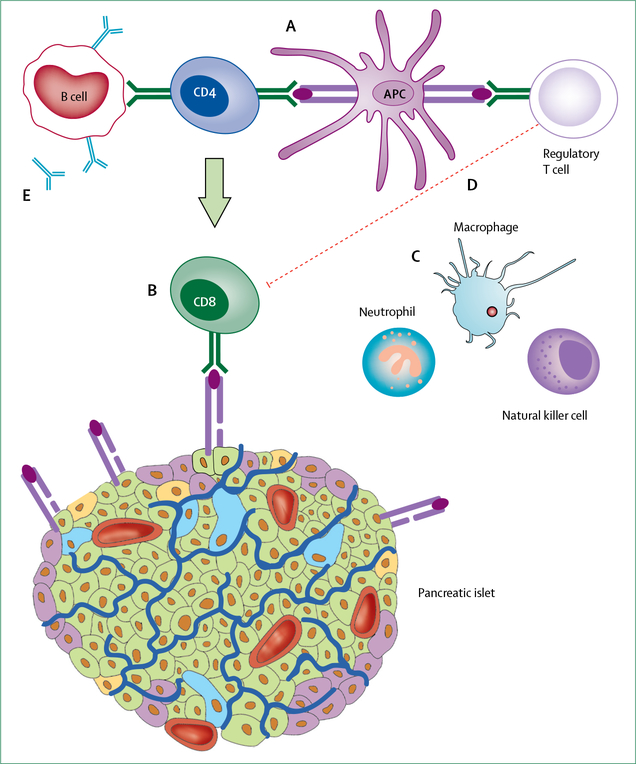
Figure 3: The immunopathogenesis of type 1 diabetes.
The development of type 1 diabetes is thought to be initiated by the presentation of β-cell peptides by antigen-presenting cell (APCs). APCs bearing these autoantigens migrate to the pancreatic lymph nodes where they interact with autoreactive CD4+ T lymphocytes, which in turn mediate the activation of autoreactive CD8+T cells (A). These activated CD8+ T cells return to the islet and lyse β cells expressing immunogenic self-antigens on major histocompatibility complex class I surface molecules (B). β-cell destruction is further exacerbated by the release of proinflammatory cytokines and reactive oxygen species from innate immune cells (macrophages, natural killer cells, and neutrophils; C). This entire process is amplified by defects in regulatory T lymphocytes, which do not effectively suppress autoimmunity (D). Activated T cells within the pancreatic lymph node also stimulate B lymphocytes to produce autoantibodies against β-cell proteins. These autoantibodies can be measured in circulation and are considered a defining biomarker of type 1 diabetes (E).