ABSTRACT
Background
There are limited data regarding the impact of atherosclerosis detection by carotid ultrasound (CUS) on physician prevention efforts and risk‐factor management for cardiovascular disease.
Hypothesis
Atherosclerosis detection by CUS in asymptomatic hypertensive patients would lead to physician prevention efforts, including target low‐density lipoprotein cholesterol (LDL‐C) level and prescription. Also, it may improve risk‐factor management.
Methods
A total of 347 asymptomatic hypertensive subjects (age 61 ± 8 years, 189 men) were prospectively recruited from 22 hospitals. Prior to CUS, physicians were surveyed regarding target LDL‐C level. After CUS, patients were classified into positive CUS (n = 182) and negative CUS (n = 165) groups based on CUS results. Physicians were resurveyed to assess whether the initial target LDL‐C goals were changed. At 6 months, cardiovascular risk‐factor modification status was reassessed.
Results
The proportion of lowered target LDL‐C levels was significantly larger in the positive CUS group than in the negative CUS group (52% vs 23%, P < 0.001). These results were observed even in subjects who had low and moderate risk according to National Cholesterol Education Program–Adult Treatment Panel III guidelines. Lipid‐lowering agents were similarly added or switched to another class in both groups (7% in the positive CUS group vs 11% in the negative CUS group, P = 0.153). LDL‐C was significantly decreased in the positive CUS group (Δ = −24 ± 38 mg/dL, P < 0.001), whereas it was not significantly decreased in the negative CUS group (Δ = −6 ± 31 mg/dL, P = 0.105).
Conclusions
Atherosclerosis detection by CUS lowered physicians' target LDL‐C level and improved cardiovascular risk management in terms of LDL‐C reduction.
Introduction
Atherosclerosis detection by carotid ultrasound (CUS) is widely used because of its lack of radiation exposure, relatively low cost, and ability to detect early‐stage atherosclerosis. Also, the association between carotid intima‐media thickness (cIMT) and cardiovascular disease (CVD) is well established.1, 2 However, there are limited data regarding the impact of atherosclerosis detection by CUS on physician and patient prevention efforts. Some studies suggested that screening for atherosclerosis and knowing the results altered the physician treatment plan.3, 4, 5 In addition, it might help motivate patients to modify their health behaviors, such as adherence to medications and lifestyle changes, and increase their perception of cardiovascular risk.6, 7, 8 In contrast to these studies, others assessing the impact of atherosclerosis screening reported that it was not associated with patient lifestyle modifications.3, 9 Furthermore, the role of screening for atherosclerosis in the clinical setting is still controversial, and it is debated whether imaging should be considered only in certain groups of subjects or extended to healthy adults, leading to controversial guidelines.10, 11, 12
However, recent studies have shown some limitations with risk stratification according to traditional methods. When we previously assessed the cardiovascular risk factors solely according to the Third Report of the National Cholesterol Education Program–Adult Treatment Panel III (NCEP‐ATP III) guidelines, two‐thirds of acute myocardial infarction patients were not qualifying for drug therapy.13 Also, other studies showed that nearly 40% of asymptomatic subjects with low risk according to the Framingham Risk Score (FRS) had abnormal CUS findings, and they were associated with increased risk for cardiovascular events.14 Similarly, cIMT and plaque assessment revised the traditional FRS in asymptomatic patients without CVD.15
Thus, this prospective multicenter observational study was designed to examine the hypothesis that atherosclerosis detection by CUS in asymptomatic hypertensive patients would lead to physician prevention efforts including target low‐density lipoprotein cholesterol (LDL‐C) level and prescription. Also, we examined whether atherosclerosis detection by CUS leads to improved risk‐factor management.
Methods
Subjects
Study participants consisted of 347 subjects who were recruited from 22 hospitals in Korea between January 2010 and May 2011. Included were men age 45 to 75 years and women age 55 to 75 years with hypertension (systolic blood pressure [SBP] ≥140 mm Hg or taking antihypertensive medication). Patients with previously documented coronary artery disease (CAD), cerebrovascular disease, peripheral arterial disease, or heart failure with symptoms were excluded. The study protocols were approved by the institutional review board at each participating institution, and written informed consent was obtained from all patients before recruitment.
Study Protocol
Potential patients were screened for the study during routine office visits and underwent routine procedures such as history‐taking, physical examination, and laboratory tests. Ten‐year risk for CAD was calculated by the FRS and NCEP‐ATP III risk category.16, 17 After routine procedures, we surveyed physicians regarding target LDL‐C for their patients. In addition, medications that patients were taking, including antihypertensive, lipid‐lowering, and antiplatelet agents, were recorded on the case report form.
After the survey was completed, CUS examination was performed to measure cIMT and to identify carotid plaques. Based on CUS findings, patients were classified into either a positive CUS group or a negative CUS group. After the CUS examination, physicians were resurveyed as to whether they changed target LDL‐C goals according to classified groups. After that, patients were informed of the test results and their physician's recommendations. Patients were educated that there was a strong association between carotid artery disease and CVD and that their risks for heart attack, stroke, and death were increased if they had plaque or increased cIMT.
A total of 326 patients were then prospectively followed up over 6 months (21 patients were lost to follow‐up). At 6 months after the initial visit, risk‐factor management was re‐evaluated, including body mass index (BMI), waist circumference, SBP, diastolic blood pressure (DBP), and lipid profile.
Carotid Ultrasound Examination
The CUS examination was performed at each participating hospital according to the protocol recommended by the American Society of Echocardiography and the Society of Vascular Medicine.18 The examination included a thorough scan of the extracranial carotid arteries for the presence of carotid plaque, defined as focal wall thickening that was 50% greater than that of the surrounding vessel wall and cIMT >1.5 mm. In the absence of identified plaque, cIMT measurements were made in the distal 1 cm of the far wall of the common carotid artery using the semiautomated border‐detection program. A mean value for cIMT was calculated on the basis of 3 separate measures of IMT on R wave–gated still frames from each of 3 scan planes.18 In our study, patients who had carotid plaque or cIMT >0.9 mm were classified into the positive CUS group, as recommended by the European Society of Hypertension and the European Society of Cardiology.19
Statistical Analysis
Continuous variables are presented as mean ± SD and categorical data are presented as frequencies and group percentages. Patient characteristics were compared between the positive CUS group and negative CUS group using the χ2 test for categorical variables and the Student t test for continuous variables. The paired t test was used to assess changes in risk‐factor management before and 6 months after CUS measurements. These changes were compared between the positive CUS group and negative CUS group using the Student t test.
All analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC). A P value of <0.05 was considered statistically significant.
Results
Baseline Characteristics
Baseline characteristics according to CUS findings are summarized in Table 1. Patients with positive CUS were older and had longer duration of hypertension. Sex, BMI, underlying disease, and blood pressure (BP) were similar. All laboratory findings except triglycerides were similar between the 2 groups. Sixty‐nine percent of the patients were receiving antihypertensive agents and 39% were receiving lipid‐lowering agents. More patients in the positive CUS group were taking antiplatelet agents compared with those in the negative CUS group (40% vs 29%, P = 0.030). The proportion of low risk for coronary heart disease by FRS (FRS <10%) was significantly higher in the negative CUS group compared with the positive CUS group (66% vs 47%, P = 0.005).
Table 1.
Baseline Characteristics According to Results of CUS Examination
| Positive CUS, n = 182 | Negative CUS, n = 165 | P Value | |
|---|---|---|---|
| Age, y | 62 ± 7 | 60 ± 8 | <0.001 |
| Male sex | 103 (56.6) | 86 (52.1) | 0.404 |
| Hypertension duration, y | 5.3 ± 6.0 | 4.0 ± 4.3 | 0.024 |
| BMI, kg/m2 | 25.7 ± 2.9 | 25.1 ± 3.0 | 0.053 |
| Waist circumference, cm | 87.3 ± 9.2 | 86.7 ± 9.8 | 0.630 |
| Family history of premature CAD | 32 (17.6) | 17 (10.4) | 0.055 |
| DM | 28 (15.4) | 17 (10.3) | 0.159 |
| Dyslipidemia | 139 (76.4) | 120 (72.7) | 0.436 |
| Smoking | 0.438 | ||
| Current smoker | 28 (15.4) | 34 (20.6) | |
| Past smoker | 50 (27.5) | 41 (24.9) | |
| Nonsmoker | 104 (57.1) | 90 (54.5) | |
| SBP, mm Hg | 136 ± 18 | 134 ± 13 | 0.376 |
| DBP, mm Hg | 83 ± 12 | 83 ± 10 | 0.627 |
| TG, mg/dL | 138 ± 71 | 156 ± 96 | 0.040 |
| LDL‐C, mg/dL | 115 ± 35 | 110 ± 32 | 0.198 |
| HDL‐C, mg/dL | 51 ± 12 | 52 ± 19 | 0.402 |
| TC, mg/dL | 189 ± 37 | 186 ± 37 | 0.555 |
| FBG, mg/dL | 108 ± 31 | 107 ± 26 | 0.824 |
| HbA1c, % | 6.3 ± 1.2 | 6.1 ± 1.0 | 0.206 |
| Cr, mg/dL | 0.9 ± 0.2 | 0.9 ± 0.2 | 0.677 |
| Medications | |||
| Antihypertensive agents | 120 (65.9) | 119 (72.1) | 0.214 |
| Lipid‐lowering agents | 72 (39.6) | 62 (37.6) | 0.705 |
| Antiplatelet agents | 72 (39.6) | 47 (28.5) | 0.030 |
| FRS | 0.005 | ||
| FRS <10% | 73 (46.5) | 84 (65.6) | |
| FRS 10%–20% | 71 (45.2) | 33 (26.4) | |
| FRS >20% | 13 (8.3) | 8 (6.4) |
Abbreviations: BMI, body mass index; CAD, coronary artery disease; cIMT, carotid intima‐media thickness; Cr, creatinine; CUS, carotid ultrasound; DBP, diastolic blood pressure; DM, diabetes mellitus; FBG, fasting blood glucose; FRS, Framingham Risk Score; HbA1c, glycated hemoglobin; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TG, triglycerides.
Data are presented as means ± SD or as n (%). Subjects with carotid plaque or cIMT >0.9 mm were classified in the positive CUS group as recommended by the European Society of Cardiology.19
Physicians' Changes in Target Low‐Density Lipoprotein Cholesterol and Prescription After CUS Examination
After confirmation of CUS examination results, physicians lowered the target LDL‐C level in 92 patients (52%) in the positive CUS group (Table 2). The most frequent change was from <130 mg/dL to <100 mg/dL. However, physicians lowered the target LDL‐C level only in 39 patients (23%) in the negative CUS group (Table 2). Thus, the proportion of lowered target LDL‐C level was significantly larger in the positive CUS group compared with the negative CUS group (P < 0.001; Figure 1). Of note, these findings even persisted in the low‐risk and moderate‐risk patients according to the NCEP‐ATP III guidelines (Figure 2).
Table 2.
Changes in Target LDL‐C After CUS Examination
| Target LDL‐C After CUS Examination, mg/dL | ||||||||
|---|---|---|---|---|---|---|---|---|
| Positive CUS, n = 182 | Negative CUS, n = 165 | |||||||
| Initial target LDL‐C, mg/dL | <160 | <130 | <100 | <70 | <160 | <130 | <100 | <70 |
| <160 | 13 (7.1)a | 15 (8.2)b | 16 (8.8)b | 0b | 24 (14.5)a | 3 (1.8)b | 0b | 0b |
| <130 | 1 (0.5)c | 45 (24.7)a | 55 (30.2)b | 2 (1.1)b | 3 (1.8)c | 52 (31.5)a | 32 (19.4)b | 1 (0.6)b |
| <100 | 0c | 0c | 25 (13.7)a | 6 (3.3)b | 0c | 1 (0.6)c | 36 (21.8)a | 3 (1.8)b |
| <70 | 0c | 1 (0.5)c | 0c | 3 (1.6)a | 0c | 0c | 0c | 10 (6.1)a |
Abbreviations: CUS, carotid ultrasound; LDL‐C, low‐density lipoprotein cholesterol.
Data are presented as frequencies (% within group).
Subjects whose target LDL‐C remained unchanged after CUS examination.
Subjects whose target LDL‐C decreased after CUS examination.
Subjects whose target LDL‐C increased after CUS examination.
Figure 1.
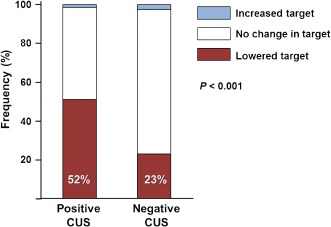
Changes in target LDL‐C after CUS examination. After confirmation of CUS examination results, the proportion of lowered target LDL‐C level was significantly larger in the positive CUS group compared with the negative CUS group (52% vs 23%, P < 0.001). Abbreviations: CUS, carotid ultrasound; LDL‐C, low‐density lipoprotein cholesterol.
Figure 2.
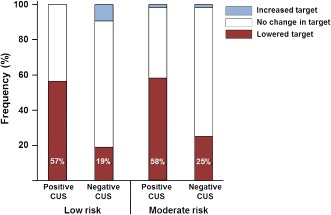
Changes in target LDL‐C after CUS examination stratified by risk according to NCEP‐ATP III guidelines. The proportion of lowered target LDL‐C level was significantly larger in the positive CUS group compared with the negative CUS group, both in the low‐risk and moderate‐risk patients, according to NCEP‐ATP III guidelines. Abbreviations: CUS, carotid ultrasound; LDL‐C, low‐density lipoprotein cholesterol; NCEP‐ATP III, National Cholesterol Education Program–Adult Treatment Program III.
When we evaluated whether the initial target LDL‐C were settled higher or lower than the recommended target level by the NCEP‐ATP III guidelines, 52% of the subjects were initially targeted the same as the recommended goals. However, 28% of subjects were initially targeted higher than the guidelines and 20% were targeted lower than the guidelines. In the initially appropriately targeted group, 55% in the positive CUS group lowered the target LDL‐C after CUS test, although only 37% in the negative CUS group lowered the target LDL‐C (P = 0.018). This finding was consistent in the initially targeted higher group (85% vs 19%, P < 0.001) and the initially targeted lower group (21% vs 6%, P = 0.054).
Regarding the changes in prescription, lipid‐lowering agents were added or switched to another class in 12 (7%) patients in the positive CUS group and in 18 (11%) patients in the negative CUS group, and there were no significant differences between the 2 groups (P = 0.153).
Risk‐Factor Management at 6 Months After Carotid Ultrasound Examination
Changes in risk‐factor management are summarized in Table 3. Body mass index was decreased at 6 months only in the negative CUS group (Δ = −0.1 ± 0.4 kg/m2, P = 0.006). Waist circumference was not changed at 6 months in either group. However, SBP and DBP were significantly decreased regardless of the results of CUS examination, and the degree of change in BP was similar between the 2 groups (P = 0.914 for SBP, P = 0.736 for DBP). Low‐density lipoprotein cholesterol was significantly decreased in the positive CUS group (Δ = −24 ± 38 mg/dL, P < 0.001), whereas it was not significantly decreased in the negative CUS group (Δ = −6 ± 31 mg/dL, P = 0.105), indicating significantly different changes between the 2 groups (P = 0.003). Similarly, total cholesterol was decreased only in the positive CUS group (Δ = −23 ± 46 mg/dL, P < 0.001), but high‐density lipoprotein cholesterol was not changed at the 6‐month follow‐up in either group.
Table 3.
Changes in Risk‐Factor Management at 6 Months After CUS Examination
| Positive CUS | Negative CUS | P Valueb | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Change (Δ) | P Valuea | Baseline | Change (Δ) | P Valuea | ||
| BMI, kg/m2 | 25.7 ± 2.9 | −0.0 ± 1.0 | 0.685 | 25.1 ± 3.0 | −0.1 ± 0.4 | 0.006 | 0.384 |
| Waist circumference, cm | 87.3 ± 9.2 | 0.4 ± 5.2 | 0.361 | 86.7 ± 9.8 | −0.3 ± 5.0 | 0.525 | 0.870 |
| SBP, mm Hg | 136 ± 18 | −6 ± 19 | <0.001 | 134 ± 13 | −6 ± 15 | <0.001 | 0.914 |
| DBP, mm Hg | 83 ± 12 | −5 ± 12 | <0.001 | 83 ± 10 | −4 ± 11 | <0.001 | 0.736 |
| LDL‐C, mg/dL | 115 ± 35 | −24 ± 38 | <0.001 | 110 ± 32 | −6 ± 31 | 0.105 | 0.003 |
| HDL‐C, mg/dL | 51 ± 12 | 1 ± 7 | 0.416 | 52 ± 19 | 2 ± 10 | 0.166 | 0.493 |
| TC, mg/dL | 189 ± 37 | −23 ± 46 | <0.001 | 186 ± 37 | −2 ± 37 | 0.583 | 0.001 |
Abbreviations: BMI, body mass index; CUS, carotid ultrasound; DBP, diastolic blood pressure; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol.
Denotes P values for comparison between baseline and 6‐month follow‐up.
Denotes P values for comparison of changes between the positive CUS and negative CUS groups.
Discussion
The principal findings of the present study are that (1) physicians lowered LDL‐C target levels if atherosclerosis was detected by CUS, and these findings were persistent even in the low‐risk and moderate‐risk patients according to NCEP‐ATP III guidelines; and (2) cardiovascular risk management in terms of LDL‐C reduction improved if atherosclerosis was detected by CUS.
Assessment of subclinical atherosclerosis by CUS is a safe, inexpensive, feasible, and accurate method for detecting early signs of atherosclerosis. Also, the association between cIMT and CVD is well established. A single measurement of cIMT and plaque assessment improves predictions of risk of CVD.1, 2 However, whether atherosclerosis detection by CUS can improve physician behavioral change as well as patient compliance with CVD preventive therapies remains unclear. Previous studies reported that abnormal results of CUS examination were associated with greater initiation of aspirin and lipid‐lowering medications.3, 4 Similar to reports with regard to CUS, abnormal coronary calcium scores also resulted in increased use of aspirin and lipid‐lowering agents.5, 6, 20 However, in the present study, a positive finding of CUS was not associated with the changes in physicians' prescribing patterns. This discrepancy can be attributed to our study subjects. Even though they had hypertension, they were healthy and asymptomatic and had relatively lower LDL‐C compared with those enrolled in the previous studies. Physicians did not change or add medications after CUS examination, but they lowered target LDL‐C after CUS examination if patients had abnormal findings according to CUS. Furthermore, it is noteworthy that these findings were observed even in the patients with low and moderate risk according to NCEP‐ATP III guidelines. Based on our findings, CUS examination could provide possibilities of further risk stratification and physician change in improving CVD risk‐factor management.
It is also interesting that physicians reacted so inconsistently to the positive CUS findings. Because we did not survey the reasons why the physicians did not lower their therapeutic target even after the confirmation of the positive CUS findings specifically, it can be partially attributed to the compliance with the guidelines. Recent guidelines recommended that if patients had documented CVD by noninvasive testing, they should be classified into the very‐high‐risk category for CVD, with a recommended target LDL‐C of <70 mg/dL.21
Our study has strength in that it included longitudinal outcome measures such as 6‐month risk‐factor management. Although several studies demonstrating the utility of screening with noninvasive testing were performed, studies including longitudinal outcomes were limited, and they had relatively short follow‐up periods. As regards patient risk‐factor management and patient behavior change after noninvasive cardiovascular imaging, there are conflicting results. Some studies reported that there was limited evidence that noninvasive cardiovascular imaging altered primary prevention efforts.9, 22, 23, 24 In contrast to these reports, in the Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research (EISNER) trial, compared with no scanning, randomization to coronary artery calcium scanning was associated with superior CAD risk‐factor control.25 Also, determination of coronary artery calcium scores by electron‐beam computed tomography or CAD by coronary computed tomography angiography improved behavioral modification.20, 26 In the present study, pronounced improvement risk‐factor management in terms of LDL‐C reduction in the CUS positive group was observed. Although we did not measure patient effort in CVD risk‐factor management, physicians' behavioral changes combined with patients' behavioral changes might contribute to improvement of risk‐factor management.
Several limitations of the present study need consideration. First, physicians' behavior could have been affected simply because they were being observed. Thus, changes in target LDL‐C level by physicians could have been overestimated. Second, we did not appropriately evaluate patient effort in CVD risk‐factor management, which could be an important contribution to reduction of LDL‐C at 6 months.
Conclusion
Atherosclerosis detection by CUS was associated with lowering physicians' target LDL‐C level and improved cardiovascular risk‐factor management regarding reduction of LDL‐C.
The following investigators also participated in the study: Dong Woon Jeon, National Health Insurance Corporation Ilsan Hospital; Woo‐Shik Kim, Kyunghee University–Industry Cooperation Foundation; Young‐Sup Byun, Inje University Sanggye Paik‐Hospital; Hye‐Sun Seo, Soonchunhyang University Bucheon Hospital; Byung‐Joo Choi, Ajou University Industry–Academic Cooperation Foundation; Sang‐Ho Jo, Hallym University Sacred Heart Hospital; Byung‐Eun Park, Dankook University Hospital; Sahng Lee, Eulji University Hospital; Kyoung Ho Yoon, Won Kwang University Hospital; Hyung‐Seop Kim, Keimyung University Dongsan Hospital; Byung‐Chun Jung, Daegu Fatima Hospital; Sang Gon Lee, Ulsan University Hospital; Han‐Cheol Lee, Pusan National University Hospital.
This research was sponsored by Pfizer Pharmaceuticals Korea Ltd.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Nambi V, Chambless L, Folsom AR, et al. Carotid intima‐media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010;55:1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Polak JF, Pencina MJ, O'Leary DH, et al. Common carotid artery intima‐media thickness progression as a predictor of stroke in multi‐ethnic study of atherosclerosis. Stroke. 2011;42:3017–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wyman RA, Gimelli G, McBride PE, et al. Does detection of carotid plaque affect physician behavior or motivate patients? Am Heart J. 2007;154:1072–1077. [DOI] [PubMed] [Google Scholar]
- 4. Johnson HM, Turke TL, Grossklaus M, et al. Effects of an office‐based carotid ultrasound screening intervention. J Am Soc Echocardiogr. 2011;24:738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McEvoy JW, Blaha MJ, Nasir K, et al. Impact of coronary computed tomographic angiography results on patient and physician behavior in a low‐risk population. Arch Intern Med. 2011;171:1260–1268. [DOI] [PubMed] [Google Scholar]
- 6. Kalia NK, Miller LG, Nasir K, et al. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. 2006;185:394–399. [DOI] [PubMed] [Google Scholar]
- 7. Sandwell JC, Wingard DL, Laughlin GA, et al. Electron beam computed tomography screening and heart disease risk factor modification. Prev Cardiol. 2006;9:133–137. [DOI] [PubMed] [Google Scholar]
- 8. Bovet P, Perret F, Cornuz J, et al. Improved smoking cessation in smokers given ultrasound photographs of their own atherosclerotic plaques. Prev Med. 2002;34:215–220. [DOI] [PubMed] [Google Scholar]
- 9. Rodondi N, Collet TH, Nanchen D, et al. Impact of carotid plaque screening on smoking cessation and other cardiovascular risk factors: a randomized controlled trial. Arch Intern Med. 2012;172:344–352. [DOI] [PubMed] [Google Scholar]
- 10. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:e584–e636. [DOI] [PubMed] [Google Scholar]
- 11. Naghavi M, Falk E, Hecht HS, et al; SHAPE Task Force . From vulnerable plaque to vulnerable patient—Part III: Executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98:2H–15H. [DOI] [PubMed] [Google Scholar]
- 12. Ferket BS, Genders TS, Colkesen EB, et al. Systematic review of guidelines on imaging of asymptomatic coronary artery disease. J Am Coll Cardiol. 2011;57:1591–1600. [DOI] [PubMed] [Google Scholar]
- 13. Yoon YE, Rivera JJ, Kwon DA, et al. National Cholesterol Education Panel III guidelines performance role in preventing myocardial infarction in a large cohort without a history of coronary artery disease: Korea Acute Myocardial Infarction Registry study. Prev Cardiol. 2009;12:109–113. [DOI] [PubMed] [Google Scholar]
- 14. Eleid MF, Lester SJ, Wiedenbeck TL, et al. Carotid ultrasound identifies high‐risk subclinical atherosclerosis in adults with low Framingham risk scores. J Am Soc Echocardiogr. 2010;23:802–808. [DOI] [PubMed] [Google Scholar]
- 15. Naqvi TZ, Mendoza F, Rafii F, et al. High prevalence of ultrasound‐detected carotid atherosclerosis in subjects with low Framingham risk score: potential implications for screening for subclinical atherosclerosis. J Am Soc Echocardiogr. 2010;23:809–815. [DOI] [PubMed] [Google Scholar]
- 16. Wilson PW, D'Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. [DOI] [PubMed] [Google Scholar]
- 17.Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed]
- 18. Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima‐Media Thickness Task Force. Endorsed by the Society for Vascular Medicine [published correction appears in J Am Soc Echocardiogr. 2008;21:376]. J Am Soc Echocardiogr. 2008;21:93–111. [DOI] [PubMed] [Google Scholar]
- 19. Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007;28:1462–1536. [DOI] [PubMed] [Google Scholar]
- 20. Orakzai RH, Nasir K, Orakzai SH, et al. Effect of patient visualization of coronary calcium by electron beam computed tomography on changes in beneficial lifestyle behaviors. Am J Cardiol. 2008;101:999–1002. [DOI] [PubMed] [Google Scholar]
- 21. European Association for Cardiovascular Prevention and Rehabilitation , Reiner Z, Catapano AL, et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32:1769–1818. [DOI] [PubMed] [Google Scholar]
- 22. Hackam DG, Shojania KG, Spence JD, et al. Influence of noninvasive cardiovascular imaging in primary prevention: systematic review and meta‐analysis of randomized trials. Arch Intern Med. 2011;171:977–982. [DOI] [PubMed] [Google Scholar]
- 23. O'Malley PG, Feuerstein IM, Taylor AJ. Impact of electron beam tomography, with or without case management, on motivation, behavioral change, and cardiovascular risk profile: a randomized controlled trial. JAMA. 2003;289:2215–2223. [DOI] [PubMed] [Google Scholar]
- 24. Young LH, Wackers FJ, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA. 2009;301:1547–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rozanski A, Gransar H, Shaw LJ, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. LaBounty TM, Devereux RB, Lin FY, et al. Impact of coronary computed tomographic angiography findings on the medical treatment and control of coronary artery disease and its risk factors. Am J Cardiol. 2009;104:873–877. [DOI] [PubMed] [Google Scholar]


