number - U01 DK108306. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors thank David C. Whitcomb, MD PhD for critical review of the manuscript and helpful comments.
References
- 1. *.Conwell DL, Banks PA, Sandhu BS, et al. Validation of Demographics, Etiology, and Risk Factors for Chronic Pancreatitis in the USA: A Report of the North American Pancreas Study (NAPS) Group. Dig Dis Sci 2017;62:2133–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]; This cross-sectional study from the NAPS2 cohort validated the demographic and etiologic distribution of patients with chronic pancreatitis reported in the original NAPS2 study.
- 2.Cote GA, Yadav D, Slivka A, et al. Alcohol and smoking as risk factors in an epidemiology study of patients with chronic pancreatitis. Clin Gastroenterol Hepatol 2011;9:266–73; quiz e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. *.Fernandez M, Arvanitakis M, Musala C, et al. The Belgian national registry on chronic pancreatitis: A prospective multi-centre study covering more than 800 patients in one year. Pancreatology 2017;17:572–579. [DOI] [PubMed] [Google Scholar]
- 4.Frulloni L, Gabbrielli A, Pezzilli R, et al. Chronic pancreatitis: report from a multicenter Italian survey (PanCroInfAISP) on 893 patients. Dig Liver Dis 2009;41:311–7. [DOI] [PubMed] [Google Scholar]
- 5.Hirota M, Shimosegawa T, Masamune A, et al. The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology 2014;14:490–6. [DOI] [PubMed] [Google Scholar]
- 6. *.Olesen SS, Poulsen JL, Drewes AM, et al. The Scandinavian baltic pancreatic club (SBPC) database: design, rationale and characterisation of the study cohort. Scand J Gastroenterol 2017;52:909–915. [DOI] [PubMed] [Google Scholar]; Ref 3 and 6 - Two recent cross-sectional studies from Europe describing the clinical profile and management of patients with chronic pancreatitis.
- 7.Szucs A, Marjai T, Szentesi A, et al. Chronic pancreatitis: Multicentre prospective data collection and analysis by the Hungarian Pancreatic Study Group. PLoS One 2017;12:e0171420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giri AK, Midha S, Banerjee P, et al. Common Variants in CLDN2 and MORC4 Genes Confer Disease Susceptibility in Patients with Chronic Pancreatitis. PLoS One 2016;11:e0147345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan J, Xin L, Wang D, et al. Risk Factors for Diabetes Mellitus in Chronic Pancreatitis: A Cohort of 2011 Patients. Medicine (Baltimore) 2016;95:e3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garg PK, Narayana D. Changing phenotype and disease behaviour of chronic pancreatitis in India: evidence for gene-environment interactions. Glob Health Epidemiol Genom 2016;1:e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S, Ooi CY, Werlin S, et al. Risk Factors Associated With Pediatric Acute Recurrent and Chronic Pancreatitis: Lessons From INSPPIRE.JAMA Pediatr 2016;170:562–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. **.Sellers ZM, MacIsaac D, Yu H et al. Nationwide Trends in Acute and Chronic Pancreatitis Among Privately Insured Children and Non-Elderly Adults in the United States, 2007–2014. Gastroenterology 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study used health-claims data from commercially insured population to determine incidence of acute and chronic pancteatitis and prevalence of chronic pancreatitis in children and adults in the United States.
- 13. **.Whitcomb DC, Frulloni L, Garg P et al. Chronic pancreatitis: An international draft consensus proposal for a new mechanistic definition. Pancreatology 2016;16:218–24. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper provides the background and rationale for a new mechanistic definition of chronic pancreatitis, and a framework to use for translational and longitudinal studies on chronic pancreatitis.
- 14. **.Setiawan VW, Monroe K, Lugea A et al. Uniting Epidemiology and Experimental Disease Models for Alcohol-Related Pancreatic Disease. Alcohol Res 2017;38:173–182. [PMC free article] [PubMed] [Google Scholar]; This is a concise yet thorough review on the mechanisms of alcohol-related pancreatic diseases, specifically acute and chronic pancreatitis.
- 15.Katz M, Carangelo R, Miller LJ, et al. Effect of ethanol on cholecystokinin-stimulated zymogen conversion in pancreatic acinar cells. Am J Physiol 1996;270:G171–5. [DOI] [PubMed] [Google Scholar]
- 16.Lu Z, Karne S, Kolodecik T, et al. Alcohols enhance caerulein-induced zymogen activation in pancreatic acinar cells. Am J Physiol Gastrointest Liver Physiol 2002;282:G501–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandol SJ, Periskic S, Gukovsky I, et al. Ethanol diet increases the sensitivity of rats to pancreatitis induced by cholecystokinin octapeptide. Gastroenterology 1999;117:706–16. [DOI] [PubMed] [Google Scholar]
- 18.Deng X, Wood PG, Eagon PK, et al. Chronic alcohol-induced alterations in the pancreatic secretory control mechanisms. Dig Dis Sci 2004;49:805–19. [DOI] [PubMed] [Google Scholar]
- 19.Nordback I, Pelli H, Lappalainen-Lehto R, et al. Is it long-term continuous drinking or the post-drinking withdrawal period that triggers the first acute alcoholic pancreatitis? Scand J Gastroenterol 2005;40:1235–9. [DOI] [PubMed] [Google Scholar]
- 20.Lerch MM, Gorelick FS. Models of acute and chronic pancreatitis. Gastroenterology 2013;144:1180–93. [DOI] [PubMed] [Google Scholar]
- 21.Yadav D, Whitcomb DC. The role of alcohol and smoking in pancreatitis. Nature reviews. Gastroenterology & hepatology 2010;7:131–45. [DOI] [PubMed] [Google Scholar]
- 22.Yadav D, Eigenbrodt ML, Briggs MJ, et al. Pancreatitis: prevalence and risk factors among male veterans in a detoxification program. Pancreas 2007;34:390–8. [DOI] [PubMed] [Google Scholar]
- 23.Kristiansen L, Gronbaek M, Becker U, et al. Risk of pancreatitis according to alcohol drinking habits: a population-based cohort study. Am J Epidemiol 2008;168:932–7. [DOI] [PubMed] [Google Scholar]
- 24.Irving HM, Samokhvalov AV, Rehm J. Alcohol as a risk factor for pancreatitis. A systematic review and meta-analysis. JOP 2009;10:387–92. [PMC free article] [PubMed] [Google Scholar]
- 25.Samokhvalov AV, Rehm J, Roerecke M. Alcohol Consumption as a Risk Factor for Acute and Chronic Pancreatitis: A Systematic Review and a Series of Meta-analyses. EBioMedicine 2015;2:1996–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Setiawan VW, Pandol SJ, Porcel J, et al. Prospective Study of Alcohol Drinking, Smoking, and Pancreatitis: The Multiethnic Cohort. Pancreas 2016;45:819–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takeyama Y Long-term prognosis of acute pancreatitis in Japan. Clin Gastroenterol Hepatol 2009;7:S15–7. [DOI] [PubMed] [Google Scholar]
- 28.Nikkola J, Raty S, Laukkarinen J, et al. Abstinence after first acute alcohol-associated pancreatitis protects against recurrent pancreatitis and minimizes the risk of pancreatic dysfunction. Alcohol Alcohol 2013;48:483–6. [DOI] [PubMed] [Google Scholar]
- 29.Masamune A, Kume K, Shimosegawa T. Sex and age differences in alcoholic pancreatitis in Japan: a multicenter nationwide survey. Pancreas 2013;42:578–83. [DOI] [PubMed] [Google Scholar]
- 30.Greer JB, Thrower E, Yadav D. Epidemiologic and Mechanistic Associations Between Smoking and Pancreatitis. Curr Treat Options Gastroenterol 2015;13:332–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. *.Vipperla K, Somerville C, Furlan A et al. Clinical Profile and Natural Course in a Large Cohort of Patients With Hypertriglyceridemia and Pancreatitis. J Clin Gastroenterol 2017;51:77–85. [DOI] [PubMed] [Google Scholar]; In this study, the natural course of patients with hypertriglyceridemia and pancreatitis is described. Of specific relevance is that a subset of patients also had chronic pancreatitis, and that the course of alcoholic pancreatitis can be modified by hypertriglyceridemia.
- 32.Whitcomb DC, LaRusch J, Krasinskas AM, et al. Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis. Nature genetics 2012;44:1349–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhong Y, Cao J, Zou R, et al. Genetic polymorphisms in alcohol dehydrogenase, aldehyde dehydrogenase and alcoholic chronic pancreatitis susceptibility: a meta-analysis. Gastroenterol Hepatol 2015;38:417–25. [DOI] [PubMed] [Google Scholar]
- 34.Rosendahl J, Kirsten H, Hegyi E, et al. Genome-wide association study identifies inversion in the CTRB1-CTRB2 locus to modify risk for alcoholic and non-alcoholic chronic pancreatitis. Gut 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. *.Juliusson SJ, Nielsen JK, Runarsdottir V et al. Lifetime alcohol intake and pattern of alcohol consumption in patients with alcohol-induced pancreatitis in comparison with patients with alcohol use disorder. Scand J Gastroenterol 2018:1–7. [DOI] [PubMed] [Google Scholar]; This is one of the few studies to describe the lifetime drinking history in patients with alcoholic pancreatitis, and compares this to subjects with other alcohol use disorders.
- 36.Lankisch MR, Imoto M, Layer P, et al. The effect of small amounts of alcohol on the clinical course of chronic pancreatitis. Mayo Clin Proc 2001;76:242–51. [DOI] [PubMed] [Google Scholar]
- 37.Imoto M, DiMagno EP. Cigarette smoking increases the risk of pancreatic calcification in late-onset but not early-onset idiopathic chronic pancreatitis. Pancreas 2000;21:115–9. [DOI] [PubMed] [Google Scholar]
- 38.Maisonneuve P, Lowenfels AB, Mullhaupt B, et al. Cigarette smoking accelerates progression of alcoholic chronic pancreatitis. Gut 2005;54:510–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sankaran SJ, Xiao AY, Wu LM, et al. Frequency of progression from acute to chronic pancreatitis and risk factors: a meta-analysis. Gastroenterology 2015;149:1490–1500 e1. [DOI] [PubMed] [Google Scholar]
- 40.Whitcomb DC. Genetic risk factors for pancreatic disorders. Gastroenterology 2013;144:1292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadr Azodi O, Orsini N, Andren-Sandberg A, et al. Effect of type of alcoholic beverage in causing acute pancreatitis. Br J Surg 2011;98:1609–16. [DOI] [PubMed] [Google Scholar]
- 42.Canha MI, Oliveiros B, Franco C, et al. The lifestyle influence on alcoholic pancreatitis versus alcoholic liver disease: a case-control study. Scand J Gastroenterol 2017;52:1278–1285. [DOI] [PubMed] [Google Scholar]
- 43.Nakamura Y, Ishikawa A, Sekiguchi S, et al. Spirits and gastrectomy increase risk for chronic pancreatitis in Japanese male alcoholics. Pancreas 2003;26:e27–31. [DOI] [PubMed] [Google Scholar]
- 44.Johansen D, Friis K, Skovenborg E, et al. Food buying habits of people who buy wine or beer: cross sectional study. BMJ 2006;332:519–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singer MV, Gyr K, Sarles H. Revised classification of pancreatitis. Report of the Second International Symposium on the Classification of Pancreatitis in Marseille, France, March 28–30, 1984. Gastroenterology 1985;89:683–5. [PubMed] [Google Scholar]
- 46.Whitcomb DC. Hereditary pancreatitis: new insights into acute and chronic pancreatitis. Gut 1999;45:317–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lankisch PG, Breuer N, Bruns A, et al. Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol 2009;104:2797–805; quiz 2806. [DOI] [PubMed] [Google Scholar]
- 48.Ahmed Ali U, Issa Y, Hagenaars JC, et al. Risk of Recurrent Pancreatitis and Progression to Chronic Pancreatitis After a First Episode of Acute Pancreatitis. Clin Gastroenterol Hepatol 2016;14:738–46. [DOI] [PubMed] [Google Scholar]
- 49.Nordback I, Pelli H, Lappalainen-Lehto R, et al. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology 2009;136:848–55. [DOI] [PubMed] [Google Scholar]
- 50.Wilcox CM, Yadav D, Ye T, et al. Chronic pancreatitis pain pattern and severity are independent of abdominal imaging findings. Clin Gastroenterol Hepatol 2015;13:552–60; quiz e28–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ye X, Lu G, Huai J, et al. Impact of smoking on the risk of pancreatitis: a systematic review and meta-analysis. PLoS One 2015;10:e0124075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Han S, Kheder J, Bocelli L, et al. Smoking Cessation in a Chronic Pancreatitis Population. Pancreas 2016;45:1303–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mullady DK, Yadav D, Amann ST, et al. Type of pain, pain-associated complications, quality of life, disability and resource utilisation in chronic pancreatitis: a prospective cohort study. Gut 2011;60:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]