Abstract
Background
The incidence of atherosclerotic cardiovascular disease has declined in the past 2 decades. However, these benefits may not extend to young patients. The objective of this work was to assess temporal trends in the incidence, risk profiles, sex‐related differences, and outcomes in a contemporary population of young patients presenting with coronary artery disease (CAD) in British Columbia, Canada.
Methods and Results
We used a provincial cardiac registry to identify young patients (men aged <50 years, women aged <55 years), with a first presentation of CAD between 2000 and 2016, who had either ≥50% stenosis of ≥1 coronary arteries on angiography or underwent coronary revascularization. A total of 12 519 patients (30% women) met our inclusion criteria. The incidence of CAD remained stable and was higher for men than women (46–53 versus 18–23 per 100 000). Of patients, 92% had at least one traditional cardiovascular risk factor and 67% had multiple risk factors. The prevalence of diabetes mellitus, obesity, and hypertension increased during the study period and was higher for women. Women had fewer emergent procedures and revascularizations. Mortality rates decreased by 31% between 2000 and 2007, then were stable for the remaining 9 years. Mortality was significantly higher for women aged <45 years compared with men.
Conclusions
The incidence of premature CAD has not declined, and the prevalence of 3 major cardiovascular risk factors increased between 2000 and 2016. The risk burden and mortality rates were worse for women. These data have important implications for the design of strategies to prevent CAD in young adults.
Keywords: cardiovascular disease, cardiovascular disease risk factors, sex specific, trends, young
Subject Categories: Atherosclerosis, Coronary Artery Disease, Epidemiology, Risk Factors, Mortality/Survival
Clinical Perspective
What Is New?
In this study of a contemporary cohort of patients with angiographically proven premature coronary disease, the incidence rates of coronary artery disease in younger people have not declined as they have for older patients.
This trend is accompanied by increasing prevalence of important cardiovascular risk factors, such as hypertension, diabetes mellitus, and obesity.
After a notable initial improvement of mortality risk between 2000 and 2007, it remained unchanged for the following 9 years of the study period.
What Are the Clinical Implications?
Comprehensive and more effective strategies for screening and primordial and primary prevention of premature coronary artery disease are needed.
Clinical studies, developed specifically for patients with premature coronary artery disease, are needed to understand further the specific cardiovascular risk profile and to enhance risk‐estimation approaches for young adults.
Initiatives and campaigns, such as the World Heart Federation's “25 by 25” campaign, should be more actively promoted to raise awareness in the general public and medical community.
Introduction
Cardiovascular events and mortality have decreased in many countries over the past 2 decades.1, 2, 3, 4 However, this positive trend does not extend to all individuals. In particular, rates of cardiovascular events and mortality in young adults have decreased to a lesser extent or have remained unchanged.1, 5, 6, 7
Atherosclerotic cardiovascular disease (ASCVD) in young adults represents a specific and growing challenge. In the INTERHEART (Effect of Potentially Modifiable Risk Factors Associated With Myocardial Infarction in 52 Countries) study, 9 traditional cardiovascular risk factors accounted for 90% of the population‐attributable risk for myocardial infarction (MI) in men and 94% in women, with a larger impact on younger people (population‐attributable risks of 93% and 97%, for men aged ≤55 years and women aged ≤65 years, respectively).8 Young people, and especially young women, may be less aware of their underlying cardiovascular risk factors and are less likely to discuss lifestyle modification or primary prevention with their healthcare providers.1, 9, 10
The burden of ASCVD in young adults is an important public health issue because of potential loss of lifetime productivity and increased lifetime healthcare use. The emphasis on sex‐ and age‐specific approaches to ASCVD has resulted in the development of programs, campaigns, and guidelines targeting this issue. The 66th World Health Assembly introduced the World Health Organization Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013 to 2020 (resolution WHA66.10).11 Targets for 6 preventable risk factors (tobacco and alcohol use, salt intake, obesity, and elevated blood pressure and glucose) were established to reduce premature ASCVD mortality by 25% in 2025.12 The World Heart Federation joined this global “25 by 25” campaign. At the same time, large campaigns targeting cardiovascular health in women, such as Go Red for Women, were launched in many countries to address sex‐related disparities in prevention and treatment of ASCVD.
Despite this, there is limited information about the cardiovascular risk profiles, management, and sex‐related differences in younger patients with ASCVD and in particular coronary artery disease (CAD). In addition, the degree to which these recent public campaigns have positively addressed the problem of premature CAD is unclear.
The objectives of this study were as follows: (1) to evaluate changes in the incidence of premature CAD; (2) to characterize recent trends in the prevalence of modifiable major cardiovascular risk factors; (3) to examine and compare differences in risk profiles, clinical presentation, revascularization, and outcomes between young women and men with CAD; and (4) to identify predictors of mortality in young patients with a first presentation of CAD in the Canadian province of British Columbia (BC).
Methods
The study data used in this study can be requested by qualified researchers from Cardiac Services of BC (CSBC) ( http://www.cardiacbc.ca/contact).
Data Source/Study Period
We analyzed data from the CSBC Registry to identify young adults with a first presentation of CAD between January 1, 2000, and December 31, 2016. CSBC is an agency responsible for planning, coordinating, monitoring, and evaluating cardiac services across BC. The CSBC Registry is an electronic cardiac information system that collects clinical, procedural, and demographic information on patients who receive treatment at all 5 regional cardiac centers that deliver cardiac services in the province.13
Patients
Inclusion criteria
We included all young adults (men aged 19–50 years, women aged 19–55 years) with a first presentation of CAD, which we defined as at least one of the following: acute ST‐segment–elevation MI (STEMI), non‐ST‐segment‐elevation myocardial infarction (NSTEMI), or stable or unstable angina pectoris with angiographically proven coronary disease. We also included patients who initially had other indications for angiography but met the angiographic criteria of eligibility (namely, ≥50% luminal stenosis of ≥1 coronary arteries on diagnostic coronary angiography) or underwent percutaneous or surgical revascularization. The first diagnostic coronary angiography or percutaneous coronary intervention was considered as the index procedure. All patients had an index procedure between January 1, 2000, and December 31, 2016 (Figure 1). To ensure that trends in the indication for cardiac catheterization did not interfere with trends in risk profiles and mortality in our cohort, the proportion of patients with first presentation as an acute coronary syndrome, stable angina, or other conditions was calculated for every year within the study period (Table S1).
Figure 1.
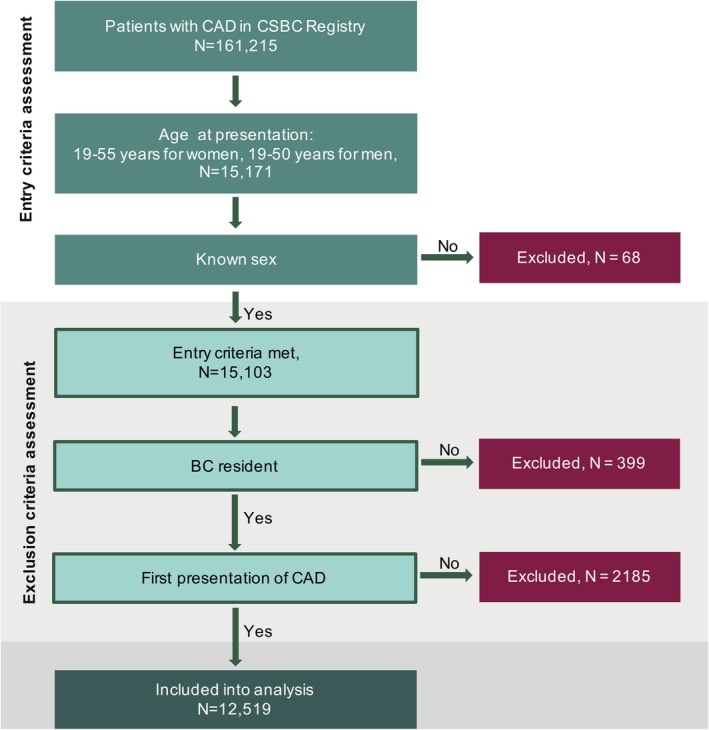
Patient flow through inclusion/exclusion procedure. Stepwise analysis of data provided by the CSBC (Cardiac Services of British Columbia) Registry to identify young adults with a first presentation of angiographically documented coronary artery disease (CAD) between January 1, 2000, and December 31, 2016, in British Columbia (BC), Canada.
Exclusion criteria
We excluded patients with a history of CAD, defined as prior MI, previous evidence of ≥50% luminal stenosis of ≥1 coronary arteries on diagnostic coronary angiography, or prior coronary revascularization. Patients who were not BC residents or for whom sex was unknown were also excluded.
Variables
Cardiovascular risk factors, comorbidities, and clinical presentation
Dyslipidemia, hypertension, and diabetes mellitus were considered present if these conditions were self‐reported by the patient before the index procedure and recorded in CSBC Registry; if they were previously diagnosed by a physician, according to medical records; or if the patient was undergoing treatment with antihypertensive, antidiabetic, or cholesterol‐lowering medications. Smoking status was determined from the patient's self‐reported status. Obesity, defined as having a body mass index ≥30 kg/m2, was determined according to height and weight recorded at the time of the index procedure. The presence of additional comorbidities was assessed from patients’ medical records and CSBC Registry. Symptoms at presentation, diagnosis, and indications for the index procedure were assessed and recorded by cardiologists in cardiac centers before the index procedure. Acute coronary syndrome by clinical manifestation (NSTEMI, STEMI, and unstable angina) was only available in patients with an index procedure from 2012 to 2016 (n=3154).
Extent of CAD, procedural variables, and mortality
The extent of CAD was determined by angiographic findings during the index procedure. Urgency at procedure was defined as follows: emergent (must be done without delay), urgent (done before hospital discharge), or elective (next available time). Data on all‐cause mortality were available between January 1, 2000, and December 31, 2016, and were obtained through linkage with vital statistics.
Ethics
The study was approved by the University of BC Research Ethics Board. Informed consent was not required as data were anonymized by data stewards, CSBC.
Statistical Analysis
Baseline characteristics and indications for index procedure, procedural variables, and clinical characteristics at presentation were summarized as frequencies and percentages or medians and first and third quartiles for categorical and continuous variables, respectively. To test for sex differences, the χ2 and Wilcoxon sum‐rank tests were conducted for categorical and continuous variables, respectively.
To account for changes in the age and sex of the underlying population over the 16‐year time frame of this study, direct standardization method was used to calculate age‐standardized incidence rates of CAD, by sex and by age group (19–40, 41–45, 46–50, and 51–55 years). All rates were standardized to the year 2016, of the BC population obtained from Statistics Canada population life tables.14
Temporal trends in each of the 5 key cardiovascular risk factors (obesity, diabetes mellitus, hypertension, hyperlipidemia, and current smoking) were assessed using the logistic regression model with year fitted as a linear covariate. To allow for different trend by sex, each model was adjusted for an interaction term between sex and year. All models were also adjusted for age. Patients were also summarized according to the number of key cardiovascular risk factors present (range, 0–5) using counts and percentages, stratified by sex and age group. The average number of risk factors per patient was plotted by sex at each year, with the trend illustrated using the “loess” smoothing method.
Unadjusted mortality rates with standard errors, by sex, were estimated for 30 days and 1, 3, 5, and 10 years using the Kaplan‐Meier method. Mortality rates were also estimated by sex for each age group and compared using the log‐rank test (with the exception of the 51–55 years of age curve, which was only done for women).
Factors associated with mortality were assessed using multivariable Cox regression analysis. Selection of predictors was conducted using the backward stepwise approach. Predictors with P≤0.1 were retained in the final model. The following 23 covariates were considered for selection: sex, age, procedure year, health authority, body mass index, smoking (never/former/current), comorbidities (heart failure, hypertension, hyperlipidemia, diabetes mellitus, peripheral vascular disease, cerebrovascular, liver/gastrointestinal tract disease, renal insufficiency, chronic lung disease, and malignancy), extent of CAD (<2, 2, and 3 vessels, including the left main coronary artery), urgency, ejection fraction (>50% and ≤50%), revascularization, and complicating factors (heart failure, hemodynamic instability, and cardiogenic shock). Revascularization, either at or after the index procedure, was modeled as a time‐dependent covariate. Four covariates were eliminated by the backward stepwise selection process: health authority, body mass index, urgency, and heart failure. The final model included sex regardless of its statistical significance because of its clinical significance in the context of the mortality outcome. The analysis was performed for all patients, and the same model was also fitted separately for female and male cohorts. Interaction between age and sex was tested on the basis of all patients. Proportional hazards assumption was tested using the Schoenfeld residuals. Estimated hazard ratios and 95% CIs were reported for the predictors for all 3 models. All analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC). Figures were generated using RStudio, version 1.1.383.15
Results
Participants
We identified 15 171 young adults with a first presentation of CAD between 2000 and 2016. We excluded 2185 patients from the study because of a history of CAD, 68 because of missing information about sex, and 399 who were not residents of BC (Figure 1). In total, 12 519 patients were included in the analysis (30.4% women). The demographics, cardiovascular risk factors, and other comorbidities are shown in Table 1.
Table 1.
Baseline Characteristics of Young Patients (Men Aged <50 Years, Women Aged <55 Years) With First Presentation of CAD, 2000 to 2016
| Characteristics | Women (N=3811) | Men (N=8708) | P Value |
|---|---|---|---|
| Age group, y | |||
| 19–40 | 220 (5.8) | 1140 (13.1) | 0.155a |
| 41–45 | 537 (14.1) | 2349 (27.0) | |
| 46–50 | 1139 (29.9) | 5219 (59.9) | |
| 51–55 | 1915 (50.2) | … | |
| Diabetes mellitus | 992 (26.0) | 1352 (15.5) | <0.001 |
| Hyperlipidemia | 1732 (45.4) | 4160 (47.8) | 0.016 |
| Hypertension | 1855 (48.7) | 3465 (39.8) | <0.001 |
| Obesityb | 1499 (39.3) | 3102 (35.6) | <0.0001 |
| Smokingc | |||
| Current | 1579 (43.5) | 3565 (43.2) | 0.642 |
| Former | 811 (22.4) | 1803 (21.9) | |
| Never | 1236 (34.1) | 2882 (34.9) | |
| Heart failure | 123 (3.2) | 189 (2.2) | <0.001 |
| Peripheral vascular disease | 214 (5.6) | 190 (2.2) | <0.001 |
| Cerebrovascular disease | 128 (3.4) | 143 (1.6) | <0.001 |
| Liver/gastrointestinal tract disease | 276 (7.2) | 465 (5.3) | <0.001 |
| Renal insufficiency | 429 (11.3) | 501 (5.8) | <0.001 |
| Chronic lung disease | 364 (9.6) | 448 (5.1) | <0.001 |
| Malignancy | 175 (4.6) | 113 (1.3) | <0.001 |
Data are given as number (percentage). BMI indicates body mass index; CAD, coronary artery disease.
The P value is based on a comparison that excludes the age group of 51 to 55 years.
A total of 304 were missing.
b643 were missing.
Incidence Rate of ASCVD
The age‐standardized rate of the first presentation with CAD was stable for both sexes over the entire observation period. The incidence was greater for men (46–53 per 100 000) than women (18–23 per 100 000) overall and in all age groups (Figure 2A and 2B).
Figure 2.
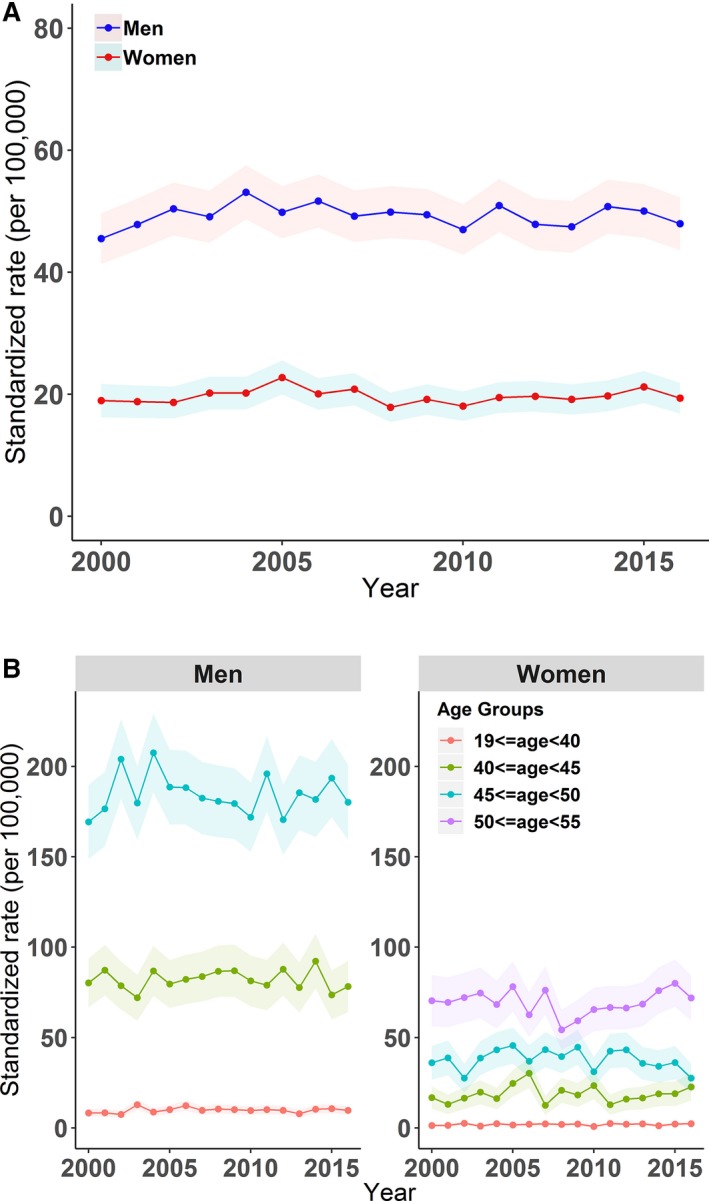
The age‐standardized incidence rate with 95% CI of premature coronary artery disease (CAD) by sex (A) and by sex and age group (B). The incidence rates of premature CAD were stable for both sexes during the observed period. The incidence rate was greater for men than women in all age groups.
Cardiovascular Risk Factors
Prevalence
A total of 92.4% of patients had at least one potentially modifiable cardiovascular risk factor. Hyperlipidemia was the most common risk factor (47.1% overall) and was more common among men (45.4% in women versus 47.8% in men; P<0.001) (Table 1). Hypertension was present in 42.5% of patients and was more common in women (48.7% in women versus 39.8% in men; P<0.001). A total of 43.3% of patients were current smokers and 22.0% were former smokers, which was similar in women and men. Obesity was present in 36.8% of patients, more often among women (39.3% in women versus 35.6% in men; P<0.0001). Diabetes mellitus was the least common risk factor (18.7% overall), and it was significantly more common in women (26.0% in women versus 15.5% in men; P<0.001).
Temporal Trends
The prevalence of hyperlipidemia and smoking decreased over the 17 years of the study period. After adjusting for age, the odds for having hyperlipidemia decreased by 3.1% (95% CI, 2.2%–3.9%) per year for men, and at a slightly higher rate for women (4.8% [95% CI, 3.9%–6.1%]; P=0.03 for interaction). The odds for current smoking declined in both sexes (1.9% [95% CI, 1.0%–2.7%] per year for men and 1.1% [95% CI, 0.3%–2.4%] per years for women; P=0.36 for interaction) (Figure 3).
Figure 3.
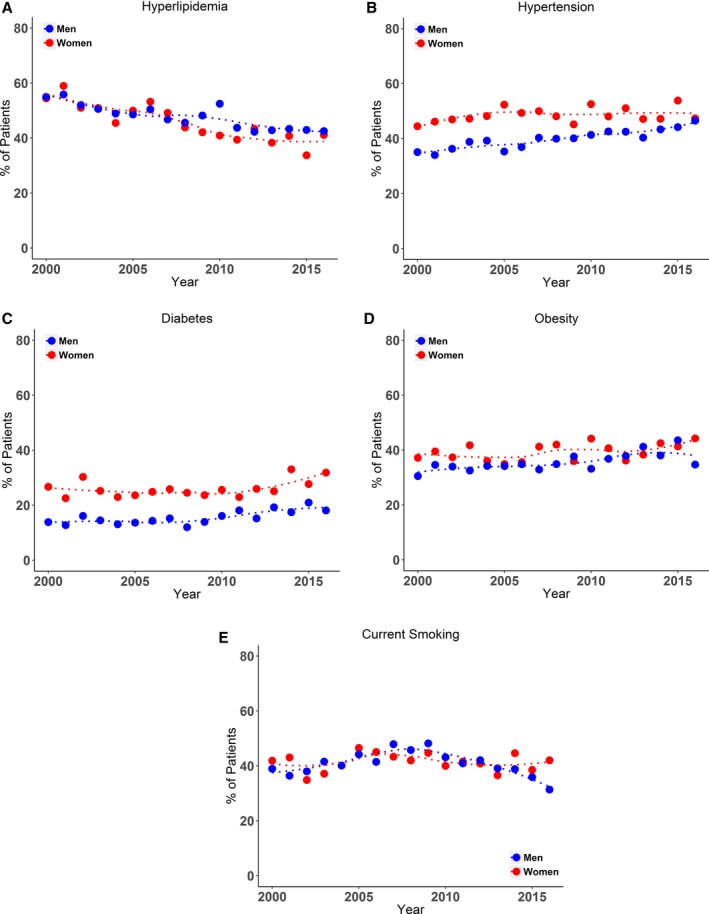
Temporal trends for key cardiovascular risk factors by sex, 2000 to 2016: hyperlipidemia (A), hypertension (B), diabetes mellitus (C), obesity (D), and current smoking (E). The prevalence decreased for hyperlipidemia and smoking and increased for hypertension, diabetes mellitus, and obesity over the 17 years of the study period.
In contrast, the prevalence of 3 risk factors increased significantly: for diabetes mellitus, the odds increased in both sexes (2.8% [95% CI, 1.6%–4.1%] per year for men and 1.4% [95% CI, 0.1%–2.9%] per year for women; P=0.16 for interaction); for obesity, the odds also increased in both sexes (1.4% [95% CI, 0.5%–2.4%] per year for men and 0.7% [95% CI, 0.6%–2.1%] per years for women; P=0.40 for interaction); and for hypertension, the odds increased more in men (2.7% [95% CI, 1.7%–3.6%] per year) compared with women (0.6% [95% CI, 0.7%–1.9%] per year; P=0.013 for interaction).
Cumulative Burden
Many patients had multiple cardiovascular risk factors: 29.8% had 2, 21.9% had 3, 11.7% had 4, and 3.4% had 5 cardiovascular risk factors. The distribution risk factor burden is shown in Figure 4. The numbers of risk factors varied by age, with less of a risk factor burden observed in the youngest group. In addition, women had a higher number of risk factors per person per year during the entire study period (Figure 5).
Figure 4.
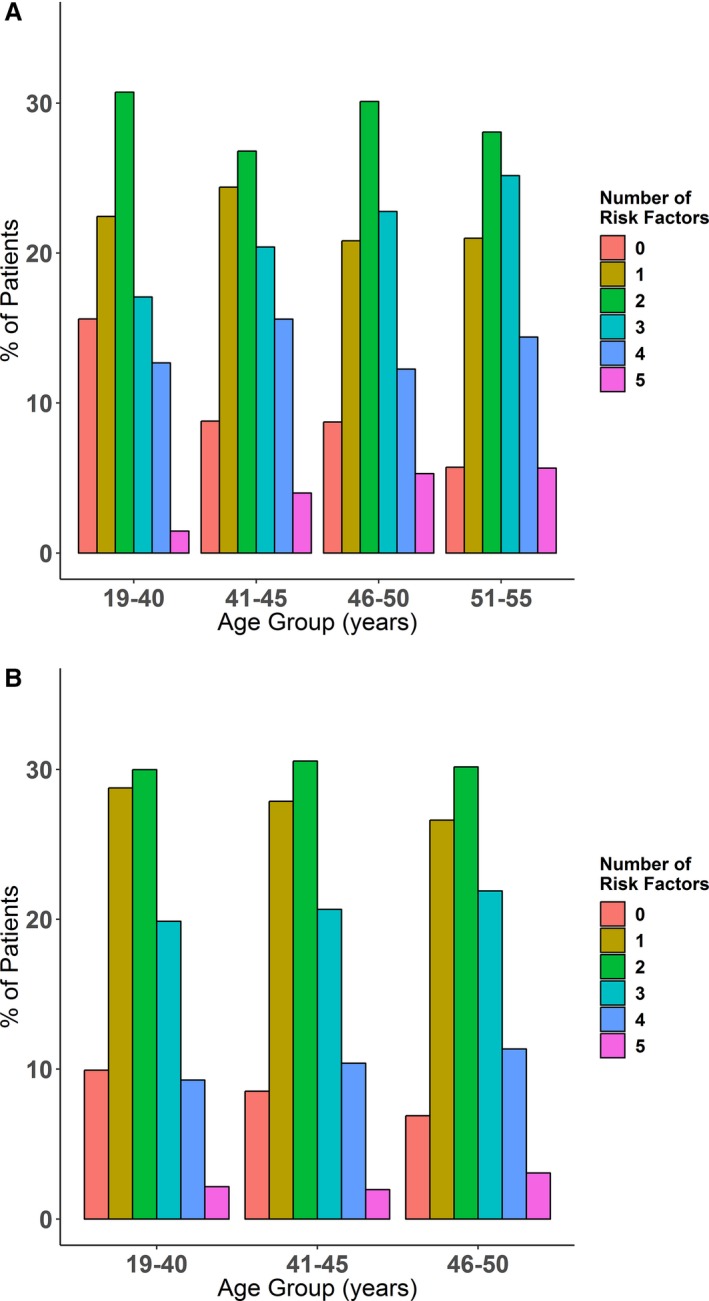
The prevalence of multiple risk factors by age group, for women (A) and men (B). The proportion of patients with 0, 1, 2, 3, 4, or 5 baseline comorbidities among young patients (men aged <50 years, women aged <55 years) with a first presentation of coronary artery disease.
Figure 5.
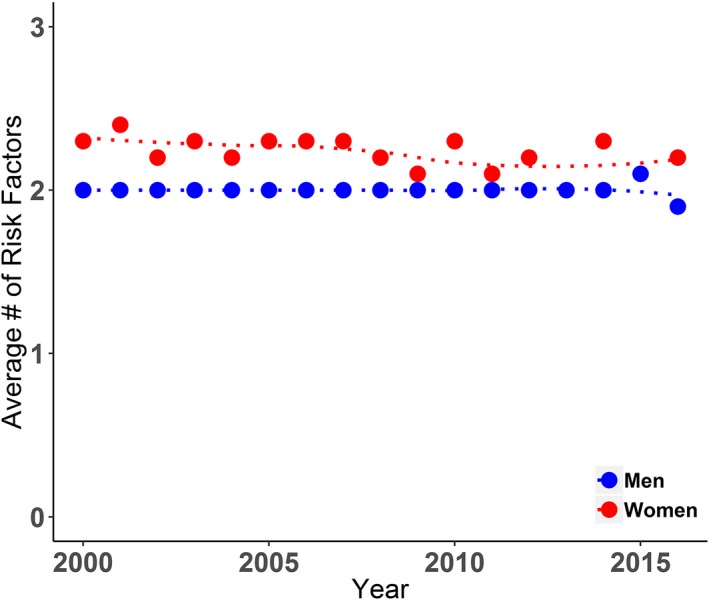
Temporal trends in average risk burden. The average number of risk factors per person per year among young patients (men aged <50 years, women aged <55 years) with a first presentation of coronary artery disease, by sex.
Clinical Presentation, Coronary Angiography, and Revascularization
Most patients, 74.4% (71.7% women versus 75.6% men; P<0.001), presented with an acute coronary syndrome. Of the subgroup of patients for whom information on clinical manifestation was available (n=3154), 49.1% had NSTEMI (51.5% of women versus 48.0% of men), 41.3% had STEMI (37.5% of women versus 43.1% of men), and 9.6% presented with unstable angina (11.0% of women versus 8.9% of men) (P=0.023). Women more often had atypical symptoms at presentation (4.1% of women versus 2.5% of men) (Table 2).
Table 2.
Indications for Index Procedure, Procedure Variables, and Clinical Characteristics at Presentation of Young Patients (Men Aged <50 Years, Women Aged <55 Years) With First Presentation of ASCVD, 2000 to 2016
| Variables | Women (N=3811) | Men (N=8708) | P Value |
|---|---|---|---|
| Indicationa | <0.001 | ||
| Acute coronary syndrome | 2727 (71.7) | 6574 (75.6) | |
| Stable angina | 832 (21.9) | 1654 (19.0) | |
| Otherb | 246 (6.5) | 464 (5.3) | |
| Acute coronary syndromes by clinical manifestationc | 0.023 | ||
| NSTEMI | 388 (51.5) | 789 (48.0) | |
| STEMI | 283 (37.5) | 708 (43.1) | |
| Unstable angina | 83 (11.0) | 146 (8.9) | |
| Procedure type | <0.001 | ||
| Coronary angiography and PCI | 2130 (55.9) | 5637 (64.7) | |
| Coronary angiography only | 1681 (44.1) | 3071 (35.3) | |
| Urgency scale at procedured | |||
| Elective | 904 (23.8) | 1722 (19.8) | <0.001 |
| Emergency | 754 (19.8) | 2165 (24.9) | |
| Urgent | 2141 (56.4) | 4797 (55.2) | |
| Ejection fraction, %e | <0.001 | ||
| ≤50 | 858 (25.6) | 2352 (30.3) | |
| >50 | 2492 (74.4) | 5419 (69.7) | |
| CCS class at presentationf | <0.001 | ||
| 0 | 137 (4.1) | 296 (3.8) | |
| I | 96 (2.9) | 233 (3.0) | |
| II | 392 (11.7) | 810 (10.5) | |
| III | 179 (5.3) | 345 (4.5) | |
| IVa | 1808 (53.8) | 4114 (53.4) | |
| IVb | 397 (11.8) | 1064 (13.8) | |
| IVc | 213 (6.3) | 644 (8.4) | |
| Atypical | 138 (4.1) | 195 (2.5) | |
| Extent of CADg | <0.0001 | ||
| <2 Vessels with >50% stenosis | 2163 (56.8) | 4190 (48.1) | |
| ≥2 Vessels with >50% stenosis | 1447 (38.0) | 4182 (48.0) | |
Data are given as number (percentage). ASCVD indicates atherosclerotic cardiovascular disease; CAD, coronary artery disease; CCS, Canadian Cardiovascular Society grading of angina pectoris; NSTEMI, non‐ST‐segment‐elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST‐segment–elevation myocardial infarction.
A total of 22 were missing.
Including cardiomyopathy, congestive heart failure, nonischemic cardiomyopathy, post–heart transplant workup, pulmonary hypertension, serious arrhythmia, valvular heart disease, and other.
Only available in patients with index procedure in 2012 to 2016 (N=3154).
A total of 36 missing.
A total of 1398 were missing.
A total of 1458 were missing.
A total of 3 were missing.
Men had a greater extent of CAD, with 48.0% of men versus 38.0% of women having ≥2 vessels with >50% stenosis. Women less frequently underwent emergent procedures (19.8% of women versus 24.9% of men) and were less likely to undergo percutaneous coronary intervention at the index procedure (55.9% of women versus 64.7% of men).
Mortality Rates and Temporal Trends
Of patients, 8% (10.3% of women and 7.1% of men) died during the study period. The all‐cause mortality rates were higher for women at 1, 3, 5, and 10 years of follow‐up (Table 3, Figure 6A). When analyzed by age‐sex groups, we observed significantly higher mortality for women in the age groups of 19 to 40 and 41 to 45 years, but not in the age group of 46 to 50 years (Figure 6B).
Table 3.
Rates of Short‐Term (30 Days) and Long‐Term (1, 3, 5, and 10 Years) Mortality With Standard Errors by Sex in Young Patients (Men Aged <50 Years, Women Aged <55 Years) With First Presentation of CAD, 2000 to 2016
| Time | Women | Men |
|---|---|---|
| 30 d | 0.011 (0.0017) | 0.011 (0.0011) |
| 1 y | 0.024 (0.0025) | 0.017 (0.0014) |
| 3 y | 0.044 (0.0034) | 0.027 (0.0018) |
| 5 y | 0.062 (0.0042) | 0.040 (0.0022) |
| 10 y | 0.12 (0.0067) | 0.076 (0.0035) |
Data are given as mortality rate (standard errors). CAD indicates coronary artery disease.
Figure 6.
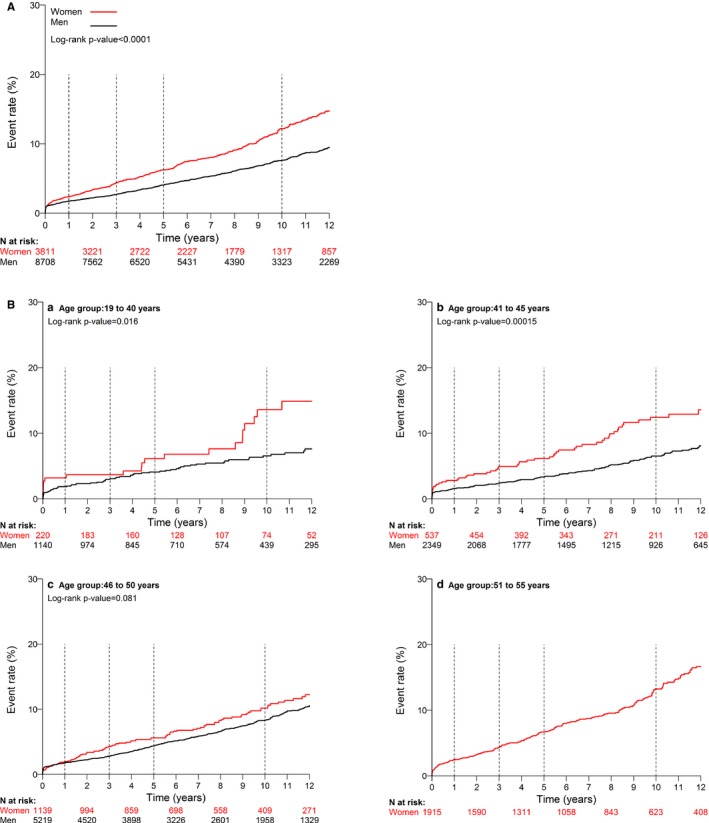
All‐cause mortality by sex (A) and by sex and age group (B). Kaplan‐Meier estimation of unadjusted mortality rates.
In multivariable Cox regression, hypertension, diabetes mellitus, current and former smoking, multivessel CAD, and accompanying cerebrovascular or peripheral vascular diseases predicted a higher mortality risk, whereas hyperlipidemia, revascularization, and baseline ejection fraction >50% reduced the risk of mortality (Table 4). After adjustment for these covariates, sex was not an independent predictor of mortality (adjusted hazard ratio [95% CI], 1.10 [0.95–1.27]).
Table 4.
Adjusted HRs and 95% CIs From Multivariable Cox Regression Model[Link] for All‐Cause Mortality Assessed for All Patients and Separately for Women and Men
| Characteristic | All Patients | Women | Men | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | |
| Sex: women vs men | 1.10 (0.95–1.27) | 0.209 | … | … | … | … |
| Age (per 5‐y increase) | 1.12 (1.04–1.20) | 0.002 | 1.09 (0.98–1.21) | 0.098 | 1.16 (1.05–1.27) | 0.004 |
| Year of the first presentation with CAD | ||||||
| 2004–2007 vs 2000–2003 | 0.69 (0.59–0.81) | <0.0001 | 0.68 (0.53–0.88) | 0.003 | 0.70 (0.57–0.86) | 0.001 |
| 2008–2011 vs 2000–2003 | 0.68 (0.56–0.83) | 0.0002 | 0.69 (0.50–0.95) | 0.021 | 0.68 (0.53–0.88) | 0.003 |
| 2012–2016 vs 2000–2003 | 0.68 (0.53–0.87) | 0.0021 | 0.71 (0.48–1.04) | 0.079 | 0.66 (0.48–0.91) | 0.012 |
| Hyperlipidemia | 0.72 (0.63–0.82) | <0.0001 | 0.77 (0.63–0.96) | 0.017 | 0.69 (0.58–0.81) | <0.0001 |
| Hypertension | 1.18 (1.03–1.36) | 0.015 | 1.20 (0.96–1.49) | 0.111 | 1.19 (1.00–1.42) | 0.046 |
| Diabetes mellitus | 1.79 (1.55–2.07) | <0.0001 | 1.97 (1.58–2.45) | <0.0001 | 1.67 (1.37–2.04) | <0.0001 |
| Smoking: current vs never | 1.99 (1.69–2.35) | <0.0001 | 1.85 (1.42–2.40) | <0.0001 | 2.11 (1.70–2.61) | <0.0001 |
| Smoking: former vs never | 1.25 (1.03–1.53) | 0.027 | 1.20 (0.87–1.64) | 0.269 | 1.30 (1.00–1.68) | 0.047 |
| Peripheral vascular disease | 1.87 (1.50–2.34) | <0.0001 | 1.98 (1.47–2.67) | <0.0001 | 1.74 (1.24–2.45) | 0.0013 |
| Cerebrovascular disease | 1.54 (1.17–2.04) | 0.0024 | 1.69 (1.14–2.50) | 0.009 | 1.41 (0.94–2.11) | 0.099 |
| Gastrointestinal tract and/or liver disease | 1.86 (1.51–2.29) | <0.0001 | 1.99 (1.45–2.75) | <0.0001 | 1.69 (1.27–2.24) | 0.0003 |
| Renal insufficiency | 1.88 (1.59–2.22) | <0.0001 | 1.66 (1.29–2.12) | <0.0001 | 2.14 (1.70–2.69) | <0.0001 |
| Chronic lung disease | 1.37 (1.11–1.69) | 0.0031 | 1.19 (0.88–1.60) | 0.257 | 1.66 (1.23–2.23) | 0.0008 |
| Malignancy | 1.90 (1.44–2.51) | <0.0001 | 1.54 (1.04–2.28) | 0.032 | 2.57 (1.73–3.82) | <0.0001 |
| Heart failure | 1.96 (1.55–2.48) | <0.0001 | 2.04 (1.43–2.91) | <0.0001 | 1.95 (1.42–2.67) | <0.0001 |
| Ejection fraction >50% vs ≤50%a | 0.53 (0.45–0.61) | <0.0001 | 0.47 (0.37–0.60) | <0.0001 | 0.57 (0.47–0.68) | <0.0001 |
| Hemodynamic instabilityb | 1.75 (1.08–2.83) | 0.024 | 2.29 (1.05–4.99) | 0.0036 | 1.54 (0.82–2.90) | 0.1833 |
| Cardiogenic shockb | 4.5 (2.84–7.15) | <0.0001 | 4.37 (2.05–9.30) | 0.0001 | 4.55 (2.49–8.30) | <0.0001 |
| CAD: 2 vs <2 vessels | 1.19 (1.01–1.40) | 0.034 | 1.25 (0.96–1.61) | 0.092 | 1.16 (0.94–1.43) | 0.1765 |
| CAD: 3c vs <2 vessels | 1.68 (1.44–1.96) | <0.0001 | 1.38 (1.05–1.79) | 0.019 | 1.87 (1.54–2.27) | <0.0001 |
| Revascularization | 0.57 (0.49–0.67) | <0.0001 | 0.64 (0.50–0.81) | 0.0002 | 0.54 (0.44–0.66) | <0.0001 |
All the covariates adjusted in the model are shown in the table. CAD indicates coronary artery disease; HR, hazard ratio.
All models exclude any patients with missing ejection fraction.
At presentation.
This category includes 3‐vessel disease and left main disease.
We assessed the effect of year of presentation on mortality. We observed a reduction in mortality rates in women (hazard ratio, 0.68; 95% CI, 0.53–0.88) and men (hazard ratio, 0.70; 95% CI, 0.57–0.86) with an index event in the period of 2004 to 2007 compared with the period of 2000 to 2003, without any significant further improvement for either sex in later periods. After an initial improvement with a risk reduction of 31.0% between 2000 and 2007, mortality remained unchanged for the remaining 9 years of the study period. However, because of the unequal follow‐up across these 4 time periods, the differences observed primarily reflect differences that occurred during the first few years of follow‐up.
Discussion
Using a provincial clinical cardiac registry, we investigated the incidence of angiographically documented premature CAD, as well as the prevalence, temporal patterns, and sex differences of cardiovascular risk factors, treatment, and outcomes in a cohort of patients with premature CAD. The study cohort included all patients in the province of BC who met the study criteria. Notable strengths of this study include the capture of all invasive cardiac procedures in the province over an extended period in a young population with a diagnosis of angiographically documented CAD. We did not identify a decline in the incidence of premature CAD in BC from 2000 to 2016, which is in notable contrast to the overall population of patients with ASCVD, among whom the age‐standardized rate of hospitalization for acute coronary events decreased from 264 to 247 per 100 000 in Canada and from 208 to 202 per 100 000 in BC between 2010 and 2016.16 We observed a high burden of potentially modifiable risk factors in this cohort with an increasing prevalence of diabetes mellitus, obesity, and hypertension over time. Finally, we found that after initial improvement between 2000 and 2007, mortality remained unchanged for the following 9 years of the study period, and both short‐ and long‐term mortality was greater in women than in men in this population.
Cardiovascular Risk Factors
One potential explanation for the steady incidence rate of CAD could be the high burden of cardiovascular risk factors in the study population, with 92% of patients having at least one recognized risk factor. The prevalence and cumulative burden of all risk factors in this cohort were higher than in the general Canadian population of the same age,17, 18, 19, 20, 21 and close to those observed previously in populations of patients with ASCVD with much higher mean age.8, 22, 23 In the INTERHEART study, 9 potentially modifiable cardiovascular risk factors accounted for >93% of the population‐attributable risk of MI in young patients.8 Consequently, some or much of the burden of premature ASCVD could be potentially prevented if these cardiovascular risk factors were identified early and effectively addressed. At the same time, young people, and especially women, are known to be less aware of their cardiovascular risk factors than older patients and less often discuss risk modification with healthcare providers.1, 9, 10
Trends in Cardiovascular Risk
A notable finding in our study was an increase in the prevalence of hypertension, diabetes mellitus, and obesity between 2000 and 2016. An increasing prevalence of these cardiovascular risk factors in young people was reported previously by Lee et al, who assessed data obtained from the general Canadian population between 1994 and 2005.24 A continuation of this trend indicates that more attention to cardiovascular primary prevention and more active preventive strategies are still required in the young population to address a possible lack of awareness and poorer control of risk factors. Also, cardiovascular risk in young patients could be strongly influenced by genetic factors and may be harder to control,25 so new approaches to screening and prevention may be needed.
Sex‐Related Differences in Risk Profiles and Outcomes
We found that throughout the 17‐year period of our study, women had a less favorable risk factor profile and higher mortality than men. Numerous previous studies have reported sex differences in the risk profiles of patients with ASCVD.6, 8, 9, 23, 24, 26 As a result, recent guidelines have focused on lifetime risk of ASCVD in women in an effort to address these disparities.27, 28 However, our data suggest that despite these efforts, significant sex disparities remain.
Our findings provide insight into the possible relationships between these disparities in risk profiles and in mortality. After adjustment for baseline and procedural confounders, there was no significant difference in all‐cause mortality between sexes. Consequently, baseline characteristics, such as risk factors, comorbidities, and preprocedural complications, were likely responsible, at least in part, for the worse prognosis in women. In addition, some of the cardiovascular risk factors, such as diabetes mellitus and hypertension, and several comorbidities were both more prevalent and had a greater impact on mortality in women than in men in our study.
Temporal Trends in Outcomes
Finally, although we observed a decrease in mortality risk from 2000 to 2007, there was no further decrease after 2007 in either sex. The lack of further declines mirrors the pattern observed in the overall population of patients with ASCVD, in whom no significant reduction in cardiovascular mortality was seen during the past 6 years.29 As we found an increasing prevalence of several cardiovascular risk factors linked with mortality in this population, more effective screening and treatment of these risk factors may be needed to further reduce mortality.
Limitations
Our study has several important limitations related to the inclusion criteria and the retrospective nature of this analysis. Previous studies have shown that young women with MI have a lower probability of undergoing angiography,30 which may have led to underrepresentation of women in our study, because our inclusion criterion was based on angiographically documented disease. Several risk factors, such as diabetes mellitus, hypertension, and hyperlipidemia, were either self‐reported or captured by attending physicians or medical records and lacked standardized definitions. Our data source was limited to variables collected in the CSBC Registry; thus, other important risk factors, like family history, were not included in our analysis. Also, the registry did not capture data on the quality of in‐hospital care or in‐hospital complication rates. Given the lack of adjudication of cause of death, our study was limited to all‐cause mortality. Finally, the study did not take into consideration chronic medical treatment before and after the index event. A prospective study of patients meeting the same inclusion criteria in BC (SAVE BC [Study to Avoid Cardiovascular Events in BC]) is underway and will provide detailed, prospectively collected phenotypic data on this population.31
Conclusion
In conclusion, the incidence of first presentation with CAD has not declined for young patients in BC from 2000 to 2016. Moreover, a high burden of risk factors and an increasing prevalence of several preventable major cardiovascular risk factors were observed in this cohort. Combined with higher mortality rates in younger women, which are possibly related to their unfavorable cardiovascular risk and comorbidity profiles, these findings suggest a greater need for effective screening and primary prevention strategies in the high‐risk young population to address the stagnation in the prevalence of premature CAD, as well as disparities in risk factors and outcomes between young men and women.
Sources of Funding
This work was supported by funds from the St. Paul's Hospital Foundation and the Vancouver General Hospital Foundation. Dr. Brunham is supported by a Canada Research Chair in Precision Cardiovascular Disease Prevention and is a Michael Smith Foundation for Health Research Scholar.
Disclosures
None.
Supporting information
Table S1. Indications to Cardiac Catheterisation by Year
Acknowledgments
The authors thank staff of the CSBC (Cardiac Services of British Columbia) Registry and BC Centre for Improved Cardiovascular Health for their important contributions. The authors acknowledge the contributions of Patrick Daniele, data analyst, for his assistance with data manipulation.
(J Am Heart Assoc. 2019;8:e012178 DOI: 10.1161/JAHA.119.012178.)
Contributor Information
Simon N. Pimstone, Email: simon.pimstone@ubc.ca.
Liam R. Brunham, Email: liam.brunham@ubc.ca.
References
- 1. Benjamin EJ, Virani SS, Callaway CW, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie G, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JHY, Alger HM, Wong SS, Muntner P. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2. Roth GA, Johnson C, Abajobir A, Abd‐Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis‐Guzman N, Amrock S, Ansari H, Ärnlöv J, Asayesh H, Atey TM, Avila‐Burgos L, Awasthi A, Banerjee A, Barac A, Bärnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castañeda‐Orjuela CA, Castillo‐Rivas J, Catalá‐López F, Choi JY, Christensen H, Cirillo M, Cooper L, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, El Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi‐Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang YH, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, El Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin MJ, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabarés‐Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor‐Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Global status report on noncommunicable diseases 2014. World Health Organization; 2015. http:// www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed November 26, 2018. [DOI] [PubMed] [Google Scholar]
- 4. Eisen A, Giugliano RP, Braunwald E. Updates on acute coronary syndrome: a review. JAMA Cardiol. 2016;1:718–730. [DOI] [PubMed] [Google Scholar]
- 5. Institute for Health Metrics and Evaluation (IHME) . Epi Visualization. Seattle, WA: IHME, University of Washington; 2017. https://vizhub.healthdata.org/epi/. Accessed August 30, 2018. [Google Scholar]
- 6. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001–2010. J Am Coll Cardiol. 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wilmot KA, O'Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011 evidence for stagnation in young adults, especially women. Circulation. 2015;132:997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 9. Singh A, Collins BL, Gupta A, Fatima A, Qamar A, Biery D, Baez J, Cawley M, Klein J, Hainer J, Plutzky J, Cannon CP, Nasir K, Di Carli MF, Bhatt DL, Blankstein R. Cardiovascular risk and statin eligibility of young adults after an MI: partners YOUNG‐MI registry. J Am Coll Cardiol. 2018;71:292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leifheit‐Limson EC, D'Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM, Lichtman JH. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol. 2015;66:1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Global action plan for the prevention and control of NCDs 2013–2020. World Health Organization; 2013. http:// www.who.int/nmh/events/ncd_action_plan/en/. Accessed August 30, 2018. [Google Scholar]
- 12. Kontis V, Mathers CD, Rehm J, Stevens GA, Shield KD, Bonita R, Riley LM, Poznyak V, Beaglehole R, Ezzati M. Contribution of six risk factors to achieving the 25×25 non‐communicable disease mortality reduction target: a modelling study. Lancet. 2014;384:427–437. [DOI] [PubMed] [Google Scholar]
- 13. Lauck SB, Abel JG, Bachiu L, Ding L, Harps H, Louis T, Moore H, Polderman J, Wu SY. Development of a clinical and administrative provincial waitlist management tool to support health service planning and patient access to cardiac catheterization and surgery. Can J Cardiol. 2014;30:S80–S81. [Google Scholar]
- 14. Population estimates on July 1st, by age and sex. Statistics Canada; 2016. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501. Accessed April 14, 2017. [Google Scholar]
- 15. RStudio Team . RStudio: Integrated Development for R. Boston, MA: RStudio, Inc; 2015. Version 1.1.463. [Google Scholar]
- 16. Health indicators interactive tool, indicator: hospitalized heart attack. Canadian Institute for Health Information (CIHI); 2018. http://indicatorlibrary.cihi.ca/pages/viewpage.action?pageId=5111832&_ga=2.36228960.1125941384.1558046961-726935276.1558046961. Accessed August 30, 2018. [Google Scholar]
- 17. Izadnegahdar M, Singer J, Lee MK, Gao M, Thompson CR, Kopec J, Humphries KH. Do younger women fare worse? Sex differences in acute myocardial infarction hospitalization and early mortality rates over ten years. J Womens Health (Larchmt). 2014;23:10–17. [DOI] [PubMed] [Google Scholar]
- 18. Health fact sheets, stats in brief: chronic conditions, 2016. Statistics Canada, 2017. https://www150.statcan.gc.ca/n1/en/catalogue/82-625-X. Accessed August 30, 2018.
- 19. Health fact sheets, stats in brief: smoking, 2017. Statistics Canada, 2017. https://www150.statcan.gc.ca/n1/en/catalogue/82-625-X. Accessed August 30, 2018.
- 20. Body mass index, overweight or obese, self‐reported, adult, age groups (18 years and older). Statistics Canada; 2018. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009620. Accessed August 30, 2018. [Google Scholar]
- 21. Health fact sheets, stats in brief: diabetes, 2016. Statistics Canada, 2017. https://www150.statcan.gc.ca/n1/en/catalogue/82-625-X. Accessed August 30, 2018.
- 22. Canto JG, Kiefe CI, Rogers WJ, Peterson ED, Frederick PD, French WJ, Gibson CM, Pollack CV Jr, Ornato JP, Zalenski RJ, Penney J, Tiefenbrunn AJ, Greenland P. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA. 2011;306:2120–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Leifheit‐Limson EC, Spertus JA, Reid KJ, Jones SB, Vaccarino V, Krumholz HM, Lichtman JH. Prevalence of traditional cardiac risk factors and secondary prevention among patients hospitalized for acute myocardial infarction (AMI): variation by age, sex, and race. J Womens Health (Larchmt). 2013;22:659–666. [DOI] [PubMed] [Google Scholar]
- 24. Lee DS, Chiu M, Manuel DG, Tu K, Wang X, Austin PC, Mattern MY, Mitiku TF, Svenson LW, Putnam W, Flanagan WM, Tu JV. Trends in risk factors for cardiovascular disease in Canada: temporal, socio‐demographic and geographic factors. CMAJ. 2009;181:E55–E66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marenberg ME, Risch N, Berkman LF, Floderus B, de Faire U. Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med. 1994;330:1041–1046. [DOI] [PubMed] [Google Scholar]
- 26. Piackova E, Jäger B, Farhan S, Christ G, Schreiber W, Weidinger F, Stefenelli T, Delle‐Karth G, Kaff A, Maurer G, Huber K. Gender differences in short‐ and long‐term mortality in the Vienna STEMI registry. Int J Cardiol. 2017;244:303–308. [DOI] [PubMed] [Google Scholar]
- 27. Anderson TJ, Grégoire J, Pearson GJ, Barry AR, Couture P, Dawes M, Francis GA, Genest J Jr, Grover S, Gupta M, Hegele RA, Lau DC, Leiter LA, Lonn E, Mancini GBJ, McPherson R, Ngui D, Poirier P, Sievenpiper JL, Stone JA, Thanassoulis G, Ward R. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263–1282. [DOI] [PubMed] [Google Scholar]
- 28. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella‐Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd‐Jones D, Lopez‐Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. Circulation. 2018;0:CIR0000000000000625. [Epub ahead of print]. [Google Scholar]
- 29. Deaths and age‐specific mortality rates, by selected grouped causes. Statistics Canada; 2017. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039201. Accessed August 30, 2018. [Google Scholar]
- 30. Arora S, Stouffer GA, Kucharska‐Newton A, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, Caughey MC. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction: the ARIC Community Surveillance Study. Circulation. 2019;139:1047–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brunham LR, Lynch K, English A, Sutherland R, Weng J, Cho R, Wong GC, Anis AH, Francis GA, Khan NA, McManus B, Wood D, Walley KR, Leipsic J, Humphries KH, Hoens A, Krahn AD, Mancini GBJ, Pimstone S. The design and rationale of SAVE BC: the Study to Avoid CardioVascular Events in British Columbia. Clin Cardiol. 2018;41:888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Indications to Cardiac Catheterisation by Year


