Abstract
Purpose.
Although estimates of heroin and injection drug use (IDU) among US adolescents have remained low and stable, national data may mask local variation in use. Adolescent use may be higher in urban areas, many of which have historically high rates of heroin use and IDU. We investigate trends in heroin use and IDU among 9th-12th grade students in major urban centers in the US.
Methods.
We used local Youth Risk Behavior Survey (YRBS) data from all large, urban school districts (n=9) with at least five years of weighted, publicly available data. We used time series mean estimation to estimate the prevalence of heroin use and IDU among high school students from 1999–2017 and used logistic regression to test for linear and quadratic trends.
Results.
We observed statistically significant linear increases in (1) lifetime heroin use in New York (β=0.43, 1%−3.9%), Chicago (β=0.15, 3.1%−4.6%), and Milwaukee (β=0.35, 2.8%−7.4%); and (2) lifetime IDU in New York (β=0.34, 0.8%−2.7%), Orange County (β=0.17, 2.2%−3.5%), and Miami-Dade County (β=0.16, 2.7%−3.9%). Only San Bernardino, experienced significant decreases in heroin use (β=−0.34, 4.6%−1.6%) and IDU (β=−0.20, 2.5%−1.9%) over the time period.
Conclusion.
In contrast to national trends, the prevalence of heroin use is increasing among adolescents in certain urban centers in the US. Our results illustrate that national averages mask local variation in adolescent heroin use. Further research with locally-representative samples is needed to inform public health policy and practice, especially in cities where heroin problems have been historically endemic and continue to rise.
Keywords: adolescent drug use, trends, opioids, heroin, injection drug use
The United States is currently facing an unprecedented opioid overdose crisis. Research with adults has documented transitions from non-medical prescription opioid use (NMPO) to heroin [1,2], substantial increases in unintentional overdose deaths [3,4], and surges in injection drug use (IDU) and HIV/Hepatitis C virus outbreaks [5]. Additional research shows an increased prevalence of opioid use in previously unaffected sociodemographic groups and localities, such as white males in rural areas [6,7]. Although research has documented the geographic context of the opioid epidemic among adults, the majority of research on adolescents has been done using national samples[8–12]. Studies using national data from large-scale substance use surveys – such as the Monitoring the Future (MTF) survey and Youth Risk Behavior Survey (YRBS) – indicate that adolescent heroin use has been relatively low (~ 2%) and stable over time [8,13]. Little research has examined local trends in adolescent opioid use, and even less work studies the effects of this epidemic among adolescents who live in urban areas where heroin use has been endemic for decades[14–17].
The lack of literature around adolescent opioid use represents an important limitation in our understanding of adverse health outcomes stemming from this epidemic. Heroin use accounts for the largest share of opioid overdoses among adolescents, is associated with injection drug and NMPO use, and leads to numerous negative health and social outcomes [5,18–20]. Adolescents who initiate heroin use are more likely to be suspended from school or drop out, report experiencing depressive symptoms, and have health problems [20]. Considering that urban environments are associated with increased availability and exposure to drugs [21] and a range of social determinants associated with vulnerability to substance use and substance use disorders (e.g., poverty), studying adolescent heroin use in urban jurisdictions is critical. Studies with adult populations demonstrate significant geographic variation in opioid and heroin use [22,23], and our research will address whether similar geographic variation exists for adolescent heroin use.
In addition to understanding regional variation in heroin use, studying the route of administration used by adolescents is critical because each route confers unique risks. Injection is a common route of heroin administration and is associated with escalation to opioid use disorder [20,24,25]. The health consequences of injection are numerous, and include vascular scarring (“track marks”) and disease transmission from unsterilized equipment, with one study showing that 68% of confiscated heroin contained bacterial pathogens linked to the development of skin abscesses and infections [26,27]. According to the 2017 MTF survey, among twelfth graders who reported lifetime use of heroin (0.6%), one-third reported only using with a needle, one- third reported never using a needle, and one-third reported both injecting and non-injection routes of administration [10]. Recently, Kleven and colleagues (2016) published the first study to examine trends in adolescent IDU from 1999 to 2013 at the national and local level. They showed that although IDU had not increased nationally, higher levels of IDU were found within specific cities, underscoring the value of local data [28]. Understanding injection drug use among adolescents is critical to prevention of HIV and Hepatitis C virus and escalation from opioid use to opioid use disorder.
To date, the literature on local variation in adolescent heroin and IDU in the United States is limited. To our knowledge, no study has examined the prevalence of adolescent heroin use at the local level. A focus on national data is insufficient to identify emerging local trends and can delay public health responses to new crises. Monitoring adolescent heroin use in urban areas is key to identifying early opportunities to intervene and prevent geographic disparities in health and psychosocial outcomes in youth. To address these gaps in the literature, we investigated trends in the prevalence of lifetime adolescent heroin use and IDU in nine urban school districts across the US.
Methods
We estimated the prevalence of lifetime heroin and IDU among high school students (grades 9 to 12) in nine local YRBS school districts and tested for changes over time between 1999 and 2017.
Data Source
Data for this study came from the Youth Risk Behavior Survey (YRBS), a cross- sectional, biennial survey managed by the Centers for Disease Control and Prevention (CDC)[29]. The YRBS is a school-based survey that uses multi-stage, cluster sampling to obtain a representative sample of high school students at the national, state, and local levels in the United States [30]. The YRBS is the only national survey of adolescent substance use that provides locally representative estimates for public use. The local YRBS surveys large, urban school districts in select cities and counties that choose to participate. Students are voluntary participants and complete an anonymous self-administered survey. This de-identified data was exempt from review from the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Analytic Sample and Inclusion Criteria
The CDC requires that all participating YRBS school districts have a minimum overall survey response rate of at least 60% in order for the CDC to weight their data by sex, grade, and race/ethnicity to produce locally representative estimates [31]. The 60% response rate is the product of school response rate (i.e., participating schools divided by all sampled) and individual response rate (participating students divided by number of students in the sampled classrooms).
We included data from all large, urban school districts that: (1) consented to have their YRBS survey data publicly available, (2) included items on heroin use, and (3) had at least five consecutive years of weighted data to allow us to estimate trends over time. Heroin use was first measured in the YRBS in 1999, therefore we have included all available survey years from 1999 to 2017. We excluded six districts that did not meet these criterion (Supplemental Table 1). Our analytic sample is comprised of nine urban school districts: Broward County (FL), Chicago (IL), Dallas (TX), Miami-Dade County (FL), Milwaukee (WI), New York City (NY), Orange County (FL), San Bernardino (CA), and San Diego (CA). Overall responses rates varied from 61–90% across districts (Supplemental Table 1). Within our analytic sample, some districts had missing years of data for heroin use or IDU because they declined to participate in the YRBS that year or because their data was not weighted (<60% response). Milwaukee did not collect data on IDU. Finally, we excluded students with missing responses for heroin use (5%) and IDU (9.6%, excluding Milwaukee). The sample size for lifetime heroin use was 180,552 and for IDU was 172,373.
Measures
Lifetime Heroin Use.
Students were asked about lifetime heroin use “During your life, how many times have you used heroin (also called smack, junk, or China White)?” and given six response choices of 0 times, 1 or 2 times, 3 to 9 times, 10 to 19 times, 20 to 39 times, and 40 or more times. From this, we derived a dichotomous variable for lifetime heroin use (ever/never).
Lifetime Injection Drug Use (IDU).
IDU was assessed by asking “During your life, how many times have you used a needle to inject any illegal drug into your body?” with three responses of 0, 1, or 2 or more times. Again, we derived a dichotomous variable indicating any lifetime IDU (ever/never).
Statistical Analyses
All analyses were performed in STATA/IC version 14.2 [32]. We estimated the prevalence and 95% confidence intervals (CIs) of lifetime heroin and IDU at each time point, using Stata’s “svy” package for survey proportion estimation [33]. This allowed us to produce estimates that were appropriately adjusted for complex sampling design of the YRBS, by accounting for clustered sampling or non-zero survey weights [33]. The CDC procedure for assigning survey weights to all YRBS data is described in detail elsewhere [30]. We used logistic regression to assess linear and quadratic trends over time, using a contrast command to assign orthogonal polynomial coefficients. The contrast command conducts an ANOVA-style test for trends and can be used to test for simple, nested, and interaction effects [32,34]. In the event that a YRBS district was missing a year in their time trend (i.e. 2015 for Chicago, IL), we were unable to run trend analysis if there were less than two years after the missing timepoint. If there were less than two timepoints, we ran trend analysis up until the most recent survey year (i.e. 2013 for Chicago, IL).
Results
Heroin Use
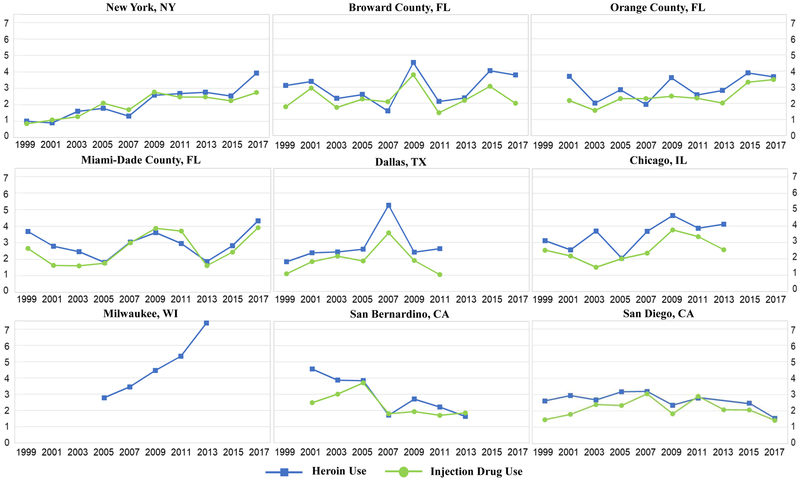
The highest mean prevalence of lifetime heroin use across years were found in Milwaukee, WI (4.5%, 95% CI: 3.80–5.31) and Chicago (3.58%, 95% CI: 3.03–4.22) (Table 1). New York City, NY had the lowest average prevalence of heroin use (2.11%, 95% CI:1.93–2.31). Despite variability in lifetime heroin use across individual districts, heroin use trends mirrored trends in lifetime IDU in every district (Figure 1). Miami-Dade County, FL had no significant trends over time. Three districts showed significant linear increases overtime: New York City (β=0.43, p <0.0001), Chicago, IL (β=0.15, p=0.02), and Milwaukee, WI (β=0.35, p=0.0001). Only one district, San Bernardino, CA, had a significant linear decrease (β=−0.34, p=0.0001) in the rate of heroin use over time and no quadratic trend (β=0.04, p=0.72). A positive quadratic trend for heroin use was found in three districts, Broward County (β=0.15, p=0.05) and Miami- Dade County, FL starting in 2011 (β=0.16, p=0.01) and San Diego, CA (β=0.49, p<0.0001), however neither of these localities had statistically significant linear trends over time. Dallas, TX was the only locality with both a marginally significant linear (β=0.14, p=0.06) and a significant quadratic trend (β= −0.15, p=0.02), indicating that there was a modest increase in heroin use that slowed over time. However, these Dallas trends were likely due to the peak in 2007 that normalized in the next survey year.
Table 1.
Percentage (95% CI) of 9th – 12th Grade Students Reporting Lifetime Heroin Use from 1999 to 2017 in 9 Urban Centers
| New York City, NY | Broward County, FL | Miami-Dade County, FL | Orange County, FL | Dallas, TX | Chicago, IL | Milwaukee, WI | San Bernardino, CA | San Diego, CA | |
|---|---|---|---|---|---|---|---|---|---|
| All Years | 2.11 (1.93, 2.31) | 2.92 (2.55, 3.35) | 2.89 (2.57, 3.23) | 3.00 (2.63, 3.41) | 2.78 (2.36, 3.28) | 3.58 (3.03, 4.22) | 4.5 (3.80, 5.31) | 2.85 (2.44, 3.33) | 2.66 (2.37, 2.99 |
| 1999 | 1.00 (0.57, 1.76) | 3.1 (2.25, 4.24) | 3.68 (2.63, 5.12) | -- | 1.81 (1.25, 2.62) | 3.11 (1.83, 5.23) | -- | -- | 2.61 (1.79, 3.77) |
| 2001 | 0.9 (0.48, 1.68) | 3.35 (2.30, 4.84) | 2.79 (2.07, 3.74) | 3.66 (1.83, 7.15) | 2.36 (1.60, 3.47) | 2.55 (1.65, 3.90) | -- | 4.56 (2.55, 8.03) | 2.94 (2.07, 4.15) |
| 2003 | 1.6 (1.28, 2.00) | 2.3 (1.40, 3.20) | 2.46 (1.81, 3.34) | 2.01 (1.00, 4.01) | 2.41 (1.76, 3.27) | 3.70 (2.57, 5.31) | -- | 3.87 (2.83, 5.29) | 2.67 (1.92, 3.70) |
| 2005 | 1.78 (1.33, 2.38) | 2.54 (1.61, 3.97) | 1.81 (1.27, 2.58) | 2.84 (1.91, 4.21) | 2.58 (1.84, 3.61) | 2.04 (0.93, 4.43) | 2.78 (1.92, 3.99) | 3.85 (2.44, 6.01) | 3.17 (2.37 4.23) |
| 2007 | 1.31 (0.90, 1.92) | 1.52 (0.86, 2.68) | 3.04 (2.33, 3.96) | 1.93 (1.28, 2.89) | 5.25 (3.59, 7.60) | 3.68 (2.15, 6.23) | 3.45 (2.62, 4.53) | 1.71 (1.18, 2.49) | 3.19 (2.36, 4.31) |
| 2009 | 2.58 (2.10, 3.16) | 4.53 (2.83, 7.20) | 3.61 (2.37, 5.47) | 3.58 (2.34, 5.43) | 2.4 (1.46, 3.92) | 4.65 (2.97, 7.20) | 4.46 (3.31, 5.99) | 2.7 (1.89, 3.84) | 2.35 (1.65, 3.33) |
| 2011 | 2.68 (2.26, 3.17) | 2.11 (1.23, 3.59) | 2.95 (2.06, 4.23) | 2.52 (1.59, 3.96) | 2.62 (1.82, 3.77) | 3.87 (2.89, 5.17) | 5.34 (3.67, 7.72) | 2.21 (1.56, 3.13) | 2.78 (1.94, 3.95) |
| 2013 | 2.76 (2.13, 3.57) | 2.33 (1.26, 4.27) | 1.86 (1.24, 2.78) | 2.8 (2.00, 3.91) | -- | 4.12 (2.57, 6.53) | 7.38 (4.95, 10.86) | 1.63 (1.03, 2.57) | -- |
| 2015 | 2.53 (1.95, 3.28) | 4.02 (2.89, 5.55) | 2.82 (1.93, 4.11) | 3.88 (2.34, 6.36) | -- | -- | -- | -- | 2.47 (1.85, 3.31) |
| 2017 | 3.92 (3.19, 4.80) | 3.75 (2.23, 6.23) | 4.32 (2.85, 6.49) | 3.64 (2.31, 5.68) | -- | 4.58 (2.96, 7.85) | -- | -- | 1.55 (0.88, 2.74) |
| Linear β (p-value) | 0.43 (<0.0001) | 0.06 (0.34) | 0.03 (0.57) | 0.10 (0.17) | 0.14 (0.06) | 0.15a (0.02) | 0.35 (0.0001) | −0.34 (0.0001) | 0.11 (0.17) |
| Quadratic β (p-value) | −0.03 (0.57) | 0.15 (0.05) | 0.13 (0.04) | 0.12 (0.11) | −0.15 (0.02) | 0.04a (0.59) | 0.02 (0.82) | 0.04 (0.72) | 1.01 (<0.0001) |
Note. Bold indicates statistical significance (p ≤ 0.05). A double dash indicates that the data were not available for the year.
Trend for Chicago, IL does not include 2017 (see Methods).
Figure 1. Trends in the Prevalence of Heroin and Injection Drug Use Among 9th-12th Graders, 1999–2017, by Urban Center.
Trends in lifetime heroin and IDU follow one another over time in all districts, suggesting there is overlap in their use.
Injection Drug Use
Chicago, IL had the highest mean prevalence of lifetime IDU use (2.73%, 95% CI: 2.36–3.15), while Dallas, TX had the lowest mean prevalence (1.85%, 95% CI:1.54–2.21) (Table 2). Despite variability in lifetime IDU among individual districts, IDU trends mirrored heroin trends in each district (Figure 1). Broward County, FL did not have any significant trends over time. Three districts showed significant linear increases over time: New York City, NY (β=0.34, p<0.0001), Orange County, FL (β=0.17, p=0.02), and Miami-Dade County, FL (β=0.16, p=0.01). Only one district, San Bernardino, CA, had a significant linear decrease (β=−0.20, p=0.05) over time, and no quadratic trend (β=−0.03, p=0.78). Significant quadratic trends were found in three districts, Dallas, TX (β= −0.16, p=0.02), San Diego, CA (β=−0.12, p=0.04) and Chicago, IL (β=−0.17, p=0.05), but were unaccompanied by significant linear trends that would make them meaningful to interpretation.
Table 2.
Percentage (95% CI) of 9th – 12th Grade Students Reporting Lifetime Injection Drug Use (IDU) from 1999 to 2017 in 9 Urban Centers
| New York City, NY | Broward County, FL | Orange County, FL | Miami-Dade County, FL | Dallas, TX | Chicago, IL | Milwaukee, WI | San Bernardino, CA | San Diego, CA | |
|---|---|---|---|---|---|---|---|---|---|
| All Years | 1.90 (1.73, 2.09) | 2.33 (2.03, 2.67) | 2.46 (2.17, 2.79) | 2.46 (2.20, 2.75) | 1.85 (1.54, 2.21) | 2.66 (2.32, 3.05) | -- | 2.31 (1.97, 2.70) | 2.13 (1.91, 2.37) |
| 1999 | 0.84 (0.53, 1.32) | 1.78 (1.15, 2.74) | -- | 2.65 (1.77, 3.96) | 1.08 (0.65, 1.78) | 2.53 (1.43, 4.45) | -- | -- | 1.46 (0.91, 2.35) |
| 2001 | 1.07 (0.64, 1.79) | 2.94 (1.90, 4.52) | 2.17 (0.93, 5.01) | 1.63 (1.14, 2.32) | 1.82 (1.22, 2.79) | 2.18 (1.32, 3.59) | -- | 2.48 (1.33, 4.54) | 1.79 (1.16, 2.74) |
| 2003 | 1.27 (0.99, 1.62) | 1.74 (1.06, 2.84) | 1.56 (0.91, 2.68) | 1.60 (1.09, 2.34) | 2.15 (1.55, 2.99) | 1.49 (0.88, 2.50) | -- | 3.01 (2.11, 4.28) | 2.39 (1.55, 3.65) |
| 2005 | 2.10 (1.56, 2.82) | 2.26 (1.39, 3.65) | 2.29 (1.50, 3.49) | 1.76 (1.22, 2.54) | 1.86 (1.11, 3.09) | 2.01 (0.84, 4.74) | -- | 3.70 (2.50, 5.46) | 2.33 (1.65, 3.28) |
| 2007 | 1.69 (1.28, 2.23) | 2.09 (1.11, 3.89) | 2.29 (1.43, 3.64) | 2.99 (2.31, 3.85) | 3.57 (2.18, 5.78) | 2.35 (1.45, 3.80) | -- | 1.80 (1.10, 2.94) | 3.04 (2.12, 4.33) |
| 2009 | 2.77 (2.35, 3.26) | 3.77 (2.35, 6.01) | 2.44 (1.57, 3.76) | 3.87 (2.83, 5.27) | 1.89 (1.28, 2.79) | 3.77 (2.64, 5.37) | -- | 1.93 (1.21, 3.05) | 1.82 (1.23, 2.69) |
| 2011 | 2.47 (1.93, 3.15) | 1.41 (0.74, 2.67) | 2.32 (1.47, 3.65) | 3.70 (2.76, 4.95) | 1.03 (0.60, 1.77) | 3.36 (2.66, 4.23) | -- | 1.70 (1.01, 2.85) | 2.89 (2.13, 3.92) |
| 2013 | 2.47 (1.92, 3.19) | 2.17 (1.27, 3.70 | 2.02 (1.37, 2.98) | 1.61 (1.06, 2.45) | -- | 2.56 (1.58, 4.11) | -- | 1.85 (1.12, 3.06) | 2.07 (1.23, 3.45) |
| 2015 | 2.24 (1.71, 2.95) | 3.05 (2.12, 4.36) | 3.31 (1.83, 5.91) | 2.43 (1.66, 3.53) | -- | -- | -- | -- | 2.06 (1.45, 2.92) |
| 2017 | 2.74 (2.18, 3.45) | 2.00 (1.01, 3.94) | 3.47 (2.32, 5.15) | 3.91 (2.88, 5.29) | -- | 4.12 (2.50, 6.73) | -- | -- | 1.42 (0.95, 2.11) |
| Linear β (p-value) | 0.34 (<0.0001) | 0.02 (0.76) | 0.17 (0.02) | 0.16 (0.01) | 0.06 (0.43) | 0.03a (0.64) | -- | −0.20 (0.05) | −0.001 (0.99) |
| Quadratic β (p-value) | −0.06 (0.20) | −0.02 (0.85) | 0.06 (0.36) | 0.03 (0.56) | −0.16 (0.02) | 0.17a (0.05) | -- | −0.03 (0.78) | −0.12 (0.04) |
Note. Bold indicates statistical significance (p ≤ 0.05). A double dash indicates that the data were not available for the year.
Trend for Chicago, IL does not include 2017 (see Methods).
Discussion
This study assessed trends in heroin and IDU among adolescents using data from urban across the country, providing an important first step towards understanding local variation in substance use in the context of the ongoing opioid crisis. We identified increases in heroin use over time in New York, Chicago, and Milwaukee, and increases in IDU in New York, Orange County, and Miami-Dade County. San Bernardino was the only locality with a decrease over time in both heroin and injection drug use. These findings suggest that the prevalence of heroin use and IDU among adolescents is increasing in some urban centers of the US. Moreover, in all nine urban centers we found that patterns of heroin use and IDU mirrored each other and moved together over time. Although more research is needed, this suggests that heroin use may account for a large portion of all injection drug use among adolescents.
There are several city-level risk factors that could contribute to an explanation of disparities in prevalence, such as historical differences in endemic heroin issues, drug availability, norms and attitudes around drug use, and other secular trends. While investigating such explanations is beyond the scope of this study, future research should explore how these different factors have contributed to emerging trends in adolescent heroin use so that we can develop effective public health interventions. With that said, we did attempt to understand why San Bernardino, CA was the only district that had decreases in both heroin and IDU. There were no significant changes in sample size between years in this city. Furthermore, state policy explanations, such as the legalization of cannabis, cannot account for these findings, especially because San Diego would have also been affected by California state laws. There was no clear explanation available in our data for these trends, so future research is needed to understand this phenomenon. However, our results from 2001 to 2013, are consistent with current trends in San Bernardino County from 2014 to 2016. In contrast with the rest of the state of California, San Bernardino experienced decreases in heroin-related emergency department (ED) visits [35]. Health experts in San Bernardino county believe the increase in prescription opioid misuse has led to more young people using heroin and have implemented taskforces to prevent opioid overdose. However, health officials cannot explain why San Bernardino experienced a decrease in ED visits, compared to remaining counties that have implemented similar efforts [35,36]. Understanding what has been effective in curbing adolescent heroin and inject drug use in San Bernardino could provide key insights into interventions that may be effective elsewhere.
Contextualizing these findings with the current literature, although limited, is important. Compared to a recent study examining local trends in injection drug use using YRBS data our study also found a significant increase in injection drug use in New York City and Miami-Dade, FL [28]. While this study only examined IDU trends, our study extends these findings by revealing the overlap between injection drug use and heroin use in these two urban centers. A key finding of this study is the observation that adolescent heroin and IDU trends overlap and follow a similar pattern over time. While the YRBS question on IDU does not ask about the specific drug used, our results strengthen the hypothesis that many adolescents that use heroin are injecting it. Indeed, the Monitoring the Future survey found that 66% of twelfth grade who used heroin reported injecting it with a needle [10]. Descriptive studies confirm that white race, parental drug use, and witnessing peers inject heroin are significantly associated with transition to IDU, and youth are more likely to report poor health status and drop out of school following this shift [15,20]. While establishing risk factors of adolescent IDU is critical, additional research should determine the prevalence of injection and non-injection routes of heroin use among subgroups of adolescents. Because the MTF survey does not collect local data for adolescent substance use, we cannot directly compare our estimates. However, according to the 2018 MTF survey, trends of heroin use by injection peaked at 1.8% in 2000 and have declined steadily among all students to 0.4% in 2018. On the other hand, the MTF reports overall heroin use has been declining since 2010, reaching its lowest levels in 2016 (0.6%) and remaining stable since [37]. This prevalence is lower than the 1.7% obtained from the 2017 National YRBS. This is because the YRBS obtains higher estimates than MTF for 10th and 12th graders, making their point estimates higher, but findings across both surveys are similar when comparing and identifying subgroups with higher risk profiles [38].
The results of this study should be considered in light of a few limitations. We were unable to include NMPO use in this analysis because no large-scale adolescent surveillance survey collected this information at the local level prior to 2017, when the YRBS added a question on pain medications. Although this study is unable to comment on potential relationships between prescription opioids, heroin, and IDU among adolescents, there is data describing that adolescents may transition from NMPO to heroin use and IDU [8,9,11,12]. Additionally, because the behaviors in question are highly stigmatized and local datasets may have less observations than national-level datasets, insufficient sample size and conservative response bias may contribute to concern about the precision of estimates. Because the YRBS is administered in schools, students who are absent, truant, or who have dropped out are likely to be missed; these youth have the highest risk of heroin and IDU initiation. Therefore, our results probably underestimate the true prevalence of adolescent heroin use and IDU. Nonetheless, our study is an important first step in understanding local variations in trends in adolescent heroin and injection drug use.
In conclusion, our study highlights two key findings and implications for future research. First, there is a clear need to consider local data in evaluation of adolescent substance use trends, especially in the context of the ongoing opioid epidemic. Researchers should devote additional attention to localities and geographic regions that may have an endemic heroin problem. Second, we need to collect additional surveillance data on adolescent opioid use, including route of administration, to fully understand regional nuances and effectively implement public health solutions. Future research should continue to address local variation in adolescent drug use to fill the existing surveillance gap. More extensive surveillance will help public health practitioners better understand the epidemiology of opioid use among adolescents and make informed program and policy decisions to promote health and wellbeing.
Supplementary Material
Implications and Contribution.
In contrast to low and stable national trends, this study identified increases in heroin and injection drug use among 9th-12th graders in some urban centers. Findings highlight the importance of understanding local variation in adolescent drug use to effectively combat the ongoing opioid epidemic through public health programming.
Role of Funding Source:
This research was supported by grants from the National Institutes of Health (K01DA031738l, RM Johnson; T32DA007292, Brighthaupt, JK Johnson, Schneider, Jones). The content is solely the responsibility of the authors and does not necessarily reflect the official views of the NIH. The study sponsor had no role in determining study design; data collection, analysis, or interpretation; writing the report; or the decision to submit the report for publication.
Abbreviations:
- IDU
Injection Drug Use
- YRBS
Youth Risk Behavior Survey
- NMPO
Non-Medical Prescription Opioid Use
- MTF
Monitoring the Future
- CDC
Centers for Disease Control and Prevention
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure of financial conflicts of interest:
No financial disclosures were reported by authors of this paper.
Conflict of interest statement:
The authors would like to declare two potential conflicts of interest. Dr. Julie K. Johnson has worked as Director of Research at Massachusetts Cannabis Control Commission since April 17, 2018, which administers the laws enabling access to medical and adult use cannabis use in the state. Dr. Abenaa A. Jones’ spouse, Will Jones, works for Smart Approaches to Marijuana, which seeks “to educate citizens on the science of marijuana and to promote health-first, smart policies and attitudes that decrease marijuana use and its consequences.” Mr. Jones did not play a role in this study.
References
- [1].Mars SG, Bourgois P, Karandinos G, et al. “Every ‘Never’ I Ever Said Came True”: Transitions from opioid pills to heroin injecting. Int J Drug Policy 2014;25:257–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Votaw VR, Wittenauer J, Connery HS, et al. Perceived risk of heroin use among nonmedical prescription opioid users. Addict Behav 2017;65:218–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hedegaard H, Chen L-H, Warner M. Drug Poisoning Deaths Involving Heroin: United States, 2000–2013. Hyattsville, MD: 2015. [PubMed] [Google Scholar]
- [4].Scholl L, Seth P, Kariisa M, et al. Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2018;67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. MMWR Morb Mortal Wkly Rep 2015;64:453–8. [PMC free article] [PubMed] [Google Scholar]
- [6].Cicero TJ, Ellis MS, Surratt HL, et al. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry 2014;71:821–6. [DOI] [PubMed] [Google Scholar]
- [7].Martins SS, Sarvet A, Santaella-Tenorio J, et al. Changes in US Lifetime Heroin Use and Heroin Use Disorder. JAMA Psychiatry 2017;74:445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Palamar JJ, Shearston JA, Dawson EW, et al. Nonmedical opioid use and heroin use in a nationally representative sample of us high school seniors. Drug Alcohol Depend 2016;158:132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cerdá M, Santaella J, Marshall BDL, et al. Nonmedical Prescription Opioid Use in Childhood and Early Adolescence Predicts Transitions to Heroin Use in Young Adulthood: A National Study. J Pediatr 2015;167:605–12.e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Miech RA, Johnston LD, O’malley PM, et al. Monitoring the Future: National Survey Results on Drug use, 1975–2017: Volume 1, Secondary School Students. vol. 1 Ann Arbor: 2018. [Google Scholar]
- [11].Palamar JJ, Le A, Mateu-Gelabert P. Not just heroin: Extensive polysubstance use among US high school seniors who currently use heroin. Drug Alcohol Depend 2018;188:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Veliz P, Boyd CJ, McCabe SE. Nonmedical Use of Prescription Opioids and Heroin Use Among Adolescents Involved in Competitive Sports. J Adolesc Heal 2017;60:346–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance — United States, 2015. Morb Mortal Wkly Rep 2016;65:1–180. [DOI] [PubMed] [Google Scholar]
- [14].Gandhi DH, Kavanagh GJ, Jaffe JH. Young Heroin Users in Baltimore: A Qualitative Study. Am J Drug Alcohol Abuse 2006;32:177–88. [DOI] [PubMed] [Google Scholar]
- [15].Sherman SG, Fuller CM, Shah N, et al. Correlates of Initiation of Injection Drug Use Among Young Drug Users. J Psychoactive Drugs 2005;37:437–43. [DOI] [PubMed] [Google Scholar]
- [16].DuPont RL. Profile of a Heroin-Addiction Epidemic. N Engl J Med 1971;285:320–4. [DOI] [PubMed] [Google Scholar]
- [17].Garfield J, Drucker E. Fatal Overdose Trends in Major US Cities. Addict Res Theory 2001;9:425–36. [Google Scholar]
- [18].Curtin SC, Tejada-Vera B, Warner M. Drug Overdose Deaths Among Adolescents Aged 15–19 in the United States, 1999–2015. NCHS Data Brief 2017:1–6. [PubMed] [Google Scholar]
- [19].Lankenau SE, Teti M, Silva K, et al. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy 2012;23:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Subramaniam GA, Stitzer MA. Clinical Characteristics of Treatment-Seeking Prescription Opioid versus Heroin using Adolescents with Opioid Use Disorder. Drug Alcohol Depend 2009;101:13–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Vaughn MG, Salas-Wright CP, Oh S. Trends in heroin access among adolescents in the United States, 2002–2014. Prev Med (Baltim) 2017;99:67–8. [DOI] [PubMed] [Google Scholar]
- [22].Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban-rural status and by drug type. Pharmacoepidemiol Drug Saf 2008;17:997–1005. [DOI] [PubMed] [Google Scholar]
- [23].Keyes KM, Cerdá M, Brady JE, et al. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health 2014;104:e52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Fuller CM, Vlahov D, Ompad DC, et al. High-risk behaviors associated with transition from illicit non-injection to injection drug use among adolescent and young adult drug users: a case-control study. Drug Alcohol Depend 2002;66:189–98. [DOI] [PubMed] [Google Scholar]
- [25].Hadland SE, Wood E, Nosova E, et al. Cessation of Injecting and Preceding Drug Use Patterns Among a Prospective Cohort of Street-Involved Youth. J Adolesc Heal 2017;61:612–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Tuazon CU, Hill R, Sheagren JN. Microbiologic Study of Street Heroin and Injection Paraphernalia. J Infect Dis 1974;129:327–9. [DOI] [PubMed] [Google Scholar]
- [27].Del Giudice P Cutaneous complications of intravenous drug abuse. Br J Dermatol 2004;150:1–10. [DOI] [PubMed] [Google Scholar]
- [28].Klevens RM, Jones SE, Ward JW, et al. Trends in Injection Drug Use Among High School Students, U.S., 1995–2013. Am J Prev Med 2016;50:40–6. [DOI] [PubMed] [Google Scholar]
- [29].Centers for Disease Control and Prevention (CDC). High School Youth Risk Behavior Survey Data. Available at: https://www.cdc.gov/healthyyouth/data/yrbs/data.htm.
- [30].Brener ND, Kann L, Shanklin S, et al. Methodology of the Youth Risk Behavior Surveillance System - 2013. Morb Mortal Wkly Rep Reccomendations Reports 2013;62:1–20. [PubMed] [Google Scholar]
- [31].Youth Risk Behavior Surveillance System. High School YRBS Participation History, Data Quality, and Data Availability. 2017.
- [32].StataCorp. Stata Statistical Software: Release 14 2017:319. [Google Scholar]
- [33].StataCorp. Stata 13 Survey Data Reference Manual. College Station, TX: Stata Press; 2013. [Google Scholar]
- [34].Bewick V, Cheek L, Ball J. Statistics review 9: One-way analysis of variance. Crit Care 2004;8:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Rokos B Is Inland area bucking statewide trend in heroin overdoses? San Bernardino Sun 2017. [Google Scholar]
- [36].Bharath D San Bernardino and Riverside counties sue drug companies, distributors and pharmacies over opioid epidemic. San Bernardino Sun 2018. [Google Scholar]
- [37].Johnston LD, Miech RA, O’Malley PM, et al. Monitoring the Future: National Survey Results on Drug use, 1975–2018: Overview - Key Findings on Adolescent Drug Use. Ann Arbor: 2018. [Google Scholar]
- [38].Substance Abuse and Mental Health Services Administration. Comparing and Evaluating Youth Substance Use Estimates from the National Survey on Drug Use and Health and Other Surveys. Rockville, MD: 2012. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.