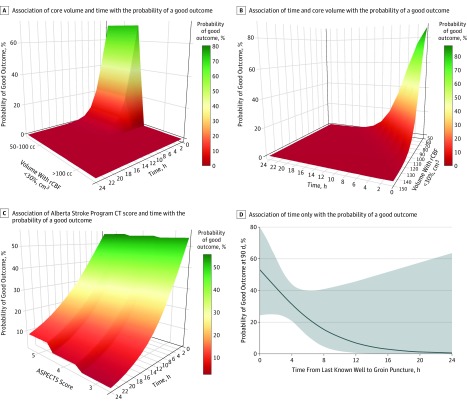
Figure 3. Association of Time and Stroke Size With Thrombectomy Outcomes in Patients With Large Core on Computed Tomographic and Computed Tomographic Perfusion Images.
A, Association of volume (with a relative cerebral blood flow [rCBF] <30%) and time with the probability of a good outcome (90-day modified Rankin Scale score, 0-2) with endovascular thrombectomy (with ischemic core volume in categories of 50-100 cm3 or >100 cm3). A good outcome is associated with core volume and time of computed tomographic (CT) perfusion imaging. There is a decrease in likelihood of a good outcome with increase in the volume and as the time progresses. B, Association of volume (with rCBF <30%) and time with the probability of good outcome with endovascular thrombectomy (ischemic core volume as a continuous variable). A good outcome is associated with the core volume and time of CT perfusion imaging. There is a decrease in the likelihood of a good outcome with increases in volume and time progression. C, Association of Alberta Stroke Program Early CT Score (ASPECTS) and time with the probability of good outcome (90-day modified Rankin Scale score, 0-2) with endovascular thrombectomy (an ASPECTS of 3, 4, or 5). The probability of good outcome is associated with time but does not differ significantly with ASPECTS. There is a decrease in the likelihood of a good outcome with decrease in the ASPECTS and time progression. D, Association of time only on the probability of good outcome with endovascular thrombectomy in patients with large core. The probability of a good outcome decreases significantly as time progresses, with very low probability (<10%) after 12 hours.