Abstract
The purpose of this study was to evaluate the impact of a community-based food education program on nutrition-related knowledge in middle-aged and older patients with type 2 diabetes (T2D). Participants (n = 36; 65.9 ± 6.0 years old) were recruited in primary health care to a 9-month community-based lifestyle intervention program for patients with T2D and randomly assigned to an exercise program (control group; n = 16) or an exercise program plus a food education program (experimental group; n = 20). Nutrition-related knowledge was assessed through a modified version of the General Nutrition Knowledge Questionnaire. The increase in total nutrition-related knowledge score and sources of nutrients area score was significantly higher in the experimental group compared to the control group. No significant changes in nutrition-related knowledge were found between groups in dietary recommendations and diet-disease relationship areas, although improvements were observed. This community-based food education program, with the use of easy to implement strategies (short-duration lectures and dual-task problem solving activities during exercise), had a positive and encouraging impact on nutrition-related knowledge in middle-aged and older patients with T2D.
Keywords: community-based intervention, food education program, nutrition-related knowledge, type 2 diabetes
1. Introduction
Diabetes is a public health problem that is increasing worldwide [1]. According to International Diabetes Federation (IDF), in Europe, in 2017, there were 58 million individuals with diabetes [2]. This number is expected to increase by 16% until 2045, reaching the value of 67 million people with diabetes [2]. In Portugal, more than 1 million people between the ages of 20 and 79 have diabetes [3]. Type 2 diabetes (T2D) is the most common type of diabetes [3], and its prevalence is likely to increase with age [4]. The adverse effects of hyperglycemia can be categorized into microvascular (diabetic nephropathy, neuropathy, and retinopathy) and macrovascular complications [5]. Cardiovascular and cerebrovascular diseases are the most common macrovascular complications and the main causes for morbidity and mortality among T2D patients [6]. The adoption of a balanced diet is one of the pillars of diabetes control [7]. For T2D patients, the reduction of energy intake is recommended through the maintenance of a healthy eating pattern based on the intake of unsaturated fats, high fiber foods such as fruits, vegetables, whole grains, and legumes, and limited alcohol intake [2,8]. However, the adherence to nutritional recommendations is generally disregarded by these patients [9]. Nutrition-related knowledge is one of the factors that can influence the adoption of a healthy diet [10] and T2D patients tend to present deficits in this area [11,12,13,14,15]. Therefore it is urgent that this population has access to self-management education focused on nutritional contents. In what concerns diabetes, despite the existence of general nutrition recommendations for self-management education [16], the best intervention remains to be identified [17]. In Portugal, as in many other European countries, caring for people with T2D occurs essentially within the primary health care system [18], which may be a successful place for the implementation of nutritional interventions, due to the fact that there is a closer contact with the patients, and the possibility to provide permanent care [19]. Despite the importance of primary health care, supportive environments are also required to promote behavior changes [20]. Thus, community-based interventions are of particular public health interest as they reach T2D patients in their natural living environment and, when replicated, may attain population level impact [21]. It is the responsibility of nutrition educators to find out innovative solutions so that the community can be aware of the indispensable role of diet in diabetes management [22]. We only found one study in the community setting that analyzed nutrition-related knowledge after the application of a food education program (developed for Korean American Immigrants) [23]. Hence, we carried out a pilot study to evaluate the impact of a community-based food education program on nutrition-related knowledge in middle-aged and older patients with T2D.
2. Methods
2.1. Study Design
This was a randomized controlled trial for patients with T2D conducted in Vila Real, Portugal, comparing an exercise program only (CON) and an exercise program plus a food education program (EXP). All patients received information to maintain their diabetes management (lifestyle-related physical activity and pharmacological plan), and to continue their medical consultations during the study.
2.2. Participants
The implementation of the community-based lifestyle intervention programs was planned for two groups of 25 participants each (the limit of our human, material, and infrastructure resources), representing a total of 274 h of intervention (135 h in the control group and 139 h in the experimental group). Predicting an initial refusal rate of 25%, primary health care medical doctors were asked to select 65 participants according to several inclusion criteria (Table 1).
Table 1.
Inclusion criteria for participation in the study.
| Inclusion Criteria for Participation in the Study |
|---|
| Diagnosed with T2D for at least six months |
| Aged between 50 and 80 years old |
| Non-smokers |
| Not engaged in supervised exercise |
| Independent living in the community |
| Medical recommendation for lifestyle intervention |
| Known medical history |
| Diabetes comorbidities under control (diabetic foot, retinopathy, and nephropathy) |
| No cardiovascular, respiratory, and musculoskeletal contraindications to exercise |
| Without major problems in gait or balance |
| Not started insulin therapy in the past three months |
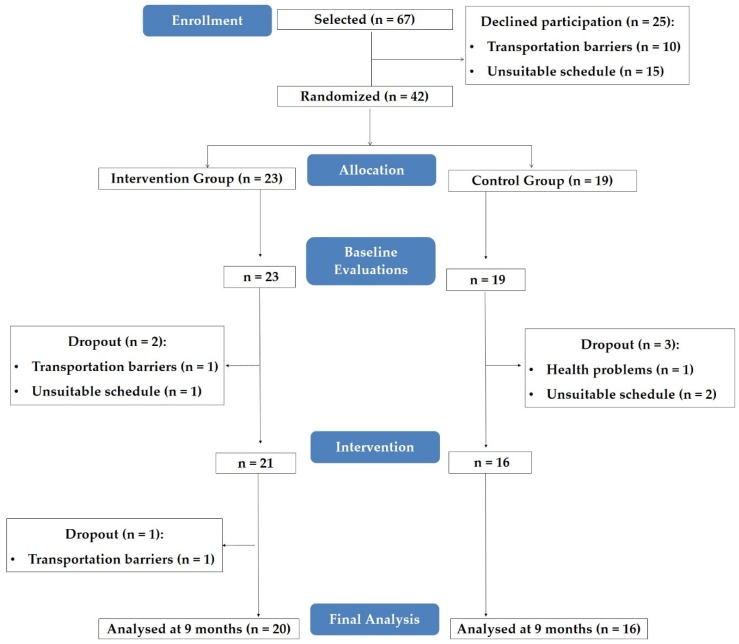
Investigators received information of 67 primary health care patients with T2D. A total of 42 agreed to participate in the study and were randomized, following simple randomization procedures with the use of a computer software, for CON (19 patients) or EXP (23 patients) (Figure 1).
Figure 1.
Participants’ flow chart.
Level of adherence to the food education program was not considered an exclusion criterion for final analysis. The reasons for dropouts are explained in Section 3.
The study protocol was approved by the local health ethics committee in accordance with the Declaration of Helsinki. All patients gave written informed consent before participation, including capture images. The trial was registered at ClinicalTrials.gov, number NCT02631902.
2.3. Exercise Program
All patients participated in a 9-month community-based exercise program [24,25], developed according with international exercise recommendations for patients with T2D [26]. As the mean age of our participants was 65.9 ± 6.0 years old, the exercise program was also based in international recommendations on falls prevention [27]. This program consisted of three exercise sessions per week, 75 min per session, combining aerobic, resistance, agility/balance, and flexibility exercise.
2.4. Food Education Program
Patients randomized to the EXP group received, plus the exercise program, a 16-week food education program (Figure 2) based on IDF nutrition teaching modules [28], and American Diabetes Association (ADA) dietary recommendations for T2D management [8]. On each week, a different nutrition-related content (Table 2) was addressed through two sessions: (1) a theoretical session of 15 min performed before one exercise session; and (2) dual-task strategies integrated in another exercise session: (food label interpretation (Figure 3); traffic light system with individual response (Figure 4) or group discussion (Figure 5); multiple choice answers after one question with individual response (Figure 6), or group discussion (Figure 7)). Attendance was recorded at each session.
Figure 2.
Food education program and exercise program timeline.
Table 2.
Contents of the food education program.
| Week | Contents |
|---|---|
| Week 1 | Diabetes, insulin, and glycaemia |
| Week 2 | Functions of nutrients |
| Week 3 | Sources of nutrients |
| Week 4 | Food Wheel (fruit, vegetables, cereals, rice, and potatoes) |
| Week 5 | Food Wheel (meat, fish and eggs, dairy products, fats, and oils) |
| Week 6 | Glycemic index and glycemic load |
| Week 7 | Added sugars |
| Week 8 | Carbohydrate counting |
| Week 9 | Food label interpretation (carbohydrates; sugars) |
| Week 10 | Food label interpretation (fats; saturated fats) |
| Week 11 | Dietetic products (lean, diet, light, zero) |
| Week 12 | Fats |
| Week 13 | Soup and salt |
| Week 14 | Drinks |
| Week 15 | Cooking methods |
| Week 16 | Meal planning and the healthy eating plate |
Figure 3.
Food label interpretation during walking exercise. Participants were asked to select, among two, which food label had more carbohydrate, added sugar, fat, or saturated fat.
Figure 4.
Traffic light system (individual response) during walking exercise: green color—best food choices; yellow color—choose carefully; red color—foods to avoid.
Figure 5.
Traffic light system (group discussion) during walking exercise: green color—best food choices; yellow color—choose carefully; red color—foods to avoid.
Figure 6.
Multiple choice answer during walking exercise. Participants were asked to select, among two, which foods had more sugar, fat, saturated fat, glycemic index, or glycemic load.
Figure 7.
Multiple choice answer (group discussion) during walking exercise. Participants were asked to select, among two, which foods had more sugar, fat, saturated fat, glycemic index, or glycemic load.
2.5. Evaluations
Demographic data, such as age, gender, education level, personal monthly (net) income, marital status, and living situation were recorded by a standard questionnaire. Diabetes data, such as HbA1c and diabetes duration were collected by primary health care medical doctors. HbA1c was assessed by a fasting (minimum of 8 h) venous blood analysis according to standard international laboratory methods before entrance in the study. Cognitive function was also evaluated by the investigators through Mini Mental State Examination, with all patients included regardless of classification.
Nutrition-related knowledge was assessed, before and after the 9-month intervention, by the Portuguese modified short version [29] of the General Nutrition Knowledge Questionnaire (GNKQ) [30]. This version of the questionnaire consisted of three sections: dietary recommendations (DR, 0–6 points); sources of nutrients (SN, 0–34 points), and diet-disease relationship (DDR, 0–16 points). Correct responses from each section were added, giving an overall score out of 56 points. Differences between the original questionnaire and the one used in our study are presented in Table 3. Participants answered on a range of different scales, such as ‘more, equal, less, don’t know’, ‘yes, no, don’t know’, ‘rich, poor, don´t know’, ‘agree, disagree, don´t know’. In the diet-disease relationship section, some items were open-ended and required participants to list diseases associated with diet-related lifestyle factors.
Table 3.
Differences between the General Nutrition Knowledge Questionnaire and the Portuguese modified short version of the General Nutrition Knowledge Questionnaire.
| Section | GNKQ | Portuguese Modified Short Version of GNKQ |
|---|---|---|
| Section 1 | Three multiple choice and one open-ended question | One multiple choice question |
| Section 2 | 21 multiple choice questions | Eight multiple choice questions |
| Section 3 | 10 multiple choice questions | No questions—lack of internal consistency and item validation |
| Section 4 | Five multiple choice and five open-ended questions | Five multiple choice and four open-ended questions |
GNKQ: General Nutrition Knowledge Questionnaire.
2.6. Data Analysis
Data are shown as mean ± SD for continuous variables and as proportions (number and percentage) for categorical variables.
To compare the effects of the time * group interaction on nutrition-related knowledge, analysis of variance (ANOVA) with repeated measures was performed. Partial eta squared values (µ2p) were reported to quantify the effect sizes. To identify factors that were independently associated with significant improvements in nutrition-related knowledge in the EXP group, a multiple linear regression analysis was performed. The level of statistical significance was set at p < 0.05 and data were analyzed with PASW Statistics version 20 (IBM SPSS, Hong Kong, China).
3. Results
3.1. Program Implementation
From the individuals initially selected, 37% refused to participate in the study, indicating as reasons transportation barriers or unsuitable schedule. Thus, 42 participants were randomized and evaluated (23 in the EXP group and 19 in the CON group). Prior to the start of the intervention, five participants dropped out (two in the EXP group (unsuitable schedule, n = 1, transportation barriers, n = 1) and three in the CON group (health problems, n = 1, unsuitable schedule, n = 2). Another dropout in EXP group was verified during the intervention due to transportation barriers (n = 1).
In the final analysis, 16 patients from the CON group and 20 patients from the EXP group were included (Figure 1). Attendance to the food education program was 47.5% ± 27.1% (ranging from 2.9% to 85.3%).
3.2. Participants’ Characteristics
The mean age of the 36 participants was 65.9 ± 6.0 years old (20 males). Participants had T2D diagnosed at 6.3 ± 5.2 years and HbA1c of 7.0% ± 1.1%. Final sample characteristics are presented in Table 4.
Table 4.
Characteristics of the study participants according to group.
| Characteristics | CON Group (n = 16) | EXP Group (n = 20) |
|---|---|---|
| Age, mean ± SD | 63.00 ± 5.39 | 68.25 ± 5.60 |
| Gender, n (%) | ||
| Male | 10 (62.5) | 10 (50.0) |
| Female | 6 (37.5) | 10 (50.0) |
| Education level, n (%) | ||
| ≤4 years | 9 (56.3) | 11 (55.0) |
| 5 to 9 years | 4 (25.0) | 6 (30.0) |
| >9 years | 3 (18.8) | 3 (15.0) |
| Personal monthly income, n (%) | ||
| <500 € | 3 (18.8) | 11 (55.0) |
| Between 500 and 1000 € | 7 (43.7) | 6 (30.0) |
| More than 1000 € | 6 (37.5) | 3 (15.0) |
| Marital status, n (%) | ||
| Single, divorced, or widower | 3 (18.8) | 4 (20.0) |
| Married or with domestic partner | 13 (81.2) | 16 (80.0) |
| Living situation, n (%) | ||
| Living alone | 1 (6.3) | 3 (15.0) |
| Living with others | 15 (93.7) | 17 (85.0) |
| Glycated hemoglobin, mean ± SD | 6.87 ± 1.13 | 7.18 ± 1.13 |
| Diabetes duration, mean ± SD | 7.63 ± 5.73 | 5.30 ± 4.57 |
| Mini Mental State score, mean ± SD | 26.56 ± 2.94 | 26.25 ± 2.97 |
CON: Control; EXP: Experimental.
3.3. Nutrition-Related Knowledge
The mean values of nutrition-related knowledge (total and per section) in CON and EXP groups in the two evaluation moments are presented in Table 5. The increase in total nutrition-related knowledge and SN area was significantly higher in the EXP group compared to the CON group. No significant changes in nutrition-related knowledge were found between groups in DR and DDR areas, although improvements were observed, mainly in the EXP group.
Table 5.
Nutrition-related knowledge (total and per section) in two evaluation moments in both groups.
| Nutrition-Related Knowledge (Points) | Control Group | Experimental Group | p | η2p | ||
|---|---|---|---|---|---|---|
| Baseline | 9 Months | Baseline | 9 Months | |||
| Total score | 30.2 ± 6.1 | 31.3 ± 7.4 | 29.4 ± 6.2 | 35.2 ± 5.7 | 0.001 | 0.290 |
| Dietary recommendations section | 5.0 ± 0.5 | 5.1 ± 0.6 | 4.9 ± 0.8 | 5.5 ± 0.6 | 0.053 | 0.106 |
| Sources of nutrients section | 18.8 ± 4.9 | 19.1 ± 5.5 | 17.8 ± 5.1 | 21.9 ± 4.5 | 0.004 | 0.217 |
| Diet-disease relationship section | 6.4 ± 1.5 | 7.1 ± 2.1 | 6.8 ± 1.7 | 7.9 ± 1.5 | 0.513 | 0.013 |
p: p-value of the time * group interaction effect determined by analysis of variance with repeated measures; η2p: partial eta squared.
Table 6 shows the factors independently associated with the increase in nutrition-related knowledge in the EXP group. After adjustment, increase in nutrition-related knowledge was significantly and negatively associated with diabetes duration (β = −0.543, p = 0.020) and significantly and positively associated with attendance to the food education program (β = 0.096, p = 0.011).
Table 6.
Factors independently associated with the increase in nutrition-related knowledge in the experimental group.
| Factors | β (95% CI) | p |
|---|---|---|
| Age | −0.043 (−0.355, 0.270) | 0.763 |
| Gender | 0.710 (−2.814, 4.234) | 0.659 |
| Education level | −2.819 (−6.015, 0.378) | 0.077 |
| Personal monthly income | 1.522 (−1.632, 4.677) | 0.303 |
| Marital status | 4.034 (−2.649, 10.717) | 0.205 |
| Living situation | −3.394 (−10.682, 3.895) | 0.320 |
| Glycated hemoglobin | 0.154 (−1.504, 1.811) | 0.839 |
| Diabetes duration | −0.543 (−0.977, −0.109) | 0.020 |
| Mini Mental State Examination score | −0.042 (−0.863, 0.778) | 0.910 |
| Attendance to food education program | 0.096 (0.028, 0.165) | 0.011 |
β: standard coefficient determined by multiple regression analysis; CI: confidence interval; p: p-value of the association of independent factors with nutrition-related knowledge in the experimental group.
Participants performed a Mini Mental State Examination to evaluate cognitive function. According to cutoffs from the Portuguese adapted version of this instrument [31], five patients (three from CON and two from EXP groups) were classified with cognitive impairment. For ethical reasons, these individuals were not excluded from participation in the study neither from the final analysis. In these patients, nutrition-related knowledge between the baseline assessment and the final analysis increased 8.3% (1.2% in the CON group and 19.6% in the EXP group).
4. Discussion
Our study revealed that a community-based food education program significantly increased nutrition-related knowledge in middle-aged and older patients with T2D. Participants’ global improvements are mostly derived from the evolution in scores of sources of nutrients. The emphasis of our food education program on contents from this knowledge area is likely to be the reason for this change. On the contrary, differences between groups were not found in dietary recommendations and diet-disease relationship areas. In dietary recommendations, participants from CON and EXP groups started with a high score (5.0 and 4.9 points respectively) in a maximum section scale of 6 points, which makes improvements harder to achieve. Regarding the diet-disease relationship area, the results may have been conditioned by the design of the questions, as half of questions were open-ended [32]. Furthermore, this was the final section of the instrument and, according to Rolstad et al. [33], the length of the survey can increase response burden.
The increase of nutrition-related knowledge is associated with healthier food patterns [10] and may lead to a better glycemic control in T2D patients [34]. Nutrition-related knowledge is a key component of diabetes knowledge. Most educational interventions analyzed in scientific studies with T2D patients focused on diabetes knowledge without presenting results for patients’ knowledge about nutrition management of diabetes [35,36,37,38,39]. Some studies showed the effectiveness of a nutritional intervention in nutrition-related knowledge of T2D patients [22,40,41,42,43]. However, as far as we know, there is only one published RCT conducted in a community setting, with Korean American immigrants [22], that assessed the effectiveness of a nutrition education program on nutrition-related knowledge in patients with T2D (n = 79; 56.5 ± 7.9 years). After two group face-to-face sessions (two hours each; one week apart) devoted to nutritional contents, there were significant differences in nutrition-related knowledge with the intervention group scoring better, as assessed after 30 weeks.
It is difficult to discuss between our study and that of Song et al. [22] because of different sample characteristics, assessment instruments, and baseline scores. As explicit memory (recognition) declines with age, the fact that average age of our participants was higher than Song’s study (65.9 ± 6.0 vs. 56.5 ± 7.9 years) makes their learning more difficult [44]. Song et al. [22] used the Diabetes Knowledge Test with seven multiple choice questions for nutrition-related knowledge, while in our trial we applied the GNKQ, comprised of three different areas of nutrition-related knowledge (DR, SN, and DDR). According to Worsley [45], it is of crucial importance to measure different areas of nutrition-related knowledge, as this outcome is not one dimensional. Contrary to Song’s results, participants from our trial started with a baseline score above 50% (29.8 out of 56 points), being more difficult to improve nutrition-related knowledge.
In our study, we used face-to-face group education delivered over 16 weeks, lasting a total of 12 h. The classes were based on IDF nutrition teaching modules [27] and ADA dietary recommendations for T2D control [28], given through theoretical classes together with dual-task problem solving strategies during exercise.
Face-to-face education is one of the most common educational methods, as it enables patients to ask and discuss their doubts, allowing the construction of a dynamic relationship between the educator and patients [46]. Despite this, there are a rising number of studies conducted in T2D patients delivering education through technology-based methods [35,47,48,49,50]. Although technology-based programs have the potential to solve the problem of distance to the place of intervention, they can represent a barrier to patients from lower socioeconomic and educational groups, such as the patients from our EXP group, who are more likely to have lower digital literacy and more difficulties in the access and use of technologies [51].
According to Coppola et al. [52], there are three different methods to provide patient education: during usual care, structured group, and individual education. Two meta-analyses [53,54] showed the benefits of group-based education on diabetes knowledge, when compared with individual education. Group education provides opportunities for patients’ interactions, making possible discussions about several topics. Moreover, it provides support from others facing similar challenges, allowing participants to feel integrated in a group context [55].
In what concerns the duration of nutritional programs, interventions conducted in T2D patients presented variable results, ranging from 2 h and 40 min [56] to 25 h [42] and being delivered between 1 week [22,49] to 6 months [43,57]. Steinsbeck et al. [54], in a systematic review of group-based T2D self-management education, concluded that interventions delivered between 6 and 10 months and with 19 to 52 h of duration give the best results in diabetes knowledge.
Regarding the development of food education programs, ADA recommendations for T2D management were also used by Song et al. [22], with some contents similar to those used in our study, such as carbohydrate counting, food pyramid, healthy eating plate, and meal planning. Other nutritional interventions that improved diabetes knowledge in T2D patients also had similar contents to our study: definition of diabetes [36,37,38], meal planning [38], meal frequency [38], cooking methods [37], importance of fruit, vegetable, and whole grains [37], and healthy eating [36,38].
Our intervention was centered on two teaching methods: structured lecture (15-min group class) and dual-task problem solving (30 min integrated in one exercise session). Lectures are the best teaching method to transmit declarative knowledge [58]. Problem solving tasks are a great indicator of functional ability in the elderly [59]. Furthermore, dual-task problem solving—in this study the completion of a secondary task while walking—is a key contributor for the prevention of falls in the elderly [60]. The use of this technique during exercise was the most innovative aspect of our study. In addition to preparing our patients to the dual-task problem solving of the daily life, it also allows them to target the lifestyle factors of T2D management. Although cognitive impairment may affect learning behaviors [61], the evolution of nutrition-related knowledge, even in these patients (assessed with Mini Mental State Examination), proves the efficacy of these simple teaching methods.
As expected, attendance to food education program was an independent factor associated with the increase of nutrition-related knowledge in our EXP group. As in our study, Bruce et al. [62] and Brown et al. [63] also found that higher attendance to educational sessions was related to greater knowledge levels.
Attendance to our food education program presented lower values compared with other educational interventions in T2D patients (47.5% vs. 72.5% [64], 74% [65], and 78% [66]). Attendance to interventions has a natural influence on its efficacy [67]. Identification of the motives of low attendance rates is of crucial importance for food education program feedback [68]. In our study, participants’ attendance was tracked. Whenever an individual missed two sessions in a row, a phone call was made to record the cause. Patients reported health status, weather, work, family activities, and transportation as constraints, meeting the reasons listed by Brzoska and Misra [69]. Therefore, there is a need for strategies to increase attendance to education sessions in people with T2D. Miller et al. [41,42] also tracked participant’s attendance. If T2D patients missed a group session, they were stimulated to attend a backup session. Participation of family members in the education sessions [22,70] and the presence of the community health professionals [22,71] are two other strategies that were used in interventions with T2D patients to promote class attendance.
The negative association between diabetes duration and the evolution in nutrition-related knowledge is another finding from our study. Hassing et al. [72] reported an association between diabetes mellitus and mild cognitive impairment, which is higher with longer duration of diabetes [73]. The accurate pathophysiology of cognitive dysfunction in diabetes is not totally defined, but probably hyperglycemia, vascular disease, hypoglycemia events, and insulin resistance are the main factors [74]. Diabetes is typically a progressive chronic disease that is often related to emotionally stressful events [75]. Chronic stress affects the function of the cognitive system, having implications for educational contexts [76]. According to Eom et al. [77], individuals with more years of diabetes have more diabetes-related stress.
The present study has some limitations that need to be addressed. Our food education program had an average low attendance level (48%). Another factor that should be highlighted was the existence of 37% of declines to participation from those originally selected by their medical doctors. Besides, we had 16% of dropouts following randomization. This underlines the difficulty in implementing lifestyle interventions for this population, even when culturally adapted and free of charge. Despite randomization, there is a five-year difference in the mean of the age between CON and EXP groups, quite a large difference for such a small trial.
Our study was strengthened by its randomized controlled design, the control of the effects of covariates on the evolution of nutrition-related knowledge in the EXP group, the application of short-duration lectures and the use of an innovative method (dual-task strategy) to give nutritional contents. Moreover, our questionnaire allowed data collection from three different areas of nutrition-related knowledge. In accordance to our search, this was the first study conducted in Portugal that evaluated the effect of a community-based food education program in nutrition-related knowledge, in middle-aged and older patients with T2D, in primary health care. Diabetes is a major public health problem in Portugal and worldwide.
5. Conclusions
In conclusion, this community-based food education program, with the use of easy to implement strategies (short-duration lectures and dual-task problem solving activities during exercise), had a positive and encouraging impact on nutrition-related knowledge in middle-aged and older patients with T2D. More research should be done to understand to which extent this increase in nutrition-related knowledge has an impact on dietary intake and diabetes-related outcomes.
Acknowledgments
The authors would like to acknowledge the support received from all institutions involved in the implementation of “Diabetes em Movimento” Vila Real, as well as to acknowledge to all participants in this study.
Author Contributions
Conceptualization, C.V. and R.M.; Data Curation, C.V. and M.C.; Formal Analysis, C.V. and R.M.; Investigation, C.V., A.A., and R.M.; Methodology, C.V., A.A., M.C., E.R., and R.M.; Project Administration, R.M.; Resources, C.V. and R.M.; Supervision, E.R. and R.; Validation, A.A., M.C., and E.R.; Visualization, C.V.; Writing—Original Draft, C.V.; Writing—Review and Editing, C.V., A.A., M.C., E.R. and R.M.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Tabish S.A. Is Diabetes Becoming the Biggest Epidemic of the Twenty-first Century? Int. J. Health Sci. 2007;1:5–8. [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation . IDF Diabetes Atlas. IDF; Brussels, Belgium: 2017. [Google Scholar]
- 3.Sociedade Portuguesa de Diabetologia . Diabetes: Factos e Números: O ano de 2015 Lisboa: Sociedade Portuguesa de Diabetologia. SPD; Lisboa, Portugal: 2016. [Google Scholar]
- 4.La Puente J.B.-D., Mundet-Tudurí X., Casellas A., Fernandez-Real J.M., Mauricio D., Mata-Cases M., Franch-Nadal J., Mundet-Tuduri X., Fernández-Real J.M., Mata-Cases M., et al. Older type 2 diabetic patients are more likely to achieve glycaemic and cardiovascular risk factors targets than younger patients: Analysis of a primary care database. Int. J. Clin. Pr. 2015;69:1486–1495. doi: 10.1111/ijcp.12741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chawla A., Chawla R., Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J. Endocrinol. Metab. 2016;20:546–551. doi: 10.4103/2230-8210.183480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shan P.-F., Li Q., Khamaisi M., Qiang G.-F. Type 2 Diabetes Mellitus and Macrovascular Complications. Int. J. Endocrinol. 2017;2017:4301461. doi: 10.1155/2017/4301461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ricci-Cabello I., Ruiz-Pérez I., Rojas-García A., Pastor G., Rodríguez-Barranco M., Gonçalves D.C. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: A systematic review, meta-analysis and meta-regression. BMC Endocr. Disord. 2014;14:60. doi: 10.1186/1472-6823-14-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evert A.B., Boucher J.L., Cypress M., Dunbar S.A., Franz M.J., Mayer-Davis E.J., Neumiller J.J., Nwankwo R., Verdi C.L., Urbanski P., et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2014;37(Suppl. 1):S120–S143. doi: 10.2337/dc14-S120. [DOI] [PubMed] [Google Scholar]
- 9.Vijan S., Stuart N.S., Fitzgerald J.T., Ronis D.L., Hayward R.A., Slater S., Hofer T.P. Barriers to following dietary recommendations in Type 2 diabetes. Diabet. Med. 2005;22:32–38. doi: 10.1111/j.1464-5491.2004.01342.x. [DOI] [PubMed] [Google Scholar]
- 10.Spronk I., Kullen C., Burdon C., O’Connor H. Relationship between nutrition knowledge and dietary intake. Br. J. Nutr. 2014;111:1713–1726. doi: 10.1017/S0007114514000087. [DOI] [PubMed] [Google Scholar]
- 11.Breen C., Ryan M., Gibney M.J., O’Shea D. Diabetes-related nutrition knowledge and dietary intake among adults with type 2 diabetes. Br. J. Nutr. 2015;114:439–447. doi: 10.1017/S0007114515002068. [DOI] [PubMed] [Google Scholar]
- 12.Doherty M.L., Owusu-Dabo E., Kantanka O.S., O Brawer R., Plumb J.D. Type 2 diabetes in a rapidly urbanizing region of Ghana, West Africa: A qualitative study of dietary preferences, knowledge and practices. BMC Public Health. 2014;14:1069. doi: 10.1186/1471-2458-14-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fitzgerald N., Damio G., Segura-Pérez S., Pérez-Escamilla R. Nutrition Knowledge, Food Label Use, and Food Intake Patterns among Latinas with and without Type 2 Diabetes. J. Am. Diet. Assoc. 2008;108:960–967. doi: 10.1016/j.jada.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 14.Klupa T., Możdżan M., Kokoszka-Paszkot J., Kubik M., Masierek M., Czerwińska M., Małecki M.T. Diet-Related Knowledge and Physical Activity in a Large Cohort of Insulin-Treated Type 2 Diabetes Patients: PROGENS ARENA Study. Int. J. Endocrinol. 2016;2016:1–6. doi: 10.1155/2016/2354956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ranasinghe P., Pigera A.S.A.D., Ishara M.H., Jayasekara L.M.D.T., Jayawardena R., Katulanda P. Knowledge and perceptions about diet and physical activity among Sri Lankan adults with diabetes mellitus: A qualitative study. BMC Public Health. 2015;15:1047. doi: 10.1186/s12889-015-2518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haas L., Maryniuk M., Beck J., Cox C.E., Duker P., Edwards L., Fisher E., Hanson L., Kent D., Kolb L., et al. National Standards for Diabetes Self-Management Education and Support. Diabetes Educ. 2012;38:619–629. doi: 10.1177/0145721712455997. [DOI] [PubMed] [Google Scholar]
- 17.Norris S.L., Engelgau M.M., Narayan K.V. Effectiveness of Self-Management Training in Type 2 Diabetes: A systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 18.Laranjo L., Neves A.L., Costa A., Ribeiro R.T., Couto L., Sá A.B. Facilitators, barriers and expectations in the self-management of type 2 diabetes—a qualitative study from Portugal. Eur. J. Gen. Pr. 2015;21:1–8. doi: 10.3109/13814788.2014.1000855. [DOI] [PubMed] [Google Scholar]
- 19.Davies M.J., Heller S., Skinner T.C., Campbell M.J., E Carey M., Cradock S., Dallosso H.M., Daly H., Doherty Y., Eaton S., et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: Cluster randomised controlled trial. BMJ. 2008;336:491–495. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glanz K., Rimer B., Viswarath K. Health Behavior and Health Education: Theory, Research and Practice. 4th ed. Jossey-Bass; San Francisco, CA, USA: 2008. [Google Scholar]
- 21.Brand T., Pischke C.R., Steenbock B., Schoenbach J., Poettgen S., Samkange-Zeeb F., Zeeb H. What Works in Community-Based Interventions Promoting Physical Activity and Healthy Eating? A Review of Reviews. Int. J. Environ. Res. Public Health. 2014;11:5866–5888. doi: 10.3390/ijerph110605866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hendrie G.A., Coveney J., Cox D. Exploring nutrition knowledge and the demographic variation in knowledge levels in an Australian community sample. Public Health Nutr. 2008;11:1365–1371. doi: 10.1017/S1368980008003042. [DOI] [PubMed] [Google Scholar]
- 23.Song H.-J., Han H.-R., Lee J.-E., Kim J., Kim K.B., Nguyen T., Kim M.T. Translating Current Dietary Guidelines into a Culturally Tailored Nutrition Education Program for Korean American Immigrants with Type 2 Diabetes. Diabetes Educ. 2010;36:752–761. doi: 10.1177/0145721710376328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mendes R., Sousa N., Reis V.M., Themudo-Barata J.L. Implementing Low-Cost, Community-Based Exercise Programs for Middle-Aged and Older Patients with Type 2 Diabetes: What Are the Benefits for Glycemic Control and Cardiovascular Risk? Int. J. Environ. Res. Public Health. 2017;14:1057. doi: 10.3390/ijerph14091057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendes R., Sousa N., Themudo-Barata J., Reis V. Impact of a community-based exercise programme on physical fitness in middle-aged and older patients with type 2 diabetes. Gac. Sanit. 2016;30:215–220. doi: 10.1016/j.gaceta.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Mendes R., Sousa N., Almeida A., Subtil P., Guedes-Marques F., Reis V.M., Themudo-Barata J.L. Exercise prescription for patients with type 2 diabetes-a synthesis of international recommendations: Narrative review. Br. J. Sports Med. 2016;50:1379–1381. doi: 10.1136/bjsports-2015-094895. [DOI] [PubMed] [Google Scholar]
- 27.Chodzko-Zajko W.J., Proctor D.N., Singh M.A.F., Minson C.T., Nigg C.R., Salem G.J., Skinner J.S. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009;41:1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 28.International Diabetes Federation . Diabetes Education Modules. IDF; Brussels, Belgium: 2011. [(accessed on 15 May 2019)]. Available online: https://d-net.idf.org/en/library/178-diabetes-education-modules-2011.html. [Google Scholar]
- 29.Souza J. Master’s Thesis. University of Porto; Porto, Portugal: 2009. [(accessed on 15 May 2019)]. Conhecimentos Nutritionais: Reprodução e Validação do Questionário. Available online: https://bibliotecadigital.ipb.pt/bitstream/10198/4274/1/tese%20de%20mestrado.pdf. [Google Scholar]
- 30.Parmenter K., Wardle J. Development of a general nutrition knowledge questionnaire for adults. Eur. J. Clin. Nutr. 1999;53:298–308. doi: 10.1038/sj.ejcn.1600726. [DOI] [PubMed] [Google Scholar]
- 31.Guerreiro M., Silva A., Botelho M., Leitão O., Castro-Caldas A., Garcia C. Adaptação à população portuguesa da tradução do Mini Mental State Examination. Rev. Port Neurol. 1994;1:9–10. [Google Scholar]
- 32.Kullen C.J., Iredale L., Prvan T., O’Connor H.T. Evaluation of General Nutrition Knowledge in Australian Military Personnel. J. Acad. Nutr. Diet. 2016;116:251–258. doi: 10.1016/j.jand.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 33.Rolstad S., Adler J., Ryden A. Response Burden and Questionnaire Length: Is Shorter Better? A Review and Meta-analysis. Value Health. 2011;14:1101–1108. doi: 10.1016/j.jval.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 34.Castro-Sánchez A.E., Ávila-Ortíz M.N. Changing Dietary Habits in Persons Living with Type 2 Diabetes. J. Nutr. Educ. Behav. 2013;45:761–766. doi: 10.1016/j.jneb.2013.04.259. [DOI] [PubMed] [Google Scholar]
- 35.Goodarzi M., Ebrahimzadeh I., Rabi A., Saedipoor B., Jafarabadi M.A. Impact of distance education via mobile phone text messaging on knowledge, attitude, practice and self efficacy of patients with type 2 diabetes mellitus in Iran. J. Diabetes Metab. Disord. 2012;11:10. doi: 10.1186/2251-6581-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Islam N.S., Wyatt L.C., Taher M., Riley L., Tandon S.D., Tanner M., Mukherji B.R., Trinh-Shevrin C. A Culturally Tailored Community Health Worker Intervention Leads to Improvement in Patient-Centered Outcomes for Immigrant Patients with Type 2 Diabetes. Clin. Diabetes. 2018;36:100–111. doi: 10.2337/cd17-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y., Xu M., Fan R., Ma X., Gu J., Cai X., Liu R., Chen Q., Ren J., Mao R., et al. The Effects of Intensive Nutrition Education on Late Middle-Aged Adults with Type 2 Diabetes. Int. J. Environ. Res. Public Health. 2016;13:897. doi: 10.3390/ijerph13090897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muchiri J., Gericke G., Rheeder P. Impact of nutrition education on diabetes knowledge and attitudes of adults with type 2 diabetes living in a resource-limited setting in South Africa: A randomised controlled trial. J. Endocrinol. Metab. Diabetes South Afr. 2016;21:26–34. doi: 10.1080/16089677.2016.1200324. [DOI] [Google Scholar]
- 39.Negarandeh R., Mahmoodi H., Noktehdan H., Heshmat R., Shakibazadeh E. Teach back and pictorial image educational strategies on knowledge about diabetes and medication/dietary adherence among low health literate patients with type 2 diabetes. Prim. Care Diabetes. 2013;7:111–118. doi: 10.1016/j.pcd.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 40.Miller C.K., Edwards L., Kissling G., Sanville L. Evaluation of a Theory-based Nutrition Intervention for Older Adults with Diabetes Mellitus. J. Am. Diet. Assoc. 2002;102:1069–1081. doi: 10.1016/S0002-8223(02)90242-7. [DOI] [PubMed] [Google Scholar]
- 41.Miller C.K., Jensen G.L., Achterberg C.L. Evaluation of a Food Label Nutrition Intervention for Women with Type 2 Diabetes Mellitus. J. Am. Diet. Assoc. 1999;99:323–328. doi: 10.1016/S0002-8223(99)00082-6. [DOI] [PubMed] [Google Scholar]
- 42.Miller C.K., Kristeller J.L., Headings A., Nagaraja H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A randomized controlled trial. Health Educ. Behav. 2014;41:145–154. doi: 10.1177/1090198113493092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pereira D.A., Costa N.M.D.S.C., Sousa A.L., Jardim P.C.B.V., Zanini C.R.D.O. The effect of educational intervention on the disease knowledge of diabetes mellitus patients. Rev. Latino Am. Enferm. 2012;20:478–485. doi: 10.1590/S0104-11692012000300008. [DOI] [PubMed] [Google Scholar]
- 44.Ward E.V., Berry C.J., Shanks D.R., Berry C. Age effects on explicit and implicit memory. Front. Psychol. 2013;4:639. doi: 10.3389/fpsyg.2013.00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Worsley A. Nutrition Knowledge and Food Consumption: Can Nutrition Knowledge Change Food Behaviour? Asia Pac. J. Clin. Nutr. 2002;11(Suppl. 3):S579–S585. doi: 10.1046/j.1440-6047.11.supp3.7.x. [DOI] [PubMed] [Google Scholar]
- 46.Hemmati Maslakpak M., Razmara S., Niazkhani Z. Effects of Face-to-Face and Telephone-Based Family-Oriented Education on Self-Care Behavior and Patient Outcomes in Type 2 Diabetes: A Randomized Controlled Trial. J. Diabetes Res. 2017;2017:8404328. doi: 10.1155/2017/8404328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dyson P.A., Beatty S., Matthews D.R. An assessment of lifestyle video education for people newly diagnosed with type 2 diabetes. J. Hum. Nutr. Diet. 2010;23:353–359. doi: 10.1111/j.1365-277X.2010.01077.x. [DOI] [PubMed] [Google Scholar]
- 48.Kandula N.R., Nsiah-Kumi P.A., Makoul G., Sager J., Zei C.P., Glass S., Stephens Q., Baker D.W. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ. Couns. 2009;75:321–327. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 49.Moussa M., Sherrod D., Choi J. An e-health intervention for increasing diabetes knowledge in African Americans. Int. J. Nurs. Pract. 2013;19(Suppl. 3):36–43. doi: 10.1111/ijn.12167. [DOI] [PubMed] [Google Scholar]
- 50.Alanzi T., Bah S., Alzahrani S., Alshammari S., Almunsef F., Turki A., Sulaiman B., Sara A., Sirah A., Fatima A. Evaluation of a mobile social networking application for improving diabetes Type 2 knowledge: An intervention study using WhatsApp. J. Comp. Eff. Res. 2018;7:891–899. doi: 10.2217/cer-2018-0028. [DOI] [PubMed] [Google Scholar]
- 51.Eysenbach G., Hansen M., Rosal M.C., Heyden R., Mejilla R., DePaoli M.R., Veerappa C., Wiecha J.M. Design and Methods for a Comparative Effectiveness Pilot Study: Virtual World vs. Face-to-Face Diabetes Self-Management. JMIR Res. Protoc. 2012;1:e24. doi: 10.2196/resprot.2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coppola A., Sasso L., Bagnasco A., Giustina A., Gazzaruso C. The role of patient education in the prevention and management of type 2 diabetes: An overview. Endocrine. 2016;53:18–27. doi: 10.1007/s12020-015-0775-7. [DOI] [PubMed] [Google Scholar]
- 53.Odgers-Jewell K., Ball L.E., Kelly J., Isenring E.A., Reidlinger D., Thomas R. Effectiveness of group-based self-management education for individuals with Type 2 diabetes: A systematic review with meta-analyses and meta-regression. Diabet. Med. 2017;34:1027–1039. doi: 10.1111/dme.13340. [DOI] [PubMed] [Google Scholar]
- 54.Steinsbekk A., Rygg L., Lisulo M., Rise M.B., Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv. Res. 2012;12:213. doi: 10.1186/1472-6963-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Odgers-Jewell K., Isenring E.A., Thomas R., Reidlinger D.P. Group participants’ experiences of a patient-directed group-based education program for the management of type 2 diabetes mellitus. PLoS ONE. 2017;12:e0177688. doi: 10.1371/journal.pone.0177688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sharifirad G., Entezari M.H., Kamran A., Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J. Res. Med. Sci. 2009;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 57.Wang H., Song Z., Ba Y., Zhu L., Wen Y. Nutritional and eating education improves knowledge and practice of patients with type 2 diabetes concerning dietary intake and blood glucose control in an outlying city of China. Public Health Nutr. 2014;17:2351–2358. doi: 10.1017/S1368980013002735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Charlton B.G. Lectures are such an effective teaching method because they exploit evolved human psychology to improve learning. Med. Hypotheses. 2006;67:1261–1265. doi: 10.1016/j.mehy.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 59.Kimbler K.J. Everyday Problem Solving and Instrumental Activities of Daily Living: Support for Domain Specificity. Behav. Sci. 2013;3:170–191. doi: 10.3390/bs3010170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liebherr M., Schubert P., Schiebener J., Kersten S., Haas C.T. Dual-tasking and aging—About multiple perspectives and possible implementations in interventions for the elderly. Cogent Psychol. 2016;3 doi: 10.1080/23311908.2016.1261440. [DOI] [Google Scholar]
- 61.Borson S. Cognition, Aging and Disabilities: Conceptual Issues. Phys. Med. Rehabil. Clin. N. Am. 2010;21:375–382. doi: 10.1016/j.pmr.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bruce D.G., Davis W.A., Cull C.A., Davis T.M.E. Diabetes education and knowledge in patients with type 2 diabetes from the community: The Fremantle Diabetes Study. J. Diabetes Complicat. 2003;17:82–89. doi: 10.1016/S1056-8727(02)00191-5. [DOI] [PubMed] [Google Scholar]
- 63.Brown S.A., Blozis S.A., Kouzekanani K., Garcia A.A., Winchell M., Hanis C.L. Dosage Effects of Diabetes Self-Management Education for Mexican Americans: The Starr County Border Health Initiative. Diabetes Care. 2005;28:527–532. doi: 10.2337/diacare.28.3.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rimmer J.H., Silverman K., Braunschweig C., Quinn L., Liu Y. Feasibility of a Health Promotion Intervention for a Group of Predominantly African American Women with Type 2 Diabetes. Diabetes Educ. 2002;28:571–580. doi: 10.1177/014572170202800411. [DOI] [PubMed] [Google Scholar]
- 65.Spencer M.S., Rosland A.-M., Kieffer E.C., Sinco B.R., Valerio M., Palmisano G., Anderson M., Guzman J.R., Heisler M. Effectiveness of a Community Health Worker Intervention Among African American and Latino Adults With Type 2 Diabetes: A Randomized Controlled Trial. Am. J. Public Health. 2011;101:2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rosal M.C., Olendzki B., Reed G.W., Ockene I., Gumieniak O., Scavron J. Diabetes self-management among low-income spanish-speaking patients: A pilot study. Ann. Behav. Med. 2005;29:225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 67.Vitolins M.Z., Rand C.S., Rapp S.R., Ribisl P.M., Sevick M.A. Measuring Adherence to Behavioral and Medical Interventions. Control. Clin. Trials. 2000;21:S188–S194. doi: 10.1016/S0197-2456(00)00077-5. [DOI] [PubMed] [Google Scholar]
- 68.Leung A.W.Y., Chan R.S.M., Sea M.M.M., Woo J. An Overview of Factors Associated with Adherence to Lifestyle Modification Programs for Weight Management in Adults. Int. J. Environ. Res. Public Health. 2017;14:922. doi: 10.3390/ijerph14080922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shawley-Brzoska S., Misra R. Perceived Benefits and Barriers of a Community-Based Diabetes Prevention and Management Program. J. Clin. Med. 2018;7:58. doi: 10.3390/jcm7030058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rosal M.C., Ockene I.S., Restrepo A., White M.J., Borg A., Olendzki B., Scavron J., Candib L., Welch G., Reed G. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: Latinos en control. Diabetes Care. 2011;34:838–844. doi: 10.2337/dc10-1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ortiz M., Lujan J., Ostwald S.K. Promotora Diabetes Intervention for Mexican Americans. Diabetes Educ. 2007;33:660–670. doi: 10.1177/0145721707304080. [DOI] [PubMed] [Google Scholar]
- 72.Hassing L.B., Hofer S.M., Nilsson S.E., Berg S., Pedersen N.L., McClearn G., Johansson B. Comorbid type 2 diabetes mellitus and hypertension exacerbates cognitive decline: Evidence from a longitudinal study. Age Ageing. 2004;33:355–361. doi: 10.1093/ageing/afh100. [DOI] [PubMed] [Google Scholar]
- 73.Roberts R.O., Geda Y.E., Knopman D.S., Christianson T.J., Pankratz V.S., Boeve B.F., Vella A., Rocca W.A., Petersen R.C. Association of duration and severity of diabetes mellitus with mild cognitive impairment. Arch Neurol. 2008;65:1066–1073. doi: 10.1001/archneur.65.8.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kodl C.T., Seaquist E.R. Cognitive Dysfunction and Diabetes Mellitus. Endocr. Rev. 2008;29:494–511. doi: 10.1210/er.2007-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ko S.-H., Park S.-A., Cho J.-H., Ko S.-H., Shin K.-M., Lee S.-H., Song K.-H., Park Y.-M., Ahn Y.-B. Influence of the Duration of Diabetes on the Outcome of a Diabetes Self-Management Education Program. Diabetes Metab. J. 2012;36:222–229. doi: 10.4093/dmj.2012.36.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vogel S., Schwabe L. Learning and memory under stress: Implications for the classroom. NPJ Sci. Learn. 2016;1:16011. doi: 10.1038/npjscilearn.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eom Y.S., Park H.S., Kim S.-H., Yang S.M., Nam M.S., Lee H.W., Lee K.Y., Lee S., Kim Y.S., Park I.B. Evaluation of Stress in Korean Patients with Diabetes Mellitus Using the Problem Areas in Diabetes-Korea Questionnaire. Diabetes Metab. J. 2011;35:182–187. doi: 10.4093/dmj.2011.35.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]