Abstract
Purpose
Undisplaced subtle ligamentous Lisfranc injuries are easy to miss or underestimate, and many cases are treated without surgical fixation. It has not yet widely known whether conservative treatment for undisplaced subtle ligamentous Lisfranc injuries may lead to a poor outcome. The purpose of this study is to compare the outcomes of conservative versus surgical management (percutaneous position screw) of undisplaced subtle ligamentous Lisfranc injury.
Methods
We analysed 61 cases in this retrospective study, including 38 males and 23 females. Forty-one patients were managed conservatively, while 20 patients received surgical treatment involving minimal invasive percutaneous position screw. American orthopaedic foot &ankle society (AOFAS), foot function index (FFI, including FFI disability, FFI pain score and activity limitation scale) scores, Maryland foot score and short form-36 (SF-36) were recorded and compared after a follow-up of 10–16 months (average 12.3).
Results
Patients in the surgical management group had higher scores in all evaluation methods (p < 0.05). The complications in the conservative management group had higher incidence, mainly including secondary diastasis (34.1% vs. 5.0%), joint stiffness after 3 months (82.9% vs. 0%), and secondary arthrodesis (12.2% vs. 0%). The highest rate of complication in surgical management group was temporary forefoot pain (55.0%).
Conclusion
The results of this study suggest that the outcomes of the surgical management with percutaneous position screw fixation are better than the conservative management to treat undisplaced subtle ligamentous Lisfranc injuries. This study can serve as a resource for orthopaedic surgeons in recognizing and managing such injuries.
Keywords: Undisplaced subtle ligamentous Lisfranc injuries, Conservative management, Surgical management, Percutaneous position screw, Complications
Introduction
Lisfranc injuries have commonly been used to describe injuries to the bases of the five metatarsals (MTs) to their articulations with the four distal tarsal bones, which comprise tarsometatarsal joints (TMTs). The Lisfranc ligament is an interosseous ligament which locates between the medial cuneiform and the second MT. It is well described that as many as 20% of subtle ligamentous Lisfranc injuries are inappropriately treated either because of missed or underestimated the severity of the injury, and that often leads to poor clinical outcomes.1 Lisfranc injuries can result in a permanent source of foot pain and loss of normal gait, and dysfunction especially in sports activities. The main reason for misdiagnosis is reported to be that 20%–50% Lisfranc injuries which showed no abnormalities in the initial radiographs.2 Recently, by utilizing computed tomography (CT) and magnet resonance images (MRI), the misdiagnosis rate has decreased and more subtle Lisfranc injuries have been recognized. However, surgical or conservative management for undisplaced subtle Lisfranc injuries haven't been established yet and still controversial.
The purpose of the study was to evaluate the outcomes of surgical and conservative management of undisplaced subtle ligamentous Lisfranc injuries. We also discuss the pros and cons of the treatment, which helps orthopaedic surgeons when faced with clinical decision of how to treat these injuries.
Methods
A retrospective study of 61 patients who sustained undisplaced subtle ligamentous Lisfranc injury from May 2012 to May 2017 was conducted. Patients were treated in two orthopaedic centres (Beijing United Family Hospital and Tianjin Hospital, China). The study was approved by the local Ethics committee, and a signed consent obtained from patients.
The study population consisted of 38 male and 23 female patients, with a mean age of 39.4 (range 19–64) years. All the cases were undisplaced subtle ligamentous Lisfranc injuries, and the diagnosis was made by medical history taking, careful physical examination and further confirmed by stress view radiographs, CT or MRI. The injury mechanisms were mainly foot sprain in the midfoot with a plantar flexion force. For example, sports (soccer) injury, jump from a height, or a direct force applied to the foot from dorsal to plantar direction. The cases inclusion criteria were as follows: no fractures in initial radio graphs; the radiographic images showed that the first and second metatarsal had no diastasis (less than 2 mm in gap), but only weight-bearing view showed the diastasis more than 3 mm; further images from CT showed some abnormality including ‘fleck sign’ or MRI showed plantar and interosseous branches of Lisfranc ligament rupture. ‘Fleck sign’ is a small chip of bone found in the space between the first and second metatarsal bases, which indicates avulsion of the Lisfranc ligament.3
The choice of the management of either surgically or conservatively was finally decided by patients, after full explanation of the pros and cons of treatments. Of the 61 patients, 41 patients were managed conservatively while 20 patients received open reduction with internal fixation (ORIF). In cases of ORIF, the implants were removed after 4–6 months (average 5.7 months).
For the surgical treatment, a reduction clamp was used to hold the position of the first and second metatarsal, one or two position screw/screws (depending on whether there is a diastasis between first and second cuneiform) were inserted. A posterior plaster splint was used for two weeks after the wound was well healed, followed by a walking boot with a foot arch supporter for the followed four weeks.
For the conservative management of the undisplaced subtle ligamentous Lisfranc injury, a posterior plaster splint was used for initial three to five days, followed by a full cast to fix the ankle in 90° with foot arch remolding without weight-bearing for totally six weeks. After the cast was removed, a walking boot with foot arch supporter was used to allow patient to fully weight bear for another six weeks.
Patients were followed up ranging from 10 to 16 months (average 12.3 months). At the end of followed up, the radiographs were taken and scores of American orthopaedic foot & ankle society (AOFAS), foot function index (FFI, including FFI disability, FFI pain score and activity limitation scale), Maryland foot score and short form-36 (SF-36) were recorded (Table 1). The surgery related complications were also recorded, which categorized as short term (within 6 months) and long term (over 6 months) complications.
Table 1.
Outcomes of surgical and conservative management of undisplaced subtle ligamentous Lisfranc injuries.
| Score system | Management (Mean ± SD) |
p value | |
|---|---|---|---|
| Surgical | Conservative | ||
| AOFAS midfoot | 90.0 ± 3.7 | 76.3 ± 13.0 | <0.05 |
| FFI disability | 18.0 ± 8.2 | 29.0 ± 13.9 | <0.05 |
| FFI pain | 11.9 ± 3.1 | 24.3 ± 11.2 | <0.05 |
| Activity limitation scale | 3.7 ± 1.5 | 8.1 ± 3.2 | <0.05 |
| Maryland foot score | 88.2 ± 4.0 | 76.6 ± 12.7 | <0.05 |
| SF-36 | 76.8 ± 4.3 | 71.1 ± 12.0 | <0.05 |
AOFAS: American orthopaedic foot & ankle society, FFI: foot function index, SF-36: short form-36.
The SPSS 17.0 software (SPSS Inc., IL, USA) was usedfor data analysis. Quantitative data were expressed asmeans ± standard deviations (SD). Result were compared usingthe Mann-Whitney U test between two groups. p<0.05 is considered as significant.
Results
The median AOFAS score in the surgical treatment group was 89.9 ± 3.7 (range 85–97) compared that of the conservative management group, which was 76.3 ± 13.0 (range 46–97, p < 0.05). The FFI disability score in the surgical treatment group was 17.9 ± 8.2 (range 5–31) and 29.0 ± 14.0 (range 4–79) in the conservative management group (p < 0.05). The FFI pain score in the surgical treatment group was 11.9 ± 3.1 (range 5–15), and 24.3 ± 11.2 (range 3–45) in the conservative management group (p < 0.05). The activity limitation scale in the surgical treatment group was 3.7 ± 1.5 (range 1–7), and 7.9 ± 3.6 (range 3–15) in the conservative management group (p < 0.05). The Maryland foot score in the surgical management group was 88.2 ± 4.0 (range 78–94), and 76.6 ± 12.7 (range 43–98) in the conservative management group (p < 0.05). The SF-36 in the surgical management group was 76.8 ± 4.3 (range 68–82), and 71.1 ± 12.0 (range 40–90) in the conservative management group (p < 0.05) (Table 1).
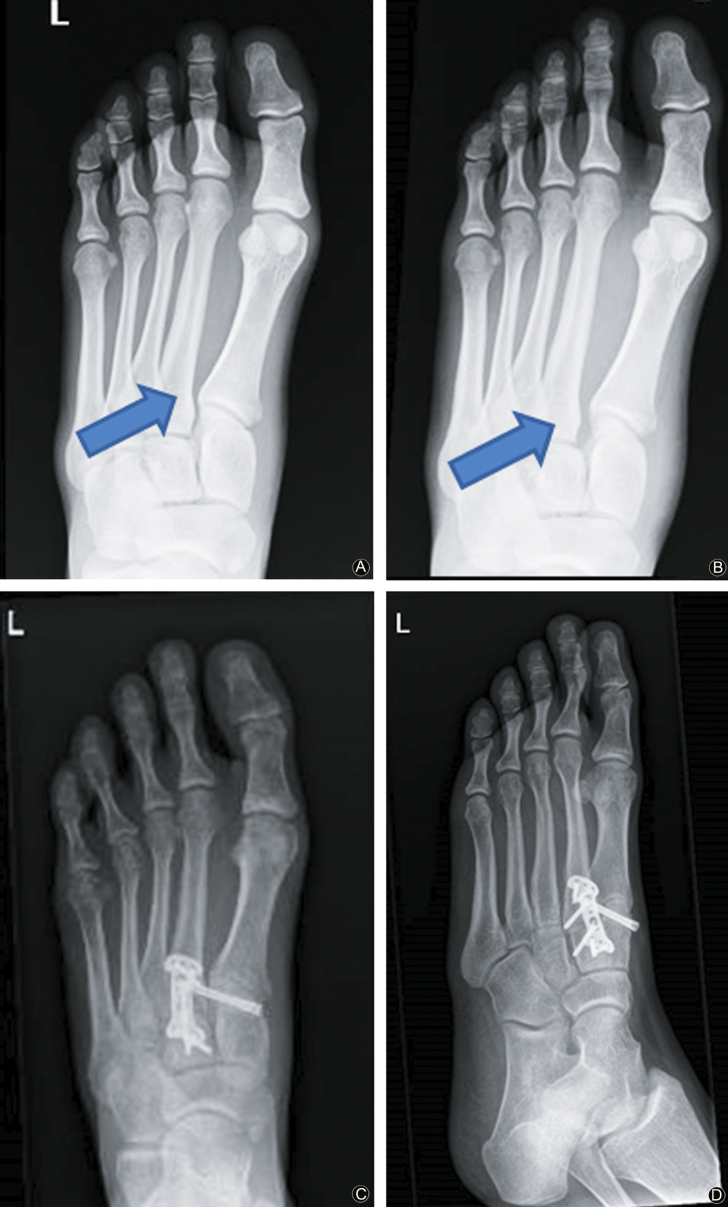
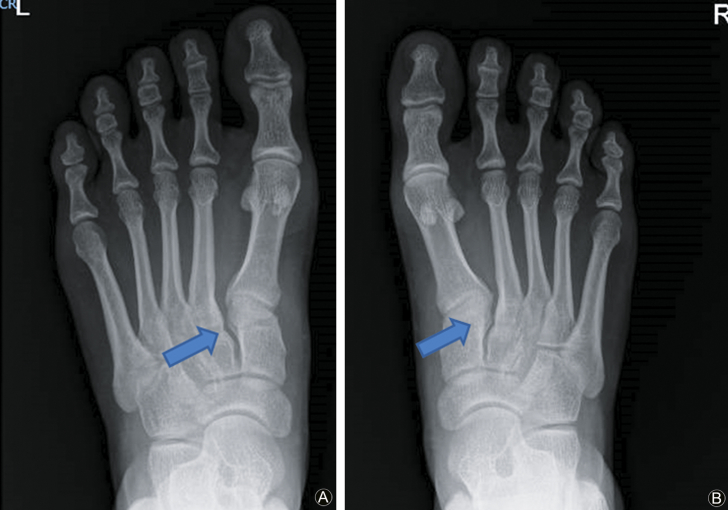
The short term complications were foot pain, surgical site infection, secondary diastasis (Fig. 1), joint pain, joint stiffness; long term (>6 months) complications including loss of foot arch and degenerative arthritis (Fig. 2). Among these cases, some received arthrodesis at late stage (Table 2).
Fig. 1.
(A) The arrow shows there was no diastasis of Lisfranc joint at initial radiograph; (B) The arrow shows there was an obvious diastasis between the first and second MT diastasis after 8 weeks conservative management; (C and D) An arthrodesis was performed at 8 weeks.
Fig. 2.
(A) The arrow shows there was no abnormality at the initial radiograph; (B) The arrow shows there was an osteoarthritis at the second TMT joint at 2 years follow up; (C and D) The arrows shows osteoarthritis at the second TMT joint at 2 years follow up; (E and F) An arthrodesis was performed at 2 years after the initial injury.
Table 2.
Summary of complications experienced by patients in the two groups.
| Complications | Surgical group, n (%) | Conservative group, n (%) |
|---|---|---|
| Infection | 1 (5.0) | 0 (0) |
| Secondary diastasis >3 mm | 1 (5.0) | 14 (34.1) |
| Joint stiffness after 3 month | 0 (0) | 34 (82.9) |
| Temporary forefoot pain <3 month | 11 (55.0) | 7 (17.0) |
| Foot arch loss | 0 (0) | 3 (7.3) |
| Arthritis | 0 (0) | 2 (4.9) |
| Secondary arthrodesis | 0 (0) | 5 (12.2) |
Discussion
Comparing to frank Lisfranc fracture-dislocation, the undisplaced subtle ligamentous Lisfranc injuries are usually caused by low energy forces. It is important to ask patients mechanisms of injury to aid in the diagnosis. The typical mechanisms of injuries are associated with an indirect longitudinal force applied to the forefoot, which is then subjected to rotation and compression causing Lisfranc ligament disruption.4 It commonly can be seen as a twisting injury during sports or a foot stuck into a hole when walking.5 The direct mechanisms of injury usually by a heavy object, applying a force on the midfoot from dorsally to plantarly, such as accidental run over by a car.
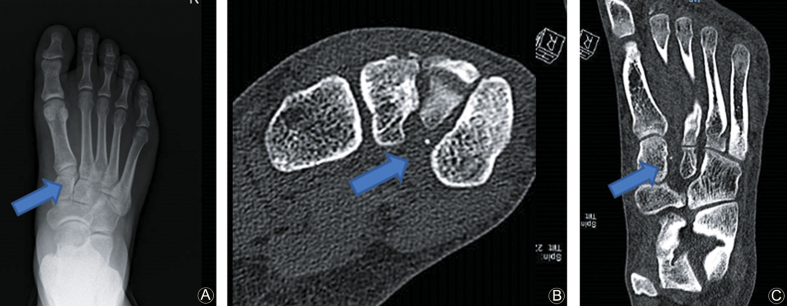
Radiographic imaging
Lisfranc injuries are a challenge to diagnose, and approximately 20% of injuries are unrecognized.1 Radiographic examinations are often enough to demonstrate more obvious Lisfranc fracture dislocations, but miss a significant number of more subtle injuries. Anteroposterior (AP) radiographs are used to demonstrate mal-alignment of the first and second TMT joints, whereas incongruity at the third and fourth joints are better visualized on a 30° oblique view.1 On the lateral view, the dorsal and plantar aspects of the MTs should correspond with the cuneiform and cuboid. A tangential line drawn through the medial aspect of the medial cuneiform and navicular should intersect the first MT base.6
It has been shown that in up to 50% of the patients, non-weight-bearing radiographs were normal and without diastasis between the first and the second metatarsals. The weight bearing views are essential to evaluate the undisplaced subtle ligamentous Lisfranc injuries, which can be obtained as long as 10–14 days after the injury. Lateral weight bearing radiographs can be helpful to identify flattening of the longitudinal arch as well as dorsal displacement at the second TMT joint.7 A weight bearing radiograph can be difficult to obtain at the time of injury because patients find it is very painful to put weight on their injured foot, therefore, some advocate that it should be performed under regional anaesthesia with an ankle block.8 Fig. 3 showed weight bearing AP view of radiograph.
Fig. 3.
(A and B) The weight bearing AP view of bilateral feet. The arrow shows there was a more than 2 mm diastasis between the first and second metatarsals and between medial and middle cuneiforms in the left foot (the injury foot).
When radiographs have little findings, additional studies such as, MRI, and CT will help the diagnosis of ligamentous injury.8, 9 The ‘fleck sign’ in CT scan, in which there is a small chip of bone found in the space between the first and second metatarsal bases, indicating avulsion of the Lisfranc ligament3; this was first described by Myerson et al.10 (Fig. 4).
Fig. 4.
(A) The arrow shows the normal AP view radiograph of foot; (B and C) The arrows show a ‘fleck sign’ between medial and middle cuneiform in the same foot, diagnosed as Lisfranc ligament injury.
In a recent study evaluating MRI images for midfoot instability, Raikin et al.11 found that MRI demonstrating a rupture or grade II sprain of the plantar ligament between the first cuneiform and the bases of the second and third MTs is highly predictive of midfoot instability, and these patients should be treated with surgical stabilization. In our study, we found similar MRI images (Fig. 5).
Fig. 5.
(A) The arrow shows that there was no Lisfrac joint diastasis at AP view radiograph; (B) The arrow shows the plantar branch of Lisfranc ligament ruptured with base of second MT bone bruise at MRI.
Treatment strategies
The controversy about surgery still exists. Nunley and Vertullo8 suggested that the subtle injuries with diastasis <2 mm represent a dorsal capsular tear and sprain without elongation of the Lisfranc ligament, and categorized as a grade I ligament injury. This group of patients did not require surgical treatment. It is suggested that the operative intervention is required only if there is elongation and/or disruption of the Lisfranc ligament. However, we think tear, sprain, and elongation of ligaments are hard to distinguish from each other. Similarly, Lien et al.12 attempted staging of Lisfranc injuries, and recommended operative treatment with restoration of the anatomic alignment of the Lisfranc joint for unstable types. However, drawing a line between stable or nonstable injuries is clinically still very difficult.
We believe that pure ligamentous injuries take far longer to heal and uncertain about its healing ability than their bony counterparts, and the surgical treatment may improve outcomes with a more rapid return to the normal activities. In our clinical practice, we noted there are complications in conservative management group, such as secondary displacement, loss of foot arch and post-traumatic arthritis. Therefore, even undisplaced subtle ligamentous injuries alone should be still considered as problematic as frank Lisfranc fracture-dislocation injuries and worth paying attention to.
As to the surgical technique, screw fixation remains the most widely used technique, although there is evidence to suggest that primary arthrodesis may have superior results.13 However, even medial column of foot is relatively rigid, there is biomechanical subtle movement in the Lisfranc joint,14, 15 it provides elasticity of the medial foot arch during running or jumping. If the Lisfranc joint is rigidly fixed or fused, it will lead to the loss of medial arch elasticity which causes distal first metatarsal pain due to overload while weight bearing. The distal first metatarsal pain after Lisfranc joint internal fixation is the most common complication in our study, and the symptom of all subjects disappear after removing the implants. To treat Lisfranc injuries, both percutaneous position screws and bridge plate fixation can be temporary, the implants can be removed to restore the elasticity of midfoot. Although some investigators reported that the open anatomic reduction and bridge plate fixation is the best way to treat Lisfranc injuries,16 all of the reported cases were high-energy injury related with more than one column involved. Vosbikian et al.17 reported a series of low-energy Lisfranc injuries with Lisfranc ligament disruption confirmed by MRI in 38 patients. The subjects were treated by percutaneous position screws and had excellent outcomes. Besides, the percutaneous position screw procedure is a minimally invasive method with less soft tissue stripping, short surgical duration and less infection rate.
We discovered there are new surgical techniques reported: Lien et al.12 with an endoscopic assisted technique. They remove the torn ligament and interposed ligament by endoscopy and also use endoscopy to guide the cancellous screw. However, this procedure prolongs the surgery time duration. Wataru et al.18 reported a Ligament reconstruction technique through a bone tunnel for chronic subtle Lisfranc injuries. Brin et al.19 reported a single suture button to secure the ligament to the MT.
Complications
The complications of subtle ligamentous Lisfranc injury can be divided into short term and long term complications. For the conservative management group, the most common complication in the short term was joint stiffness; this prolonged the functional recovery time, more hospital visit for physiotherapy. Some of the cases showed a significant loss of range of motion in ankle joint due to the cast immobilization. The second but more severe complication was secondary subluxation, especially for the cases with normal radiographs and underestimated the severity. The salvage management for these cases is inevitably arthrodesis. Two most common long term complications were degenerative arthritis and foot arch loss. We think in these cases, there was mal-union of the Lisfranc ligament, leading the Lisfranc joint instability, resulting in second MT joint osteoarthritis.
For the surgical management group, in addition to surgical site infection and perioperative pain, the most common complication was the first metatarsophalangeal (MP) joint pain at two to three months post-operative period. This pain was emanating from the rigid fixation by positional screws at TMT joint, which altered the flexibility of the joints in the midfoot, and more axial force into metatarsophalangeal (MP) joint. The symptoms gradually disappeared after removing the screws. Although the long term complications of secondary diastasis, osteoarthritis and loss of normal foot arch were seen, but significantly at lower rates (Table 1). This reflected better functional scores in the surgical group.
The results of this study demonstrated that the differences in outcome of the conservative and surgical treatment to the undisplaced subtle Ligamentous Lisfranc injury. We are reporting some poor outcomes of the conservative treatment. Although surgical intervention for treating ligamentous injuries to Lisfranc joint is still controversial, we can learn a lesson and inform patients to give an appropriate warning to consider conservative and surgical management for undisplaced subtle Ligamentous Lisfranc injuries.
Funding
Nil.
Acknowledgements
None at present.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Ethical statement
The study was approved by the local ethics committee, and a signed consent obtained from patients.
Conflicts of interest
The authors declared that there are no conflicts of interest.
References
- 1.Stein R.E. Radiological aspects of the tarsometatarsal joints. Foot Ankle. 1983;3:286–289. doi: 10.1177/107110078300300508. [DOI] [PubMed] [Google Scholar]
- 2.Richter M., Wippermann B., Thermann H. Plantar impact causing midfoot fractures result in higher forces in Chopart's joint than in the ankle joint. J Orthop Res. 2002;20:222–232. doi: 10.1016/S0736-0266(01)00096-1. [DOI] [PubMed] [Google Scholar]
- 3.Tadros A.M., Al-Hussona M. Bilateral tarsometatarsal fracture-dislocations: a missed work-related injury. Singap Med J. 2008;49:e234–e235. [PubMed] [Google Scholar]
- 4.Hatem S.F., Davis A., Sundaram M. Your diagnosis? Midfoot sprain: lisfranc ligament disruption. Orthopedics. 2005;28(2):75–77. doi: 10.3928/0147-7447-20050101-01. [DOI] [PubMed] [Google Scholar]
- 5.Trevino S.G., Kodros S. Controversies in tarsometatarsal injuries. Orthop Clin N Am. 1995;26:229–238. [PubMed] [Google Scholar]
- 6.Coss H.S., Manos R.E., Buoncristiani A. Abduction stress and AP weightbearing radiography of purely ligamentous injury in the tarsometatarsal joint. Foot Ankle Int. 1998;19:537–541. doi: 10.1177/107110079801900806. [DOI] [PubMed] [Google Scholar]
- 7.Faciszewski T., Burks R.T., Manaster B.J. Subtle injuries of the Lisfranc joint. J Bone Joint Surg Am. 1990;72:1519–1522. [PubMed] [Google Scholar]
- 8.Nunley J.A., Vertullo C.J. Classification, investigation, and management of midfoot sprains: lisfranc injuries in the athlete. Am J Sports Med. 2002;30:871–878. doi: 10.1177/03635465020300061901. [DOI] [PubMed] [Google Scholar]
- 9.Aronow M.S. Treatment of the missed Lisfranc injury. Foot Ankle Clin. 2006;11:127–142. doi: 10.1016/j.fcl.2005.12.005. ix. [DOI] [PubMed] [Google Scholar]
- 10.Myerson M.S., Fisher R.T., Burgess A.R. Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle. 1986;6:225–242. doi: 10.1177/107110078600600504. [DOI] [PubMed] [Google Scholar]
- 11.Raikin S.M., Elias I., Dheer S. Prediction of midfoot instability in the subtle Lisfranc injury. Comparison of magnetic resonance imaging with intraoperative findings. J Bone Joint Surg Am. 2009;91:892–899. doi: 10.2106/JBJS.H.01075. [DOI] [PubMed] [Google Scholar]
- 12.Lien S.B., Shen H.C., Lin L.C. Combined innovative portal arthroscopy and fluoroscopy-assisted reduction and fixation in subtle injury of the lisfranc joint complex: analysis of 10 cases. J Foot Ankle Surg. 2017;56:142–147. doi: 10.1053/j.jfas.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Ly T.V., Coetzee J.C. Treatment of primarily ligamentous Lisfranc joint injuries: primary arthrodesis compared with open reduction and internal fixation. A prospective, randomized study. J Bone Joint Surg Am. 2006;88:514–520. doi: 10.2106/JBJS.E.00228. [DOI] [PubMed] [Google Scholar]
- 14.Niu W., Tang T., Zhang M. An in vitro and finite element study of load redistribution in the midfoot. Sci China Life Sci. 2014;57:1191–1196. doi: 10.1007/s11427-014-4731-1. [DOI] [PubMed] [Google Scholar]
- 15.Stevens J., Meijer K., Bijnens W. Gait analysis of foot compensation after arthrodesis of the first metatarsophalangeal joint. Foot Ankle Int. 2017;38:181–191. doi: 10.1177/1071100716674310. [DOI] [PubMed] [Google Scholar]
- 16.Schepers T., Oprel P.P., Van Lieshout E.M. Influence of approach and implant on reduction accuracy and stability in lisfranc fracture-dislocation at the tarsometatarsal joint. Foot Ankle Int. 2013;34:705–710. doi: 10.1177/1071100712468581. [DOI] [PubMed] [Google Scholar]
- 17.Vosbikian M., O'Neil J.T., Piper C. Outcomes after percutaneous reduction and fixation of low-energy lisfranc injuries. Foot Ankle Int. 2017;38:710–715. doi: 10.1177/1071100717706154. [DOI] [PubMed] [Google Scholar]
- 18.Miyamoto W., Takao M., Innami K. Ligament reconstruction with single bone tunnel technique for chronic symptomatic subtle injury of the Lisfranc joint in athletes. Arch Orthop Trauma Surg. 2015;135:1063–1070. doi: 10.1007/s00402-015-2250-6. [DOI] [PubMed] [Google Scholar]
- 19.Brin Y.S., Nyska M., Kish B. Lisfranc injury repair with the TightRope device: a short-term case series. Foot Ankle Int. 2010;31:624–627. doi: 10.3113/FAI.2010.0624. [DOI] [PubMed] [Google Scholar]