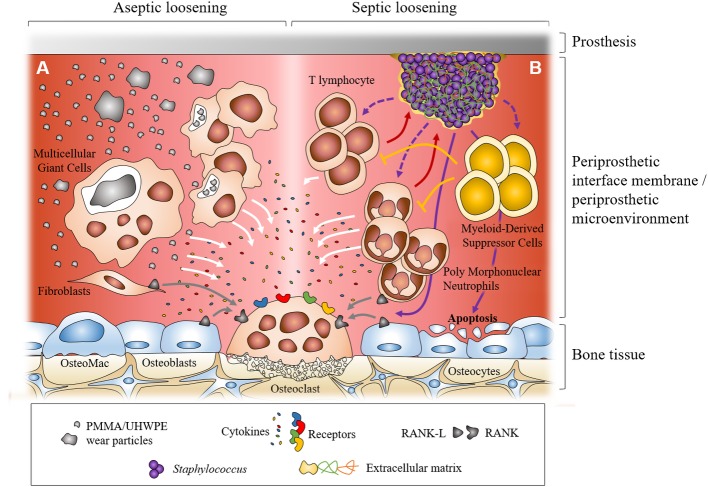
Figure 1.
Dual representation of the major cellular mechanisms during aseptic and septic loosening at the interface between prosthesis and bone. In aseptic loosening, small wear debris from the prosthesis is phagocytosed by macrophages and bigger particles are phagocytosed by multicellular giant cells. Frustrated phagocytosis leads to the production of pro-inflammatory cytokines. Activated fibroblasts in the interfacial membrane can also produce RANKL (A). In septic loosening, biofilm attached to the prosthesis can interact with polymorphonuclear neutrophils (PMNs) and T lymphocytes, which leads to the production of pro-inflammatory cytokines. Myeloid-derived suppressor cells (MDSCs) are recruited during biofilm-associated PJI. They can regulate immune response, notably inhibiting T lymphocyte proliferation. In PJI, recruited PMNs can express RANKL. Staphylococcal biofilm can also induce osteoblast apoptosis (B). In both situations, pro-inflammatory cytokines and RANKL can trigger the formation and activation of osteoclasts which leads to bone resorption and prosthesis loosening.