Abstract
Background:
Cardiac rehabilitation (CR) promotes long‐term positive health behaviours, such as physical activity (PA), in patients following a cardiovascular event. We have limited knowledge of long‐term PA and its correlates. Therefore, this research examined both PA behaviour and socioecological correlates among elderly graduates 2‐6 years following CR.
Hypothesis:
CR graduates will have a moderate PA level in the long term. Greater PA will be associated with various multilevel correlates.
Methods:
This was a retrospective, cross‐sectional study which quantified PA using the Physical Activity Scale for the Elderly (PASE) and collected information about socioecological correlates at the intrapersonal, interpersonal and health service levels. Both univariate and multivariate analyses assessed PA and PA correlates.
Results:
The majority of the 584 participants were older (69.8 ± 9.8), male (80.3%), and well educated (75.4% ≥ some post‐secondary). Average time since CR graduation was 41.5 ± 11.5 months. Seventy five percent of CR graduates reported current weekly PA levels that met, or exceeded, Canadian PA guidelines (>150 minutes of moderate‐vigorous PA). Univariate analyses identified 13 PASE score correlates. Multivariate analyses identified age, PA enjoyment, current work status, CR staff support, location of primary residence, and perceived health as significantly associated with higher PASE scores (p < 0.001).
Conclusions:
Three and a half years post‐CR graduates had high PA levels. Greater PA was associated with several modifiable multilevel correlates at all levels of influence. Understanding correlates of long‐term PA behaviour among CR graduates will help identify groups at risk for nonadherence and assist with continued program development.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Compared to patients who only receive conventional in‐hospital care, patients who complete a cardiac rehabilitation (CR) program following a cardiac event experience a significant reduction in all‐cause mortality1, 2, 3 by 20% to 25% within 3 years.3 CR programs are traditionally short‐term multifaceted interventions that include physical activity (PA) as a core element.2, 4, 5 One of the overarching objectives of CR is to encourage patients to maintain PA at guideline‐recommended levels after program completion. Current Canadian PA guidelines for effective health advocate at least 150 minutes of moderate–vigorous PA per week.6 There is some evidence that states that PA behavior among CR graduates in the short term (1 year post‐CR) often fails to meet the recommendations.7, 8 There is very little evidence on PA behavior over the long term (2 or more years).
Encouraging positive health behaviors among CR graduates is a complex process that involves many levels of influence. To examine these levels of influence, a comprehensive approach to health promotion must be employed, such as the socioecological model.9 The socioecological model integrates intra‐ and interpersonal factors, community and organizational factors (or institutional), and public policies.9, 10 Using this model as a guide, the current research focuses on factors within 3 levels of influence: the intrapersonal level, interpersonal level, and health service level.
To our knowledge, no original research has been undertaken to examine long‐term PA behavior following CR, specifically in relation to the socioecological model. Consequently, this study first evaluates the degree to which graduates of cardiac rehabilitation participate in physical activity, and then identifies the most influential correlates of physical activity. The time frame examined is 2 to 6 years post‐CR.
Methods
Procedure and Design
Approval was obtained from the University of Toronto and the Toronto Rehabilitation Institute Research ethics boards for a retrospective cross‐sectional study. The Toronto Rehabilitation Institute is a large academic CR program that offers a 12‐month, comprehensive, guideline‐based2 program to cardiac patients. While enrolled in the 12‐month program, patients complete supervised exercise (aerobic and resistive) sessions and are offered both health information and counseling sessions. Successful graduate status is granted to patients with ≥80% program attendance. Further details on the program have been previously published.11
All those enrolled in a program at the Toronto Rehabilitation Institute are asked if they are willing to be contacted for research in the future. For this research, eligible participants were English‐speaking CR graduates from between 2005 and 2009. They were mailed packages including an invitation to participate, an introductory letter, a consent form, and a questionnaire. Questionnaires assessed both PA behavior and socioecological factors predicted to affect this behavior. To reduce bias, both branching questions and the “check all that apply” option were avoided.12 In total, information was gathered for 15 candidate PA correlates at the intrapersonal level, 9 at the interpersonal level, and 4 at the health service level.
Measures
Dependent Variable—Physical Activity Assessment:
The outcome of interest (dependent variable) was PA. To quantify PA, a self‐reported questionnaire called the Physical Activity Scale for the Elderly (PASE)13 was used because of its accepted validity,14 reliability,15 and suitability for CR graduates.16 To calculate an individual's PASE score, the total time spent doing individual activities such as leisure activity, household chores, and occupational activities, is multiplied by respective item weights (available for each activity reported). The various products are then summed.13 A higher PASE score indicates greater PA.
The PASE questionnaire was also used to compute whether or not a participants PA level met Canadian recommendations of ≥150 minutes of moderate–vigorous activity per week.6 There are 3 PASE items that capture specific recommended activities: walking (item 2), moderate activity (item 4), and strenuous activity (item 5). Using these 3 items only, a new variable was computed as either meeting current PA guidelines or not.
Independent Variables—Socioecological Correlate Assessment:
As seen in Table 1, the socioecological model describes 5 levels of influence on behavior. The current research focuses on factors within 3 levels of influence: the intrapersonal level, interpersonal level, and health service level. Based on the socioecological model9, 10 and a review of the literature,17 there were a total of 28 potential PA correlates assessed at 3 of these levels, 15 at the intrapersonal level, 9 at the interpersonal level, and 4 at the health service level. At the intrapersonal level sociodemographic items included age, sex, and self‐reported level of education. Self‐reported clinical items included height and weight (to calculate body mass index), smoking status, blood pressure control, cholesterol control, medication compliance, number of comorbidities, and number of recurrent events. Clinical items extracted from patient records included peak aerobic capacity (VO2 peak) test at the program start (initial) and end (final). Perceived health, motivation to exercise, and PA enjoyment were each scored on a 5‐point Likert scale. The final item at the intrapersonal level, fear of falling, was assessed nominally as yes/no.
Table 1.
Socioecological Model Levels of Influence
| Level of Influence | Description |
|---|---|
| Intrapersonal | Individual characteristics that influence behavior, such as knowledge, attitudes, beliefs, and personality traits. |
| Interpersonal | Interpersonal processes and groups (family, friends, and peers) that provide social identity, support, and role definition. |
| Organizational/service | Rules, regulations, policies, and informal structures that may constrain or promote recommended behaviors. |
| Community | Social networks and norms, or standards, which exist as formal or informal among individuals, groups, and organizations. |
| Public policy | Local, state, and/or federal policies and laws that regulate or support healthy actions and practices for disease prevention, early detection, control, and management. |
At the interpersonal level, self‐reported items included ethnicity, household income, current marital status, current work status (as either full time or non‐full time), primary residence location (as either rural or nonrural), birthplace, preferred PA location, and mode of transportation to PA. Social support was assessed using the Tangible, Informational, and Emotional Social Support Survey (TIES), which is a 16‐item survey with higher scores indicative of greater social support.18
Finally, at the health service level, all 4 items were self‐reported. Contact with health services was quantified as the number of visits within the past 6 months to either a family doctor or a cardiologist.19 Healthcare staff support of PA was assessed nominally. The final correlate of CR staff support assessed patients' perceptions of CR staff encouragement in regard to future activity behaviors, measured as the number of health directives a patient could recall receiving.
Statistical Analysis
IBM SPSS version 19 (IBM SPSS, Armonk, NY) was used for all analyses. Descriptive statistics, including means with standard deviation or frequencies with percentages, was performed on the PASE with each correlate. Outputs can be found in Table 2.
Table 2.
PASE Score Correlates According to the Socioecological Model.
| Correlate | Mean ± SD/No. (%) | Relation to PASE Score |
|---|---|---|
| Intrapersonal level | ||
| Age (y) | 69.8 ± 9.8 | r = −0.35a |
| Sex, male | 469 (80.3%) | t(582) = 39.16a |
| Highest level of education | F(5, 566) = 0.819 | |
| <High school | 63 (11.0%) | |
| High school | 78 (13.6%) | |
| Some postsecondary | 112 (19.6%) | |
| Postsecondary | 153 (26.7%) | |
| Graduate/professional | 166 (29.1%) | |
| BMI (kg/m2) | 26.9 ± 5.02 | r = 0.01 |
| Smoking status | F(2, 575) = 1.52 | |
| Currently smoke | 33 (5.7%) | |
| Quit | 302 (52.4%) | |
| Never smoked | 242 (41.9%) | |
| Blood pressure control | F(2, 581) = 1.07 | |
| Yes | 544 (97.5%) | |
| No | 11 (2.9%) | |
| Don't know | 3 (0.5%) | |
| Cholesterol control | F(2, 42.31) = 7.49b | |
| Yes | 522 (89.5%) | |
| No | 21 (3.7%) | |
| Don't know | 40 (6.8%) | |
| Medication compliance, yes >80% of the time | 564 (97.7%) | r = 0.05 |
| Number of comorbidities | 1.65 ± 1.42 | r = −0.20a |
| Arthritis | 179 (30.8%) | |
| Diabetes | 123 (21.1%) | |
| Digestive | 64 (11.0%) | |
| Respiratory | 64 (11.0%) | |
| Other | 151 (26.1%) | |
| Number of recurrent events | 0.53 ± 0.85 | r = −0.06 |
| Arrhythmia | 81 (13.9%) | |
| Angina | 74 (12.7%) | |
| None | 379 (65.1%) | |
| Other | 48 (8.3%) | |
| VO2 peak (mL/kg/min)c | ||
| Intake | 18.6 ± 5.1 | r = 0.23a |
| Graduation | 23.1 ± 7.7 | r = 0.27a |
| Perceived health | F(4, 570) = 9.03a | |
| Excellent | 77 (13.4%) | |
| Very good | 159 (27.7%) | |
| Good | 233 (40.5%) | |
| Fair | 95 (16.5%) | |
| Poor | 11 (1.9%) | |
| Motivation to exercise | F(4, 531) = 1.38 | |
| Physician | 47 (8.8%) | |
| Me | 439 (81.2%) | |
| Friends | 19 (3.5%) | |
| Other | 31(5.8%) | |
| No choice | 4 (0.7%) | |
| PA enjoyment | F(5, 556) = 6.84a | |
| Very little | 40 (7.1%) | |
| Little | 38 (6.7%) | |
| Somewhat | 169 (30.0%) | |
| Much | 162 (28.8%) | |
| Very much | 154 (27.4%) | |
| Fear of falling, yes | 135 (23.6%) | t(572) = 38.55a |
| Interpersonal level | ||
| Ethnicity | F(8, 567) = 0.74 | |
| North American | 301 (52.3%) | |
| European | 165 (28.6%) | |
| Other | 110 (19.1%) | |
| Household income | F(11, 482) = 1.55 | |
| $0 to $39,999 | 129 (26.1%) | |
| $40,000 to $79,000 | 173 (35.0%) | |
| >$80, 000 | 192 (38.9%) | |
| Marital status | F(3, 570) = 5.71a | |
| Married | 453 (78.9%) | |
| Widow | 46 (8.0%) | |
| Separated/divorced | 40 (7.0%) | |
| Single | 35 (6.1%) | |
| Work status | t(186.9) = 7.46a | |
| Full time | 138 (24.0%) | |
| Non‐full time | 438 (76.0%) | |
| Primary residence location | t(574) = −3.0b | |
| Urban | 469 (81.4%) | |
| Nonurban | 107 (18.6%) | |
| Birthplace | t(576) = 38.81 | |
| Canada | 328 (56.8%) | |
| Other | 249 (43.2%) | |
| Preferred PA location | F(8, 501) = 1.45 | |
| Community locations | 273 (53.6%) | |
| Private locations | 237 (46.4%) | |
| Mode of transportation to PA | F(7, 539) = 3.18b | |
| Personal modes | 389 (71.1%) | |
| Public modes | 44 (8.0%) | |
| None | 114 (20.9%) | |
| Social support (TIES) | 20.95 ± 9.43 | r = 0.10d |
| Health service level | ||
| Number of visits to a family doctor | 2.73 ± 2.61 | r = −0.06 |
| Number of visits to a cardiologist | 0.78 ± 0.71 | r = −0.07 |
| Healthcare staff support | t(676) = 42.14 | |
| Yes, PA suggestion(s) made | 99 (17.4%) | |
| No, PA suggestion not made | 469 (82.6%) | |
| CR staff support (% yes) | 355 (61%) | r = 0.15d |
| Was asked how | 391 (69.6%) | t(560) = 2.99b |
| Was asked where | 215 (38.4%) | t(558) = 2.36d |
| Was provided information | 138 (23.5%) | t(559) = 2.74)d |
| None | 126 (22.4%) | t(560) = −2.47d |
Abbreviations: BMI, body mass index; CR, cardiac rehabilitation; PA, physical activity; PASE, Physical Activity Scale for the Elderly; SD, standard deviation; TIES, Tangible, Informational, and Emotional Social Support Survey; VO2 peak, peak aerobic capacity. a P < 0.001. b P < 0.005. c Denotes information collected from patient chart. d P < 0.01.
Univariate analyses were used to investigate the initial association between each correlate and total PASE score (the dependent variable) using either Pearson correlation, one way analysis of variance, or Student t test as appropriate. The significance level was set at P < 0.05. Afterward, a stepwise multivariate linear regression analysis was computed to ascertain a correlate model of total PASE score. Only those variables related to PASE in the univariate analyses were entered into the model. Regression diagnostics were performed, and the presence of multicollinearity was assessed using eigenvalues and condition indices.
Results
Based on research inclusion criteria, between 2005 and 2009 there were 1642 CR graduates who consented to be contacted for research, and they were all mailed study materials. Of these, 1058 either declined or were nonresponsive, and 584 consented to participate (36% response rate, Figure 1).
Figure 1.
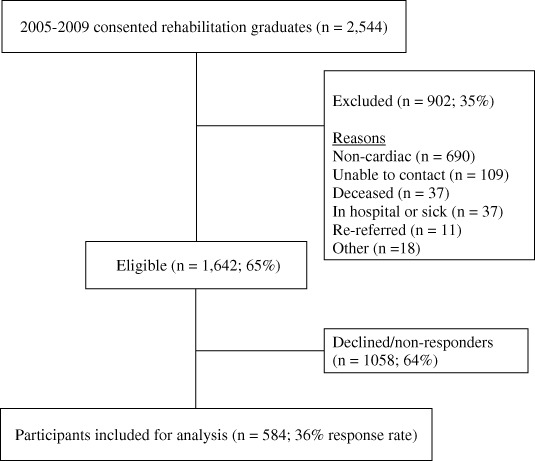
Recruitment flow diagram.
Descriptive characteristics of participants can be found in Table 2. The average time since CR graduation was 41.5 ± 11.5 months, with no significant association between the number of months since CR graduation and PASE scores (r = 0.02, P = 0.66).
Dependent Variable—Physical Activity Assessment
PASE scores ranged from 0 to 432.1 (122.9 ± 74.6). PASE scores were normally distributed with acceptable measures of skewness (0.92 ± 0.10) and kurtosis (0.74 ± 0.20). Two cases were identified as potential outliers; however, further exploration determined their respective values to be indicative of overall activity. Four hundred thirty‐seven (75%) participants were meeting the Canadian PA guidelines for older adults6 at the time of questionnaire distribution.
Independent Variables—Socioecological Correlate Assessment
Of the 15 correlates assessed at the intrapersonal level, those that had a statistically significant association with greater PASE scores (Table 2) were younger age, male sex, cholesterol control, fewer comorbidities, higher VO2 peak at both measurement points, higher perceived health, greater PA enjoyment, and no fear of falling. Of the 9 correlates assessed at the interpersonal level, those who had a statistically significant association with greater PASE scores (Table 2) were higher household income, being married, full‐time work status, living outside the city, having a personal form of transportation, and higher social support (TIES). Of the 4 correlates assessed at the health service level (Table 2), the only item that had a statistically significant association with greater PASE scores (Table 2) was higher level of perceived support from CR staff.
Multivariate Correlate Model
After confirming normality, linearity, and homoscedasticity of residuals (plots omitted), a stepwise linear regression was performed which included correlates that were significant at the univariate level. All tolerance values within the final model were above 0.74, and all variance inflation factors (VIFs) were below 1.3, indicating the absence of multicollinearity.20 The final regression model accounts for 23.9% of the variance in total PASE scores and includes at least 1 correlate from each of the socioecological levels assessed: PASE score = 226.75 + (−1.60·Age) + (13.90·PAenjoyment) + (−31.24·WorkStatus) + (7.93·CRstaffSupport) + (19.46· PrimaryResidenceLocation) + (7.93·PerceivedHealth). Full analysis can be seen in Table 3.
Table 3.
Stepwise Linear Regression Output
| Unstandarized β | SE Unstandardized β | Standarized β | Significance (P) | |
|---|---|---|---|---|
| Step 1 | ||||
| Constant | 302.99 | 21.69 | ||
| Age | −2.58 | 0.31 | −0.34 | <0.001 |
| Step 6 | ||||
| Constant | 226.75 | 26.84 | ||
| Age | −1.60 | 0.33 | −0.21 | <0.001 |
| PA enjoyment | 13.90 | 2.53 | 0.22 | <0.001 |
| Work status | −31.24 | 7.48 | −0.18 | <0.001 |
| CR staff support | 7.93 | 2.82 | 0.11 | 0.005 |
| Primary residence location | 19.46 | 7.15 | 0 .10 | <0.01 |
| Perceived health | 7.93 | 3.06 | −0.10 | <0.05 |
Abbreviations: CR, cardiac rehabilitation; PA, physical activity; SE, standard error. R 2 = 0.24 for step 6 (P < 0.001).
Discussion
Physical Activity Level
An average of 3.5 years after CR completion, three quarters of study participants reported PA participation at a level that meets the current Canadian PA guidelines of ≥150 minutes of moderate–vigorous intensity activity per week.6 To our knowledge, few studies have reported such high percentages of PA post‐CR, although considerable variation between studies is evident. Both Zullo et al21 and Moore et al22 reported low activity adherence of 41% and 48%, respectively, whereas Bock et al8 reported high activity adherence of 84%. Results from the present study fall within these ranges but support higher PA adherence. More importantly, the current results dispute skeptics who perceive PA is not maintained post‐CR.
The wide range of reported PA adherence values may be related to PA measurement techniques. Several methods are available including accelerometers, heart rate monitors, direct calorimetry, indirect activity logs, and self‐reported questionnaires.16 For large cross‐sectional studies, self‐reported questionnaires are the method of choice despite the potential for social desirability bias to cause an exaggeration of PA levels when compared to more objective measures.23, 24 Using objective measures in large cross‐sectional studies of CR graduates is rare, with only 2 groups utilizing heart rate wristwatch monitors22 and pedometers.25 Additionally, discrepancies in reported PA participation may be related to the amount of time since CR graduation, which ranges across studies from 1 month to a few years. However, there was no significant relationship between PA levels and time since graduation in the current study.
Socioecological Correlates of Physical Activity
In this study, a comprehensive list of evidence‐based correlates potentially related to PA among CR graduates at the intrapersonal, interpersonal, and health service levels was investigated. Many of the findings were consistent with the literature; greater PA was significantly associated with male sex, younger age, better perceived health status, higher VO2 peak, better cholesterol control, greater social support, higher income, location, being married, and full‐time work status.21, 25 To our knowledge, we were first to identify among this population a significant relationship between PA and the correlates of PA enjoyment, number of comorbidities, fear of falling, mode of transportation to PA, and CR staff support. The PA enjoyment variable is particularly interesting.
Current literature describes PA enjoyment as an impactful correlate of PA among adolescents.26, 27 Our results indicate that this relationship may be extended to also include an older population of CR graduates. It has been shown that within CR PA enjoyment may be mediated by immediate program benefits such as weight loss.28 However, in the current study CR and its immediate benefits occurred many years ago suggesting a deeper, habitual, intrinsic source of PA enjoyment. It is important that future studies continue to explore this correlate because a lack of PA enjoyment may lead to withdrawal from CR programs and inactivity.29
A stepwise linear regression identified the strongest model able to predict PA behavior among CR graduates. This model included established items (age and work status) and new items (PA enjoyment, CR staff support, and home location). Additionally, the model may identify potential groups who are vulnerable to PA dropout including those who were female, unmarried, of older age, with a lower fitness capacity, a higher number of comorbidities, and a fear of falling.
Historically, women have been dramatically under‐represented in CR programs30, 31 despite documented benefits.2, 3 The present participant pool was only 19.1% female. This low percentage is to be expected when considering the high CR dropout rates reported in women.32 Creating environments focused on women and heart health is especially important because women reported lower PASE scores (103.8 ± 69.8) when compared to men (125.7 ± 74.6) (t582 = 2.86, P < 0.005). In‐depth PASE analysis revealed that women were more likely to participate in light housework and the caring of others. Other activities, such as gardening, lawn work, and light to moderate exercise/sport, are PA opportunities available to women with the potential for further development. By incorporating other vulnerable traits, such as fear of falling, CR programs may continue to develop attractiveness to at‐risk groups.
Limitations
This study and its conclusion about PA must be read within its limitations. There is potential self‐selection and social desirability bias that may have been present in this pool of CR graduates who were eager to volunteer for research. Our response rate was 36%. Those who responded were likely more motivated and health conscious than nonresponders33; however, emerging evidence suggests that nonresponse bias may not be a large threat to the generalizability of findings.34 In comparison to a previous sample of 5922 CR patients at the same center, there were no differences in smoking status, marital status, or the sex ratio of our respondents. However, the current sample was less obese, had greater intake VO2peak, and had a higher proportion of diabetes.11 Nevertheless, a repeat mailing should have been instituted to increase the response rate. The overall generalizability of the results are limited in that this study was undertaken at a single CR center with a program that is both long in duration and financially covered under the provincial government. Finally, the cross‐sectional study design, although common in CR research, meant that we could not come to causal conclusions about the PA correlates and PA.
Conclusion
Three quarters of CR graduates were achieving at least the minimum level of PA associated with health benefits 2 to 6 years post‐CR. This PA maintenance may contribute to the mortality and morbidity benefits reported in meta‐analyses on CR outcomes.30 As a final regression model, younger age, PA enjoyment, working status, CR staff support, home location, and high perceived health were significantly related to greater PA. The importance of both post‐CR PA enjoyment and encouragement from CR staff should not be underestimated within the CR environment.
Acknowledgements
The authors thank all participants who volunteered their time to complete the questionnaire. In addition, the authors thank Jack Goodman, Amy Hwang, and Peter Polyzotis for their help in this research project.
References
- 1. Heran BS, Chen JM, Ebrahim S, et al. Exercise‐based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(7):CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stone JA, Clark AM, Arena R. Cardiac rehabilitation as chronic disease care. In: Stone JA, Arthur HM, Suskin NG, eds. Cardiac Guidelinesfor Cardiac Rehabilitation and Cardiovascular Disease Prevention. 3rd ed. Winnipeg, Manitoba, Canada: Canadian Association of Cardiac Rehabilitation; 2009:73–103. [Google Scholar]
- 3. Chase JA. Systematic review of physical activity intervention studies after cardiac rehabilitation. J Cardiovasc Nurs. 2011;26:351–358. [DOI] [PubMed] [Google Scholar]
- 4. Fletcher GF, Balady GJ, Amsterdam EA, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 2001;104:1694–1740. [DOI] [PubMed] [Google Scholar]
- 5. Wenger NK, Froelicher ES, Smith LK, et al. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1999;17:1–23. [PubMed] [Google Scholar]
- 6. Tremblay MS, Warburton DE, Janssen I, et al. New Canadian physical activity guidelines. Appl Physiol Nutr Metab. 2011;36:36–46. [DOI] [PubMed] [Google Scholar]
- 7. Willich SN, Muller‐Nordhorn J, Kulig M, et al. Cardiac risk factors, medication, and recurrent clinical events after acute coronary disease; a prospective cohort study. Eur Heart J. 2001;22:307–313. [DOI] [PubMed] [Google Scholar]
- 8. Bock BC, Carmona‐Barros RE, Esler JL, et al. Program participation and physical activity maintenance after cardiac rehabilitation. Behav Modif. 2003;27:37–53. [DOI] [PubMed] [Google Scholar]
- 9. McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. [DOI] [PubMed] [Google Scholar]
- 10. Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10:282–298. [DOI] [PubMed] [Google Scholar]
- 11. Marzolini S, Mertens DJ, Oh PI, et al. Self‐reported compliance to home‐based resistance training in cardiac patients. Eur J Cardiovasc Prev Rehabil. 2010;17:35–41. [DOI] [PubMed] [Google Scholar]
- 12. Dillman D, Christian L. Survey mode as a source of instability in responses across surveys. Field Methods. 2005;17:30–52. [Google Scholar]
- 13. Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. [DOI] [PubMed] [Google Scholar]
- 14. Bonnefoy M, Normand S, Pachiaudi C, et al. Simultaneous validation of ten physical activity questionnaires in older men: a doubly labeled water study. J Am Geriatr Soc. 2001;49:28–35. [DOI] [PubMed] [Google Scholar]
- 15. Harada ND, Chiu V, King AC, et al. An evaluation of three self‐report physical activity instruments for older adults. Med Sci Sports Exerc. 2001;33:962–970. [DOI] [PubMed] [Google Scholar]
- 16. Le Grande MR, Elliott PC, Worcester MU, et al. An evaluation of self‐report physical activity instruments used in studies involving cardiac patients. J Cardiopulm Rehabil Prev. 2008;28:358–369. [DOI] [PubMed] [Google Scholar]
- 17. Petter M, Blanchard C, Kemp KA, et al. Correlates of exercise among coronary heart disease patients: review, implications and future directions. Eur J Cardiovasc Prev Rehabil. 2009;16:515–526. [DOI] [PubMed] [Google Scholar]
- 18. Boutin‐Foster C, Alexander J. Development and validation of the Tangible, Informational, and Emotional Social Support Survey. J Cardiopulm Rehabil. 2006;26:307–313. [DOI] [PubMed] [Google Scholar]
- 19. White S, Bissell P, Anderson C. Patients' perspectives on cardiac rehabilitation, lifestyle change and taking medicines: implications for service development. J Health Serv Res Policy. 2010;15(suppl 2):47–53. [DOI] [PubMed] [Google Scholar]
- 20. Field A. Discovering Statistics Using SPSS. 3rd ed. Thousand Oaks, CA: SAGE Publications; 2009. [Google Scholar]
- 21. Zullo MD, Dolansky MA, Jackson LW. Cardiac rehabilitation, health behaviors, and body mass index post‐myocardial infarction. J Cardiopulm Rehabil Prev. 2010;30:28–34. [DOI] [PubMed] [Google Scholar]
- 22. Moore SM, Dolansky MA, Ruland CM, et al. Predictors of women's exercise maintenance after cardiac rehabilitation. J Cardiopulm Rehabil. 2003;23:40–49. [DOI] [PubMed] [Google Scholar]
- 23. Ewald B, McEvoy M, Attia J. Pedometer counts superior to physical activity scale for identifying health markers in older adults. Br J Sports Med. 2010;44:756–761. [DOI] [PubMed] [Google Scholar]
- 24. Shields M, Tremblay MS, Laviolette M, et al. Fitness of Canadian adults: results from the 2007–2009 Canadian Health Measures Survey. Health Rep. 2010;21:21–35. [PubMed] [Google Scholar]
- 25. Izawa KP, Yamada S, Oka K, et al. Long‐term exercise maintenance, physical activity, and health‐related quality of life after cardiac rehabilitation. Am J Phys Med Rehabil. 2004;83:884–892. [DOI] [PubMed] [Google Scholar]
- 26. Wiley AR, Flood TL, Andrade FC, et al. Family and individual predictors of physical activity for older Mexican adolescents. J Adolesc Health. 2011;49:222–224. [DOI] [PubMed] [Google Scholar]
- 27. Jago R, Davis L, McNeill J, et al. Adolescent girls' and parents' views on recruiting and retaining girls into an after‐school dance intervention: implications for extra‐curricular physical activity provision. Int J Behav Nutr Phys Act. 2011;8:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pope L, Harvey‐Berino J, Savage P, et al. The impact of high‐calorie‐expenditure exercise on quality of life in older adults with coronary heart disease. J Aging Phys Act. 2011;19:99–116. [DOI] [PubMed] [Google Scholar]
- 29. Rivett MJ, Tsakirides C, Pringle A, et al. Physical activity readiness in patient withdrawals from cardiac rehabilitation. Br J Nurs. 2009;18:188–191. [DOI] [PubMed] [Google Scholar]
- 30. Jolliffe JA, Rees K, Taylor RS, et al. Exercise‐based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001;(1):CD001800. [DOI] [PubMed] [Google Scholar]
- 31. Sanderson BK, Shewchuk RM, Bittner V. Cardiac rehabilitation and women: what keeps them away? J Cardiopulm Rehabil Prev. 2010;30:12–21. [DOI] [PubMed] [Google Scholar]
- 32. Marzolini S, Brooks D, Oh PI. Sex differences in completion of a 12‐month cardiac rehabilitation programme: an analysis of 5922 women and men. Eur J Cardiovasc Prev Rehabil. 2008;15: 698–703. [DOI] [PubMed] [Google Scholar]
- 33. Haskell WL, Alderman EL, Fair JM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP). Circulation. 1994;89:975–990. [DOI] [PubMed] [Google Scholar]
- 34. Davern M, McAlpine D, Beebe TJ, et al. Are lower response rates hazardous to your health survey? An analysis of three state telephone health surveys. Health Serv Res. 2010;45:1324–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]


