Figure 1. Study Design and Characterization of PH in SSc-ILD Cohort.
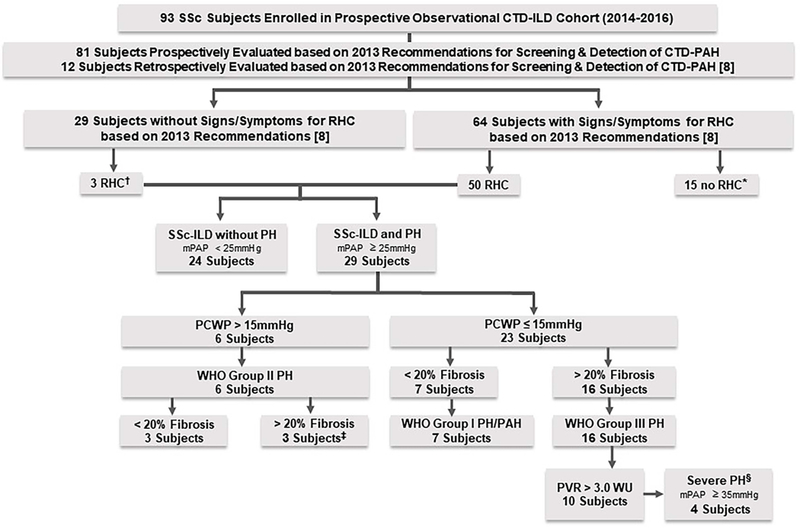
* Seven referred to cardiology, but no RHC as low likelihood of PH based on evidence; 2 refused RHC; 1 lost to follow up; 2 had negative RHC after data analysis; 2 had TTE findings normalize; 1 with stable lower DLCO, normal NTproBNP and no PAH findings on TTE.
†Two underwent RHC due to severe symptoms, which was negative, and 1 underwent RHC due to decline in DLCO and had WHO Group III; none had variables required to calculate DETECT scores.
‡ One subject also had combined post-capillary and pre-capillary PH (PCWP >15mmHg and diastolic PAP – PCWP ≥ 7mmHg) according to Vachiery et al [11] and had features of chronic thromboembolic disease based on pulmonary artery angiogram.
§ SSc-ILD with PH due to ILD who have severe PH based on mPAP ≥ 35mmHg on RHC according to Seeger et al. [12].
PH-pulmonary hypertension; PAH –pulmonary arterial hypertension; SSc-systemic sclerosis; ILD-interstitial lung disease; SSc-ILD-systemic sclerosis associated interstitial lung disease; CTD-connective tissue disease; I/E –inclusion/exclusion; RHC –right heart catheterization; mPAP –mean pulmonary arterial pressure; PCWP-pulmonary capillary wedge pressure; WHO-World Health Organization; PVR –pulmonary vascular resistance; WU-woods units; DLCO-diffusing capacity for carbon monoxide.
