Abstract
Objective:
While conduct problems (CP) and hyperactivity/attention problems (HAP) are thought to covary with regularity, few studies have traced the probability of co-occurring CP and HAP longitudinally, particularly beginning in the toddler period. Further, there is little research examining how early co-occurring trajectories of CP and HAP predict functioning across several domains through late adolescence and early adulthood.
Method:
Using a cohort of 284 low-income boys, we examined whether separate developmental trajectories of overt CP and HAP symptomatology from ages 2 to 10 relate to violent behavior, established correlates of antisocial behavior, impulsivity, and internalizing problems in adolescence and early adulthood. Co-occurring trajectory patterns of CP and HAP from ages 2 to 10 were also investigated in relation to later maladjustment.
Results:
Findings indicated that trajectories of CP beginning in early childhood were related to violent behavior in adolescence and adulthood, adolescent correlates of antisocial behavior (i.e., deviant talk with peers), and internalizing problems in adulthood. Early HAP trajectories were also related to later problem behaviors when considered in isolation. However, when examining trajectories of CP and HAP simultaneously, children with chronic CP + chronic HAP, but not HAP-only, were most at risk for multiple types of problem behaviors in adolescence and early adulthood, including violent behavior and depressive and anxiety symptoms. Thus, HAP symptomatology was no longer predictive of adolescent and adult functioning once co-occurring CP was accounted for.
Conclusions:
Findings extend prior research with older children of HAP and/or CP, highlighting the predictive value of trajectories of CP beginning in the toddler period.
Characterizing childhood pathways to antisocial behavior (AB) is important to identify those who would benefit from early prevention and intervention (Dishion & Patterson, 2016). Relative to late-starters, children with the early-starting pattern of conduct problems (CP) show a more persistent and chronic trajectory of AB from early childhood into adulthood that is associated with significant societal costs and co-occurring problematic behavior (Moffitt, Caspi, Harrington, & Milne, 2002; Rivenbark et al., 2017; Shaw, Hyde, & Brennan, 2012). For example, children with co-occurring CP and hyperactivity-attention problems (HAP) differ from HAP-only and CP-only children by having an earlier onset of CP and displaying more serious forms of AB and other mental health problems in adolescence and adulthood (Biederman, Petty, Dolan, & Hughes, 2008; Sibley et al., 2011; Waschbusch, 2002). However, few studies have examined how co-occurrence among children’s developmental trajectories of CP and HAP beginning in toddlerhood predicts functioning across several domains of mental health through late adolescence and early adulthood, such as deviant communication patterns, serious violent behavior, and internalizing problems. As AB typically peaks in late adolescence and early adulthood, these are particularly critical developmental periods for understanding the persistence or desistence of AB. Thus, the current study examined the predictive value of developmental trajectories of CP and HAP previously established by Shaw, Lacourse, and Nagin (2005), using a high-risk sample of boys followed prospectively from infancy through early adulthood.
The Developmental Heterogeneity of CP and HAP
Despite prior research on the co-occurrence between CP and HAP, few studies have examined heterogeneity in developmental trajectories of CP and HAP beginning in early childhood. Understanding individual differences in these developmental pathways can help in identifying specific groups of children at increased risk for persistent AB which may escalate to more violent and dangerous behaviors in adulthood. With the advent of Nagin’s (1999) semi-parametric, group-based approach for modeling development trajectories, it became possible to identify distinctive clusters of individuals within a population who share common and dissimilar pathways, including for CP and/or HAP. As a part of growing number of person-oriented methods, classification of more homogeneous groups occurs based on the pattern of trajectories over time rather than using an a priori criterion. While variable-oriented approaches restrict all children to following a single mean trajectory, potentially obscuring patterns of change unique to subgroups of children, person-centered approaches can reveal symptom trajectories that vary not only in rank-order but also in functional form.
In one of the first studies to apply a semi-parametric growth modeling method to the identification of CP and HAP pathways, beginning at child age 6, Nagin and Tremblay (1999) identified four similar developmental trajectories for physical aggression, oppositionality, and hyperactivity, including a chronic persistence trajectory, a high moderate-desisting trajectory, a moderate-level desisting trajectory, and a persistent low-problem trajectory. However, in contrast to prior studies modeling children’s CP and HAP beginning at school age or later (Fontaine et al., 2008; Nagin & Tremblay, 1999; Nagin & Tremblay, 2001b), in one of the few studies initiated during early childhood, Shaw et al. (2005) examined separate trajectories of overt CP and HAP from ages 2 to 10 using the current sample of low-income and racially diverse boys. Shaw et al. (2005) identified four similar trajectory groups for both CP and HAP, including persistently high and persistently low CP and HAP groups, as well as moderately high and moderately low desister CP and HAP groups. These trajectories were consistent with prior studies examining trajectories of CP and HAP (Fontaine et al., 2008; Nagin & Tremblay, 1999). Despite differences in sample characteristics (e.g., Fontaine study included only females), the similar CP and HAP trajectory groups found across all three studies suggest that these disruptive problem behaviors follow comparable developmental courses from early childhood onward. All three investigative teams also found similar patterns of co-occurrence between the CP and HAP trajectory groups. Specifically, their analyses showed that a majority of youth showing chronic CP usually also showed chronic HAP. In contrast, a more sizeable portion of children showing chronic HAP remained free of chronic CP.
Risks Associated with Differing Trajectories of CP and HAP
Early childhood CP and HAP have been shown to be important components of a larger developmental cascade that ultimately lead to serious AB in adolescence and beyond. Due in part to a shared underlying vulnerability for trait impulsivity conferred by dysfunction of the mesolimbic dopaminergic system (Gatzke-Kopp et al., 2009), children with ADHD have been shown to be at risk for CP (Beauchaine, Hinshaw, & Pang, 2010). Indeed, impulsivity, a hallmark feature of ADHD, might increase risk for persistent and serious AB by impairing the ability to think through consequences or disengage from pursuing rewards when instructed (e.g., Humphreys & Lee, 2011; Masunami, Okazaki, & Maekawa, 2009). Impulsivity may also lead to greater frustrated reactivity and aggression when tolerating distress (e.g., Seymour, Macatee, & Chronis-Tuscano, 2016). Accordingly, numerous studies have also shown that school-age children with elevated HAP are at increased risk for CP and more serious forms of AB in adolescence and early adulthood (e.g., Babinski et al., 1999; Sibley et al., 2011). However, despite studies linking early HAP with subsequent AB, research on the unique effects of HAP remains inconclusive. Whereas some studies have found that HAP in early or middle childhood were unrelated to AB in adolescence or adulthood after accounting for CP (e.g., Nagin & Tremblay, 1999; Mordre et al., 2011), others have found significant effects of HAP independent of prior levels of AB (e.g., Babinski et al., 1999; Lee & Hinshaw, 2004; Mannuzza, Klein, Abikoff, & Moulton, 2004; Sibley et al., 2011; Waschbusch, 2000).
The aforementioned literature suggests that the incremental utility of HAP in predicting future CP remains unclear. This lack of clarity may exist because ADHD children’s risk for future CP has been shown to be influenced by accumulating exposure to environmental risks that have cascading effects throughout development (Beauchaine et al., 2010). Therefore, it is possible that an underlying vulnerability for externalizing problems indexed by impulsivity may result in HAP-only in supportive environments but escalate to more serious patterns of co-occurring HAP + CP in the context of family dysfunction and stress. For example, impulsive children have been shown to be at risk for CP in the context of coercive parenting (Meier, Slutske, Heath & Martin, 2009) and high-crime neighborhoods (Lynam et al., 2000). These contexts may increase the likelihood of exposure to neighborhood violence and delinquency that further potentiates CP (Dishion, McCord, & Poulin, 1999; Lynam et al., 2000; Meier, Slutske, Arndt, & Cadoret, 2008).
Because vulnerabilities that increase risk for early CP are also involved in maintaining and exacerbating risk for future CP (Beauchaine et al., 2010), it is not surprising that many studies have demonstrated that the emergence and persistence of CP during early childhood is one of the most robust predictors of serious AB at later developmental periods (e.g., Aguilar, Sroufe, Egeland, & Carlson, 2000; Campbell, Shaw, & Gilliom, 2000; Loeber & Dishion, 1983). Although early CP frequently co-occur with HAP (Waschbusch, 2002), there is extensive research documenting the unique effects of childhood CP on adolescent and adult AB after accounting for HAP (e.g., Farrington et al., 1990; Lahey, Loeber, Burke, & Applegate, 2005; Mordre et al., 2011).
While prior research has linked early CP and HAP measured at a single time point with adolescent and early adult outcomes, fewer studies have examined whether CP and HAP trajectories are related to later maladaptive functioning. Indeed, the chronicity and/or growth of CP and HAP over time might be more informative of future adulthood outcomes when compared to levels of CP and HAP at one point in time. Nagin and Tremblay (1999) found that boys’ physical aggression trajectories from ages 6 to 12 uniquely predicted AB at age 17 after controlling for HAP, whereas HAP trajectories did not uniquely predict age-17 AB after accounting for earlier physical aggression. Notably, Nagin and Tremblay (1999) did not evaluate the risk associated with co-occurring physical aggression and HAP. Furthermore, Pingault et al. (2013) found that boys’ physical aggression trajectories from ages 6 to 12 predicted criminal charges at age 25 before and after adjusting for hyperactivity and inattention trajectories, whereas trajectories of hyperactivity predicted criminality only when physical aggression was not accounted for. These studies collectively suggest that based on the confluence of deficits associated with each disorder, children displaying chronic CP or co-occurring CP/HAP may show the worst outcomes later in life when compared to children following chronic HAP-only or other trajectories of CP and HAP. Indeed, research has demonstrated that school-aged children and adolescents with co-occurring CP and HAP show greater levels of aggression, criminal behavior, substance use, and antisocial personality disorder as adults when compared to those showing CP-only, HAP-only or few symptoms of either problem behavior (e.g., Loeber et al., 1990; Waschbusch, 2000).
While early trajectories of CP and HAP have been linked to later AB, it is unclear whether these trajectories are predictive specifically of violent behaviors or serve as collateral predictors of general maladjustment in early adulthood. Indeed, Caspi et al. (2016) found that 20% of adults in the Dunedin Study accounted for approximately 80% of the cohort’s societal costs at 38 years, including criminal convictions, social welfare benefits, pharmaceutical prescriptions, and hospital bed-nights. Furthermore, poor self-control in early childhood, operationalized to include measures of impulsivity, CP, and HAP, was a significant predictor of risk for belonging to the high-cost group in adulthood. However, while Caspi et al. (2016) assessed CP and HAP at multiple ages (i.e., 5, 7, 9, and 11 years), a single measure of self-control was computed by averaging across ages and different types of problem behaviors. As less is known about how early-starting trajectories of CP and HAP relate to adolescent and adult functioning, the present study examined whether CP and HAP trajectories from ages 2 to 10 are predictive of violent behavior, less serious forms of AB, and peer correlates of AB (i.e., deviant talk; Granic & Dishion, 2003). Our unique approach of examining CP and HAP trajectories from toddlerhood to late childhood has the potential to more comprehensively capture HAP severity than prior studies, which may clarify the inconsistent literature on the unique contribution of HAP to AB. Assessment methodology included observational tasks, official court records, and youth reports. Furthermore, consistent with prior research suggesting that a small fraction of the adult population may demonstrate multiple types of problem behaviors that account for a disproportionate share of societal costs, we also assessed for other indicators of maladjustment in early adulthood. Based on our co-focus on HAP, we explored how trajectories of HAP and CP were related to impulsivity in early adulthood (Mathias et al., 2007). Finally, we also examined whether chronic trajectories of CP and/or HAP were related to young men’s depression and anxiety. Examining internalizing problems is important because CP and HAP may play causal roles in evoking demoralizing failures across multiple domains of life (Capaldi, 1991) and/or share similar trait-level risk factors with internalizing problems (Tackett, Waldman, Van Hulle & Lahey, 2011; Wang, Chassin, Eisenberg & Spinrad, 2015). By examining violent behavior, established correlates of AB and other problem behaviors (i.e., deviant talk with peers), and internalizing problems in young adulthood, the current study also addressed homotypic vs. heterotypic continuity and specificity in the range of adjustment difficulties for youth with persistent histories of CP and/or HAP.
The Current Study
The present study extends prior research by examining the unique effects of HAP and CP on later problem behaviors while also utilizing a person-oriented approach for modeling developmental trajectories. Using a low-income sample of boys followed prospectively from infancy through early adulthood, we tested three study aims. First and second, we compared the outcomes of children following four previously identified CP trajectories and four previously identified HAP trajectories (Shaw et al., 2005). We hypothesized that children following the chronic CP trajectory would show the poorest outcomes across domains of adjustment when compared to all other CP groups. Similarly, we expected that children following the chronic HAP trajectory also would show the poorest outcomes when compared to all other HAP groups. Third, to examine how co-occurring patterns of CP and HAP relate to adolescent and adult functioning, we compared the following groups: 1) youth with chronic CP + chronic HAP, 2) the chronic HAP-only trajectory (i.e., those without chronic CP), 3) youth with low CP + low HAP, and 4) all other trajectories. We hypothesized that children with chronic CP + chronic HAP would show the poorest outcomes with the exception of impulsivity, wherein they might show similar or lower levels compared to children in the HAP-only group. Finally, we expected that children following the chronic HAP-only trajectory would show poorer outcomes when compared to all groups except for children with chronic CP + chronic HAP.
Methods
Participants
Participants were drawn from the Pitt Mother & Child Project, a prospective longitudinal study of child vulnerability and resiliency in low-income, high-risk youth (Shaw et al., 2003). Beginning in 1991, 310 infant boys and their primary caregivers were recruited from Women, Infants, and Children Program (WIC) Nutritional Supplement Clinics in Allegheny County, PA when the boys were between 6 and 17 months old. Participation was limited to boys because of the project’s original focus on the developmental precursors of AB, which occurs at higher rates in men (American Psychiatric Association, 2013; Kessler et al., 1994).
At the time of recruitment, the boys were between 6 and 17 months and 53% of them were European American, 36% were African American, 5% were biracial, and 6% were of other races (e.g., Asian American or Hispanic). Families also were required to have at least one other child at home or “on the way” (i.e., mother in 2nd trimester or later of pregnancy) to further increase child risk of AB. At the study’s outset, the mean per capita income was $241 per month ($2892 per year), and the mean Hollingshead SES score was 24.5, indicating a working class sample (Hollingshead, 1975). Mothers ranged in age from 17 to 43 years (M = 28.20 years), and in reporting their relationship status, 63% were married or cohabitating, 28% had always been single, 8% were divorced or separated, and 1% were other (e.g., widowed). Fifty-nine percent of the mothers had 12 years of education or less. Thus, boys in the sample were considered to be at elevated risk for behavioral problems based on their low SES, family size, and child sex.
Retention rates have been consistently high throughout the two decades of data collection. Of the 310 families recruited for the initial assessment at age 1.5 years, data were available on 84–91% of families at ages 3.5 to 10, and 81–83% at ages 17 to 22 (i.e., 83% at age 22). The current study utilized the same sample of 284 boys used by Shaw et al. (2005), who restricted their analyses to participants with measures of CP at three or more time points for purposes of modeling individual trajectories. As reported by Shaw et al. (2005), those included versus excluded from study analyses did not significantly differ with respect to key demographic, parenting, or child-related variables at age 2, including maternal age, maternal education, child fearlessness, child negative emotionality, maternal depressive symptoms, or rejecting parenting. As there were small sample sizes of certain trajectory groups (e.g., chronic CP: n = 19) and missing data on age 20 outcomes (i.e., missing data on 22 men), expectation-maximization (EM) algorithm was used to replace missing values for the 284 participants in our subsample.
Procedure
Two- to three-hour assessments were conducted almost annually in families’ homes and/or laboratory settings with mothers and their participating child from toddlerhood through early adulthood. The assessments providing data for the present study occurred at child ages 1.5, 2, 3.5, 5, 5.5, 6, 8, 10, 17, and 20 years. During the age 1.5 to 17 year assessments, mothers and when available, alternative caregivers, completed a series of questionnaires regarding socio-demographic characteristics, family functioning (e.g., parenting), and child behavior. At age 20, young men completed questionnaires regarding their behaviors and attitudes. Additionally, juvenile court records from Allegheny County, PA, were collected when participants were between 12 and 18 years of age and adult court records were obtained via public records searches in the state of Pennsylvania. All participants provided consent and were compensated for their time after each assessment. All procedures received Institutional Review Board approval at the University of Pittsburgh.
Measures
Trajectories of CP and Hyperactivity (Figures 1 and 2).
Figure 1.
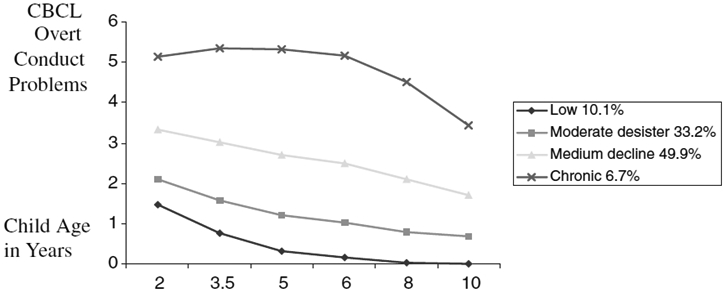
Trajectories of overt conduct problems from ages 2 to 10
Figure 2.
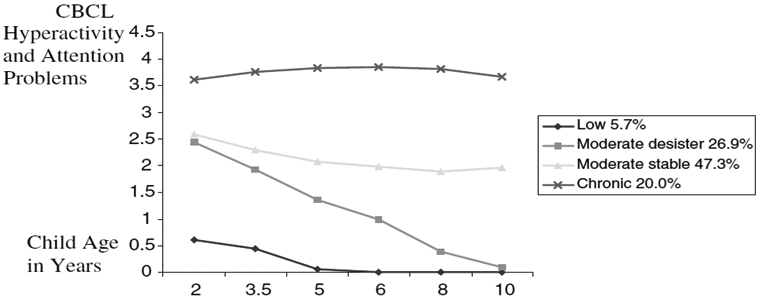
Trajectories of hyperactivity/attention problems from ages 2 to 10
The present study examined previously established trajectories of overt CP, HAP, and co-occurring patterns of CP and HAP from ages 2 to 10 (Shaw et al., 2005). Five items focusing on physical aggression, oppositional behavior, and temper tantrums found on both early child and child/adolescent versions of the Child Behavior Checklist (CBCL; Achenbach, 1991, 1992) were aggregated to generate a factor for CP, and 3 items tapping attention, impulsivity, hyperactivity were generated to form a factor for HAP. For the CP factor, average inter-item correlations ranged from a low of .302 at age 2 to a high of .404 at age 10. Average inter-item correlations for the HAP factor ranged from 0.350 at age 2 to .439 at age 10.
Employing semi-parametric group-based mixture modeling with Proc Traj in SAS, Shaw et al. (2005) identified four distinct trajectory groups on the basis of CP: low (n = 29; 10.1%), moderate desisters (n = 94; 33.2%), medium decline (n = 142; 49.4%), and chronic (n = 19; 6.7%). Analyses similarly yielded four distinct groups for HAP symptoms: low (n = 16; 5.7%), moderate desisters (n = 77; 26.9%), moderate stable (n = 134; 47.3%), and chronic (n = 57; 20.2%). Finally, Shaw et al. (2005) categorized boys as belonging to one of four groups based on their pattern of co-occurring CP and HAP: 1) chronic HAP without chronic CP (i.e., boys in the low, moderate desister, or medium decline CP groups), 2) chronic CP + chronic HAP trajectories, 3) low CP + low HAP trajectories, and 4) those encompassing all remaining trajectories. As many children in the chronic CP group also showed chronic HAP in early childhood (n = 10), we lacked statistical power to evaluate a “pure” chronic CP group. A more extensive description of how these trajectories were created can be found in Shaw et al. (2005).
Violent Petitions.
After receiving written permission from primary caregivers (n = 272), juvenile court records of arrests were obtained from local county offices until the youth was 18 years of age. Juvenile records were obtained for 87% of the initial recruitment sample. Consistent with prior work using this sample (Sitnick et al., 2017), violent petitions were used to minimize the potential for social class and race to influence the outcome of court proceedings, as petitions are filed after the arrest but prior to court proceedings. Juvenile petitions are equivalent to the number of criminal charges pressed against the boy in this state, and boys with a petition for violent acts or threat of violent acts were categorized as violent offenders. The following petitions were included in this category for their harm or potential for harm to others: homicide and attempted homicide, forcible rape, indecent and sexual assault, aggravated assault, robbery, arson, and weapons possession. If a participant had petitions for both nonviolent and violent criminal behavior, the violent offense would supersede the other offenses in terms of group placement. Of the 284 participants included in the present sample, 53 had at least one petition for a violent crime.
Similarly, adult arrest records in the state of Pennsylvania were obtained for all participants (N = 310) via public record search from the ages of 18 to 22. In keeping with the Federal Bureau of Investigation’s (U.S. Department of Justice, 2017) definition of violent crime, participants were categorized as having a violent offense as an adult if they had arrest records for homicide and attempted homicide, forcible rape, indecent and sexual assault, aggravated assault, robbery, or arson. Unlike with the juvenile petitions, weapons offenses were not included for adults can legally possess firearms. Again, individuals with both violent and nonviolent offenses were categorized as violent. It is noteworthy that adult court records for all participants in the state of Pennsylvania were searched. If no court records were obtained, then participants were scored as having no adult offenses. However, as searches were limited to Pennsylvania, it is possible that non-offenders have offenses outside of the state.
Finally, juvenile and adult records were combined such that participants who had any violent juvenile or adult offenses were categorized as “violent offenders.” Combining juvenile and adult court records was advantageous, as some of the juvenile violent offenders were still incarcerated for their offenses at the time of the adult records search. Thus, using only adult records would have inaccurately resulted in the participant being classified as a non-offender. To minimize missing data for those participants who had missing data for their juvenile court records, these participants were coded as having no juvenile court records similar to the treatment of adult court records. However, as with adult records, it is possible that those participants had offenses in other states.
It is noteworthy that there were significant differences in attrition at age 20 specific to arrest records [F (2, 26) = 4.774, p = .009], such that individuals who were arrested for violent criminal behavior (see court records below) were more likely to have missing data at age 20 than nonviolent offenders and those with no criminal records. This is not surprising as these individuals were more likely to be incarcerated and unavailable for an assessment.
Deviant Peer Talk.
At age 17, boys invited a friend to the lab to participate in a 40-minute, videotaped discussion task. Each dyad was asked to discuss the following eight topics for five minutes each: 1) planning an activity together, 2) a current problem nominated by the target child, 3) a current problem nominated by the participating peer, 4) alcohol and drug use, 5) goals for the next year, 6) dating and relationships, 7) friends and peer groups, and 8) planning a party. Conversations were then transcribed and coded by trained research assistants for verbal and non-verbal behaviors using the Norm Topic Code (NTC; Piehler & Dishion, 2005). Each sentence was considered a unit and was coded as being deviant, normative, or reinforcement. Deviant talk was operationalized to refer to all verbal and nonverbal behavior that is not appropriate to the setting or task, such as talking about using drugs or alcohol (e.g., “How much beer can you get?”), using obscene language or gestures (e.g., fingering the camera), and inciting the other person to break the rules of the session (e.g., “Take a piss on the microphone.”)
Self-Reported Violent Behavior.
At age 20, participants completed a 53-item, modified version of the Self-Report of Delinquency Questionnaire (SRD; Elliott, Huizinga, & Ageton, 1985), rating the frequency of their AB during the past year on a 3-point scale (1 = never to 3 = more often). For the present study, boys’ violent behavior scores were computed by summing 11 items describing aggressive or violent acts, such as “Have you physically hurt or threatened to hurt someone to get them to have sex with you?” and “Have you attacked someone with a weapon or with the idea of seriously hurting or killing them?” The resulting scale showed adequate internal consistency (α = .78).
Self-Reported Impulsivity.
Impulsivity was assessed at age 20 using the Barratt Impulsiveness Scale-Version II (BIS-II; Patton, Stanford, & Barratt, 1995). The BIS is a widely used and psychometrically sound measure that assesses various forms of impulsivity, including attentional, motor, and non-planning impulsiveness. Men rated how they act and think in different situations on a 4-point scale (1 = rarely/never to 3 = almost always/always), and a total score was computed by summing all 30 items (α = .79).
Self-Reported Depression.
At age 20, men completed the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock & Erbaugh, 1961), a well-established and widely used measure of depressive states. Men rated the intensity of 21 depressive symptoms over the past 6 months on a 4-point Likert scale (0 = no symptomatology to 3 = severe symptomatology), and a total score was derived by summing these items (α = .86).
Self-Reported Anxiety.
At age 20 men reported on their anxiety symptoms using the 21-item Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988). Men rated how much each symptom bothered them over the past month using a 3-point scale ranging from not at all to severely/it bothered me a lot. The total score was used, with sample items including “fear of losing control” and “unable to relax” (α = .93).
Covariates.
Demographic data were collected at the age 2 home assessment and included as covariates in study analyses. Monthly family income and the primary caregiver’s level of educational attainment were included as covariates with education level dummy coded as 0 = less than high school diploma and 1 = high school diploma or higher. A single dummy code was also used to indicate minority status (0 = European American, 1 = Other races and ethnicities). As the vast majority of non-European American boys were part or fully African American, we combined the small samples of biracial and Hispanic participants with the larger African American group, and refer to non-European American boys as African American for the duration of this manuscript.
Data Analyses.
All analyses were conducted using SPSS Statistics 24 (IBM Corp, 2013). Following inspection of bivariate correlations, we tested the association between CP and HAP trajectory group membership and subsequent adolescent and adult behavioral problems. Separate analyses were conducted for adolescent and adult outcomes to examine convergence in findings between these two developmental periods. One-way ANCOVAs were computed to assess the association between trajectory group membership and deviant talk during an observational task with a peer at age 17. As violent petitions were coded dichotomously, a multinomial logistic regression was used to model the relationship between class membership and arrests. Odds-ratios and their 95% confidence intervals are reported in tables. After examining group differences in adolescent functioning, we computed a series of one-way MANCOVAs to test associations between trajectory group membership and self-reported impulsivity, violent behavior, depression, and anxiety in early adulthood. Following a significant MANCOVA, we examined separate outcomes via analyses of covariance (ANCOVAs) plus Bonferroni post-hoc comparisons of each subgroup contrast. Separate analyses were conducted for each of the three trajectory groups (i.e., CP, HAP, and co-occurring CP/HAP), yielding a total of three one-way MANCOVAS that were computed. All analyses adjusted for the effects of minority status, maternal education, and family income at 18 months.
Results
Descriptive Statistics and Bivariate Correlations
Descriptive statistics for study variables are presented in Table 1. Skew did not exceed +/− 2.00 and kurtosis did not exceed +/− 7.00 (Curran, West, & Finch, 1996). Table 2 presents bivariate correlations among study covariates and adolescent and adult outcomes. Minority status was significantly associated with juvenile/adult violent petitions and self-reported impulsivity at age 20, with African American boys more likely to be arrested for violent crimes during adolescence but reporting lower levels of impulsivity in early adulthood relative to European American boys. Additionally, lower levels of family income were related to higher levels of deviant talk, an increased likelihood of being convicted of a violent crime in adolescence, and higher levels of violent behavior in early adulthood. Violent petitions as a juvenile or young adult were related to higher levels of deviant talk at age 17 and higher levels of violent behavior at age 20, but unrelated to internalizing symptoms at age 20. Conversely, violent arrests in adolescence or adulthood, deviant talk at age 17, and self-reported impulsivity, depressive symptoms, and anxiety symptoms at age 20 were all significantly related to youth-reported violent behavior at age 20.
Table 1.
Descriptive Statistics
| Min | Max | Mean | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|
| Minority Status | 0.00 | 1.00 | 0.53 | 0.50 | −0.10 | −2.00 |
| Maternal Education (18 months) | 0.00 | 1.00 | 0.77 | 0.33 | −1.94 | 3.37 |
| Monthly Family Income (18 months) | 248.00 | 4000.00 | 1049.28 | 643.14 | 1.18 | 1.49 |
| Violent Petitions (Juvenile & Adult) | 0.00 | 1.00 | 0.22 | 0.41 | 1.37 | −0.11 |
| Deviant Talk (Age 17) | 0.00 | 9.00 | 2.83 | 2.51 | 0.56 | −0.76 |
| Impulsivity (Age 20) | 9.00 | 61.00 | 29.99 | 8.40 | 0.41 | 1.17 |
| Violent Behavior (Age 20) | 10.00 | 18.00 | 11.80 | 1.22 | 1.99 | 4.65 |
| Depressive Symptoms (Age 20) | 0.00 | 32.00 | 5.39 | 5.23 | 1.68 | 4.04 |
| Anxiety Symptoms (Age 20) | 0.00 | 38.00 | 6.67 | 7.68 | 1.97 | 4.42 |
Note.
p < .10.
p < .05.
p < .01. Minority Status: 0 = European American, 1 = Other races and ethnicities; Maternal Education: 0 = Less than high school diploma, 1 = High school diploma or higher; Violent Petitions: 0 = No Violent Petitions, 1 = Violent Petitions
Table 2.
Correlation Matrix
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Minority Status | 1 | ||||||||
| 2. Maternal Education (18 months) | −0.02 | 1 | |||||||
| 3. Family Income (18 months) | −0.33** | 0.21** | 1 | ||||||
| 4. Violent Petitions (Juvenile & Adult) |
0.260** | −0.07 | −0.18** | 1 | |||||
| 5. Deviant Talk (Age 17) | −0.07 | −0.06 | −0.13* | 0.14* | 1 | ||||
| 6. Impulsivity (Age 20) | −0.13* | 0.06 | 0.10† | 0.018 | 0.25** | 1 | |||
| 7. Violent Behavior (Age 20) | 0.07 | 0.01 | −0.13* | 0.092 | 0.31** | 0.30** | 1 | ||
| 8. Depressive Symptoms (Age 20) | 0.02 | 0.05 | −0.06 | 0.082 | 0.15* | 0.47** | 0.41** | 1 | |
| 9. Anxiety Symptoms (Age 20) | −0.04 | 0.10† | 0.03 | −0.011 | 0.08 | 0.42** | 0.35** | 0.60** | 1 |
Note.
p < .10.
p < .05.
p < .01. Minority Status: 0 = European American, 1 = Other races and ethnicities; Maternal Education: 0 = Less than high school diploma, 1 = High school diploma or higher; Violent Petitions: 0 = No Violent Petitions, 1 = Violent Petitions
Adolescent Outcomes Associated with CP Trajectory Groups
We next examined the hypothesis that CP trajectory group membership would discriminate adolescent outcomes. As reported in Table 3 and consistent with study hypotheses, results from the one-way ANCOVA indicated a significant effect of CP trajectory group on observed levels of deviant talk with a peer during adolescence. Post-hoc tests showed that the chronic CP group demonstrated more deviant talk than the low CP, moderate desister, and medium decline groups. The medium decline CP group also showed higher levels of deviant talk than the moderate desister groups. Next, a multinomial logistic regression was computed to examine whether CP class membership was associated with violent petitions, controlling for the effects of minority status, maternal education, and family income. Results indicated that children in the chronic CP group had a higher probability of having a violent petition as a juvenile or adult relative to low CP, moderate desister, and medium decline groups.
Table 3.
Adolescent and Adult Outcomes Associated with Trajectories of Conduct Problems from 2 to 10 years
| Adolescent & Adult Outcomes |
Low (1) (n = 29) |
Moderate Desister (2) (n = 94) |
Medium Decline (3) (n = 142) |
Chronic (4) (n = 19) |
Chi-Square Test (χ2) or Analysis of Covariance (ANCOVA) |
|---|---|---|---|---|---|
| Deviant Talk (Observation; Age 17) |
1.89 (0.45) 1 < 3,4 | 2.22 (0.25) 2 < 3,4 | 3.12 (0.20) 3 > 1,2; 3 < 4 | 5.12 (0.57) 4 > 1,2,3 | F(3, 277) = 9.61,p < .01 |
| Juvenile & Adult Violent Petitionsa |
OR = .16* [0.04, 0.65] |
OR = .17** [0.06, 0.50] |
OR = 0.33* [0.12, 0.89] |
_____ | χ2(3) = 12.08,p < .01 |
| Impulsivity (BIS; Age 20) |
29.75 (1.55) | 29.46 (0.87) | 29.90 (0.71) | 32.88 (1.96) | F(3, 274) = 0.86, p = .46 |
| Violent Behavior (SRD; Age 20) |
11.31 (0.29) 1 < 3,4 | 11.46 (0.16) 2 < 3, 4 | 12.08 (0.13) 3 > 1, 2; 3 < 4 | 13.09 (0.36) 4 > 1,2,3 | F(3, 274) = 7.99, p < .01 |
| Depressive Symptoms (BDI; Age 20) |
3.39 (0.95) 1 < 4 | 4.57 (0.53) 2 < 4 | 5.70 (0.43) 3 < 4 | 10.08 (1.20) 4 > 1,2,3 | F(3, 274) = 7.57, p < .01 |
| Anxiety Symptoms (BAI; Age 20) |
4.10 (1.40) 1 < 4 | 5.92 (0.79) 2 < 4 | 6.32 (0.64) 3 < 4 | 12.00 (1.77) 4 > 1,2,3 | F(3, 274) = 4.36, p < .01 |
Note. BIS = Barratt Impulsiveness Scale; SRD = Self-Reported Delinquency; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; Analyses control for minority status, maternal education, and family income. Marginal means (standard errors) adjusted for covariates are provided in columns with corresponding F-tests. Superscript numbers denote significant differences in mean scores between classes based on Bonferroni post-hoc comparisons, ps < .05. Underlined superscript numbers denote marginally significant differences in marginal mean scores between classes.
OR = Odds Ratio; Chronic CP is the reference group; 0 = No Violent Petitions, 1 = Violent Petitions
p< .05.
Adult Outcomes Associated with CP Trajectory Groups
We then examined whether differences in CP trajectory groups were related to measures of impulsivity, violent behavior, depression, and anxiety in early adulthood after accounting for covariates. MANCOVA results revealed a significant effect of CP trajectory group membership on the combined early adult outcomes, Pillai’s Trace = 0.13, F(12, 810) = 3.10, p < .01. We followed up the significant MANCOVA by conducting separate ANCOVAs for the four early adult outcomes. Results indicated that CP group membership was a significant predictor of self-reported violent behavior, depressive symptoms, and anxiety symptoms at age 20 (see Table 3). Because of the significant omnibus ANCOVAs, we next computed subgroup contrasts between CP trajectory groups using Bonferroni corrections. Post-hoc analyses indicated that children with chronic CP from ages 2 to 10 reported significantly higher levels of violent behavior, depression, and anxiety than the low CP and moderate desister groups. The chronic CP group also showed higher levels of depressive and anxiety symptoms than the medium decline group. Finally, children in the medium decline group demonstrated higher levels of violent behavior in early adulthood than the moderate desister group.
Adolescent Outcomes Associated with HAP Trajectory Groups
Turning to the adolescent outcomes associated with trajectories of HAP, results from the one-way ANCOVA indicated the effect of HAP group membership on observed levels of deviant talk was nonsignificant (see Table 4). Findings from the multinomial logistic regression also revealed that HAP group membership was not a significant discriminator of violent petitions in adolescence or early adulthood.
Table 4.
Adolescent and Adult Outcomes Associated with Trajectories of Hyperactivity/Attention Problems from 2 to 10 years
| Adolescent & Adult Outcomes |
Low (1) (n = 16) |
Moderate Desister (2) (n = 77) |
Moderate Stable (3) (n = 134) |
Chronic (4) (n = 57) |
Chi-Square Test (χ2) or Analysis of Covariance (ANCOVA) |
|---|---|---|---|---|---|
| Deviant Talk (Observation; Age 17) |
2.11 (0.65) | 2.63 (0.30) | 2.82 (0.21) | 3.34 (0.35) | F(3, 277) = 1.25, p = .29 |
| Juvenile & Adult Violent Petitionsa |
OR = .38 [0.08, 1.89] |
OR = .40 [0.16, 1.01] |
OR = 0.79 [0.39, 1.62] |
_____ | χ2(3) = 5.74, p = .15 |
| Impulsivity (BIS; Age 20) |
29.13 (2.17) | 29.27 (0.98) | 29.70 (0.70) | 31.75 (1.16) | F(3, 274) = 1.05, p = .37 |
| Violent Behavior (SRD; Age 20) |
10.98 (0.41) 1 < 4 | 11.74 (0.19) | 11.83 (0.13) | 12.39 (0.22) 4 > 1 | F(3, 274) = 3.57, p < .05 |
| Depressive Symptoms (BDI; Age 20) |
2.45 (1.36) 1 < 4 | 4.90 (0.61) | 5.38 (0.44) | 6.86 (0.73) 4 > 1 | F(3, 274) = 3.11, p < .05 |
| Anxiety Symptoms (BAI; Age 20) |
2.79 (1.97) 1 < 4 | 6.35 (0.89) | 5.79 (0.64) 3< 4 | 8.78 (1.06) 4 > 1,3 | F(3, 274) = 3.09, p < .05 |
Note. BIS = Barratt Impulsiveness Scale; SRD = Self-Reported Delinquency; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; Analyses control for minority status, maternal education, and family income. Marginal means (standard errors) adjusted for covariates are provided in columns with corresponding F-tests. Superscript numbers denote significant differences in mean scores between classes based on Bonferroni post-hoc comparisons, ps < .05. Underlined superscript numbers denote marginally significant differences in marginal mean scores between classes.
OR = Odds Ratio; Chronic HAP is the reference group; 0 = No Violent Petitions, 1 = Violent Petitions
p< .05.
Adult Outcomes Associated with HAP Trajectory Groups
We then examined whether group differences in HAP trajectories were related to early adult measures of impulsivity, violent behavior, depression, and anxiety. Although there was a marginally significant difference among HAP groups, Pillai’s Trace = 0.09, F(12, 810) = 1.93, p < .10, ANCOVAs revealed that HAP group membership was a significant predictor of self-reported violent behavior, depressive symptoms, and anxiety symptoms in early adulthood (see Table 4). Post-hoc comparisons indicated that children following a trajectory of chronic HAP from ages 2 to 10 showed higher levels of violent behavior, depressive symptoms, and anxiety symptoms at age 20 than the low HAP group. No other differences in early adult outcomes were evident among HAP trajectory groups.
Adolescent Outcomes Associated with Comorbid CP & HAP Trajectory Groups
Our final set of analyses focused on adolescent and early adult outcomes associated with patterns of co-occurring CP and HAP from ages 2 to 10. Results from the one-way ANCOVA indicated a significant effect of CP/HAP group membership on deviant talk (Table 5). Post-hoc analyses indicated that children in the chronic CP + chronic HAP group spoke more about antisocial topics than the chronic HAP, low HAP + low CP, and ‘others’ groups. Findings from the multinomial logistic regression also revealed that children in the chronic CP + chronic HAP group were more likely to be violent offenders than the chronic HAP-only group, low CP + low HAP group, and ‘others’ group.
Table 5.
Adolescent and Adult Outcomes Associated with Trajectories of Conduct Problems (CP) and Hyperactivity/Attention Problems (HAP) from 2 to 10 years
| Adolescent & Adult Outcomes |
Chronic HAP-only (1) (n = 42) |
Chronic CP + Chronic HAP (2) (n = 18) |
Low CP + Low HAP (3) (n = 60) |
Others (4) (n = 160) |
Chi-Square Test (χ2) or Analysis of Covariance (ANCOVA) |
|---|---|---|---|---|---|
| Deviant Talk (Observation; Age 17) |
2.81 (0.38) 1 < 2 | 5.13 (0.57) 2 > 1,3,4 | 2.16 (0.32) 3 < 2 | 2.82 (0.19) 4 < 2 | F(3, 287) = 6.87, p < .01 |
| Juvenile & Adult Violent Petitionsa |
OR = .31* [0.09, .98] |
_____ |
OR = 0.18** [0.06, 0.57] |
OR = 0.26** [0.10, 0.71] |
χ2(3) = 8.90, p < .05 |
| Impulsivity (BIS; Age 20) |
30.90 (1.30) | 32.87 (1.96) | 29.20 (1.08) | 29.63 (0.66) | F(3, 274) = 1.17, p = .32 |
| Violent Behavior (SRD; Age 20) |
11.97 (0.24)1 < 2 | 13.09 (0.37)2 > 1, 3,4 | 11.37 (0.20) 3 < 2 | 11.89 (0.12)4 < 2 | F(3, 274) = 5.79, p < .01 |
| Depressive Symptoms (BDI; Age 20) |
5.61 (0.80)1 < 2 | 10.09 (1.20)2 > 1,3,4 | 3.84 (0.66) 3 < 2 | 5.35 (0.41) 4 < 2 | F(3, 274) = 6.95, p < .01 |
| Anxiety Symptoms (BAI; Age 20) |
7.23 (1.18) | 11.99 (1.77)2 > 3,4 | 4.91 (0.98) 3 < 2 | 5.98 (0.60) 4 < 2 | F(3, 274) = 4.43, p <.01 |
Note. BIS = Barratt Impulsiveness Scale; SRD = Self-Reported Delinquency; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; Analyses control for minority status, maternal education, and family income. Marginal means (standard errors) adjusted for covariates are provided in columns with corresponding F-tests. Superscript numbers denote significant differences in mean scores between classes based on Bonferroni post-hoc comparisons, ps < .05. Underlined superscript numbers denote marginally significant differences in marginal mean scores between classes.
OR = Odds Ratio; Chronic CP + Chronic HAP is the reference group; 0 = No Violent Petitions, 1 = Violent Petitions
p< .05.
Adult Outcomes Associated with Comorbid CP & HAP Trajectory Groups
Turning to adult outcomes, we first examined group differences with respect to maternal education, child race, and family income. In instances in which a grouping variable and covariates are related, removing the variance associated with covariates may alter the groups in potentially problematic ways (Miller & Chapman, 2001). As shown in Supplemental Table 1, there were no systematic group differences on covariates, indicating that application of the MANCOVA was appropriate in the current study.
The overall MANCOVA yielded a statistically significant finding for the effect of CP/HAP trajectories on the combined early adult outcomes, Pillai’s Trace = 0.11, F(12, 810) = 2.47, p < .01. Follow-up ANCOVAs were significant for three of the four adult outcomes (Table 5), including violent behavior, depressive symptoms, and anxiety symptoms at age 20. Post-hoc contrasts indicated that children with chronic CP + chronic HAP demonstrated significantly higher levels of violent behavior, depressive symptoms, and anxiety symptoms than the low CP + low HAP and ‘others’ group. The chronic CP + chronic HAP group also showed higher levels of depressive symptoms at age 20 relative to the chronic HAP group.
Discussion
This paper sought to extend our understanding of how early developmental trajectories of overt CP and HAP relate to adolescent and early adult outcomes. Consistent with study hypotheses and prior research, results of the current study suggest that trajectories of CP beginning in early childhood are specifically related to violent behavior in adolescence and adulthood, established adolescent correlates of AB (i.e., deviant talk with peers), and internalizing problems in adulthood. As expected, children in the chronic CP group showed the highest levels of deviant talk in adolescence, were more likely to have a petition for a violent crime petition as a juvenile or adult, and showed the highest levels of violent behavior, depressive symptoms, and anxiety symptoms in early adulthood when compared to all other groups. Turning to the analyses that linked trajectories of HAP to boys’ later adjustment, we found that boys with chronically high levels of HAP from ages 2 to 10 had higher levels of violent behavior, depression, and anxiety in early adulthood relative to children with persistently low HAP. The chronic HAP group did not differ from the moderate desister or moderate stable HAP groups on later problem behavior. Finally, children with chronic CP + chronic HAP appeared to be most at risk for multiple types of problem behaviors in adolescence and early adulthood.
Results from the present study corroborate and extend prior research showing that children who demonstrate elevated levels of CP as early as toddlerhood often continue to do so throughout adolescence and early adulthood (Aguilar, Sroufe, Egeland, & Carlson, 2000; Moffitt et al., 2002; NICHD Early Child Care Research Network, 2004; Odgers et al., 2008). Thus, although oppositional and aggressive behaviors prior to age 2 are likely to be transient for most children, for a small group of children, high rates of disruptive behaviors in toddlerhood may represent the beginning of a life-course persistent trajectory of AB (Moffitt, 2006). While early-starters represent a small percentage of the population, they are nonetheless responsible for approximately half of adolescent crimes and three-fourths of violent crimes (Loeber, 1982, Offord, Boyle, & Racine, 1991). These findings highlight the importance of early preventive interventions aimed at altering trajectories of early-starting CP before they escalate to more serious forms of violent behavior in adolescence and early adulthood, ranging from mass murders and rampage violence to violent crimes involving a single victim (e.g., physical assault, rape).
Unlike trajectories of CP, early trajectories of HAP were generally not predictive of later problem behavior in isolation. When we only considered HAP symptomology from ages 2 to 10, boys with chronically high levels of HAP showed greater violent behavior as adults compared to children with persistently low HAP. However, in contrast to children with persistently high HAP and CP, the chronic HAP-only group did not differ from the low CP/HAP group on adult outcomes. Further, compared to the chronic CP + chronic HAP group, children with chronic HAP-only showed fewer negative outcomes -- they engaged in less deviant talk during an observational task with a peer at age 17 and were less likely to have a petition for a violent crime in adolescence or early adulthood. Thus, chronic HAP was no longer predictive of adolescent or adult violent behavior once its overlap with co-occurring CP was considered. Our results are consistent with prior work documenting the heterogeneity of outcomes for children with HAP (Molina & Pelham, 2014). Indeed, despite the common vulnerability to impulsivity shared by HAP and CP, research has shown that about two thirds of youth showing symptoms of HAP do not go on to develop serious CPs because of protective environmental conditions (Lynam et al., 2000; Meier, Slutske, Arndt, & Cadoret, 2008). Children with chronic HAP-only may follow a separable developmental pathway characterized by fewer points of entry to serious CPs, possibly explaining why symptoms of HAP in the absence of CP provide little incremental value to the prediction of later AB (Lahey, McBurnett, & Loeber, 2000; Lahey et al., 2010; Loeber, Green, Keenan, & Lahey, 1995). Results from the present study suggest that elevated CP in early childhood is likely the best predictor of future violent behavior as an adolescent or adult.
It is notable that differences between the chronic CP + chronic HAP group and chronic HAP-only group emerged primarily for deviant talk and violent offenses. The fact that both constructs were assessed with more objective measures (i.e., observational tasks coded by project staff and official court records) suggests that the lack of group differences in self-reported violent behavior at age 20 may in part be attributable to youth underreporting on their antisocial activities. Indeed, using the current sample of all men, Shaw, Hyde, and Brennan (2012) found that men following a high decreasing trajectory of CP actually had a high percentage of court involvement (60%) despite low levels of endorsement on the Self-Report of Delinquency (SRD) at age 15 and 17. Thus, we believe that the present findings reveal important differences in AB between the chronic CP + chronic HAP and chronic-HAP only groups even if such differences are less likely to be detected relying on self-reported measures.
Consistent with prior research suggesting that a small fraction of the adult population may account for a disproportionate share of societal costs (e.g., Caspi et al., 2016), children with co-occurring CP and HAP not only showed the highest levels of violent behavior, but they also demonstrated greater depressive and anxiety symptoms compared to other groups. Notably, Caspi et al. (2016) found that low self-control in childhood predicted adult membership in the multiple-high-cost segment of the population. Further, although Shaw et al. (2005) did not examine self-control per se, authors found that child fearlessness was an important factor discriminating CP and HAP groups, such that children following trajectories of high HAP and high CP were more fearless compared with children with persistently low CP + low HAP. Collectively, results suggest that childhood self-control is an important factor to consider in the early identification and treatment of children showing early co-occurring patterns of CP and HAP.
Consistent with the dual-failure model, it is possible that the aggressive and aversive behavior of children with early CP may contribute to interpersonal problems (e.g., conflict with caregivers, peer rejection) and poor academic performance, which in turn lead to mood problems (Capaldi, 1991; Capaldi & Stoolmiller, 1999). However, while it is possible that depressive and anxiety symptoms may follow from demoralizations related to repeated failures, the lack of earlier measures of depression or anxiety and the non-experimental nature of the study’s design precludes inferring directionality of this association between early CP and later internalizing problems.
Our findings suggest that children with chronic CP + chronic HAP are most at risk for showing both homotypic (e.g., violent behavior) and heterotypic (i.e., internalizing symptoms) continuity. The individual traits and environmental risks that underlie chronic CP + chronic HAP may be especially pernicious, continuing to manifest in varying forms well into adulthood. This stands in contrast to all other CP and HAP groups, which showed similar functioning relative to those with low problem behaviors by adulthood (i.e., they showed discontinuities in problem behavior). Of course, our results do not provide unequivocal evidence for homotypic or heterotypic continuity. As outlined previously, chronic CP + chronic HAP may also predict AB-related outcomes and internalizing symptoms indirectly through cascading effects over the course of development. Nonetheless, our findings suggest that discovering the latent traits underlying chronic CP + chronic HAP could clarify the mechanisms by which individuals manifest multiple forms of problem behavior throughout the life course.
In contrast to adolescent and adult violent behavior, depression, and anxiety, there were no group differences with respect to impulsivity in early adulthood, regardless of whether CP and HAP trajectories were assessed separately or concurrently. Notably, even children with persistently high levels of HAP from toddlerhood through middle childhood reported comparable levels of impulsivity in adulthood as all other HAP groups. These findings are consistent with research showing that although symptoms of hyperactivity and impulsivity are prominent in preschool, they tend to decrease with age as inattention becomes increasingly common and problematic (APA, 2013; Galéra et al., 2011; Kooij et al., 2010; Lahey et al., 2005). Although we did not collect measures of inattention in early adulthood, future research would benefit from examining whether HAP trajectory groups differ in inattention despite non-significant differences in impulsivity.
Limitations
There are several limitations of the study that warrant further consideration. First, the current sample was originally recruited from WIC nutrition supplement centers in a single metropolitan area, and thus, families faced financial hardships and other correlates of financial adversity (e.g., living in poor neighborhoods). The present sample was recruited because male children from low-SES backgrounds are at a greater risk for showing meaningful levels of AB, but findings may not generalize to girls or children from other socioeconomic strata (Miller, Malone, & Dodge, 2010).
Second, as many children in the chronic CP group also showed chronic HAP in early childhood, we lacked statistical power to evaluate a “pure” chronic CP group. Thus, while HAP trajectories generally did not predict adult functioning once co-occurring CP was considered, it remains unclear whether children presenting with both chronic HAP and chronic CP are more impaired as adults relative to children with chronic CP-only. Indeed, meta-analytic findings suggest an additive combination of HAP and CP, such that children presenting with both types of behavioral problems exhibit more severe and varied types of AB relative to children with CP-only (Washbusch, 2002).
Finally, the current study did not distinguish between inattention and hyperactivity problems. The small body of work examining whether inattention and hyperactivity are differentially related to AB has yielded inconclusive findings – some studies reported a predominant role for hyperactivity in the prediction of criminal behavior (Babinski et al., 1999; Pardini & Fite, 2010), while another study found inattention symptoms to be more important (Eklund & Klinteberg, 2003). Nonetheless, other work has shown that neither childhood hyperactivity nor inattention are predictive of later AB after accounting for their overlap with physical aggression (e.g., Pingault et al., 2013). Further, while there is continued debate about the distinctiveness of ADHD subtypes (e.g., Milich, Balantine, & Lynam, 2001), there is evidence that children with hyperactive and attention problems (i.e., ADHD-Combined) and children presenting primarily with inattention difficulties (i.e., ADHD-Inattentive) are comparably impaired as adults across multiple symptom areas (e.g., Hinshaw et al., 2012). Thus, there is reason to believe that findings from the present study would have been replicated had we modeled separate trajectories for inattention and hyperactivity.
Implications for early intervention
In spite of these limitations, the present study extends previous research by examining the predictive value of early developmental trajectories of HAP, CP, and co-occurring HAP and CP in a sample strengthened by its use of multiple assessment methods (i.e., observational data, official court records, self-report), prospective longitudinal design, and high levels of retention over 20 years. Studies examining associations between early ADHD symptoms and later AB frequently fail to account for co-occurring CP, making it difficult to determine the unique contributions of HAP in early childhood to adult AB. Findings from the current study underscore the importance of assessing for co-occurring CP among children presenting with elevated HAP to determine which youth may be at greatest risk for later violent behavior. Additionally, past research linking early trajectories of CP and HAP with adolescent and adult functioning have typically been initiated during the school-aged years (e.g., Nagin et al., 1999; Pingault et al., 2013); fewer studies have followed trajectories beginning as young as age 2 (Renken, Egeland, Marvinney, Mangelsdorf, & Sroufe, 1989). Our success in using developmental trajectories of CP and HAP beginning in toddlerhood to predict functioning through late adolescence and early adulthood suggest that early identification may be warranted for children showing early co-occurring patterns of CP and HAP. Developmentally, early childhood is an optimal time for initiating prevention efforts because of the greater malleability of child behavior and family relationships relative to later developmental periods (Reid, Webster-Stratton, & Baydar, 2004). Further, consistent with prior research suggesting that a small fraction of the adult population may account for a disproportionate share of societal costs (e.g., Caspi et al., 2016), children with co-occurring CP and HAP not only showed the highest levels of violent behavior, but they also demonstrated greater depressive and anxiety symptoms compared to other groups. Thus, although providing resources to identify these high-risk children in early childhood poses a formidable challenge for policy makers, this group of children seems to be a high-value target for prevention efforts given their risk for impaired functioning across several domains through late adolescence and early adulthood.
Supplementary Material
Acknowledgements of grant support:
This research was supported by National Institute on Drug Abuse Grants DA25630 and DA26222 awarded to D.S. Shaw and E.E. Forbes. We thank the staff of the Pitt Mother and Child Project and the study families for making the research possible.
Footnotes
Statements of conflict of interest: The authors have no conflicts of interest to report
References
- Achenbach TM (1991). Manual for Child Behavior Checklist/ 4–18 and 1991 Profile. Burlington, VT: University of Vermont, Dept. of Psychiatry. [Google Scholar]
- Achenbach TM (1992). Manual for Child Behavior Checklist/ 2–3 and 1992 Profile. Burlington, VT: University of Vermont, Dept. of Psychiatry. [Google Scholar]
- Aguilar B, Sroufe LA, Egeland B, & Carlson E (2000). Distinguishing the early-onset/persistent and adolescence-onset antisocial behavior types: From birth to 16 years. Development and Psychopathology, 12(2), 109–132. [DOI] [PubMed] [Google Scholar]
- Babinski LM, Hartsough CS, & Lambert NM (1999). Childhood conduct problems, hyperactivity-impulsivity, and inattention as predictors of adult criminal activity. Journal of Child Psychology and Psychiatry, 40(3), 347–355. [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J (1961). An Inventory for Measuring Depression. Archives of General Psychiatry, 4(6), 561–571. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Dolan C, Hughes S, Mick E, Monuteaux MC, & Faraone SV (2008). The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: Findings from a controlled 10-year prospective longitudinal follow-up study. Psychological Medicine, 38(7), 1027–1036. [DOI] [PubMed] [Google Scholar]
- Capaldi DM (1991). Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: I. Familial factors and general adjustment at Grade 6. Development and Psychopathology, 3(3), 277. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, & Stoolmiller M (1999). Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment. Development and Psychopathology, 11(1), 59–84. [DOI] [PubMed] [Google Scholar]
- Caspi J, & Barrios VR (2016). Destructive sibling aggression In Cuevas CA, & Rennison CM (Eds.), The Wiley Handbook on the Psychology of Violence (pp. 297–323) Wiley-Blackwell. [Google Scholar]
- Dishion TJ, & Patterson GR (in press). The development and ecology of problem behavior: Linking etiology, prevention, and treatment In Cicchetti D (Ed.), Handbook for developmental psychopathology. [Google Scholar]
- Eklund JM, & Klinteberg BAF (2003). Childhood behaviour as related to subsequent drinking offences and violent offending: A prospective study of 11- to 14-year-old youths into their fourth decade. Criminal Behaviour and Mental Health, 13(4), 294–309. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, & Ageton SS (1985). Explaining delinquency and drug use. Beverly Hills: Sage Publications. [Google Scholar]
- Farrington DP, Loeber R & Van Kammen WB (1990). Long-term criminal outcomes of hyperactivity-impulsivity-attention deficit and conduct problems in childhood In Robins LN & Rutter MR (Eds.),Straight and devious pathways from childhood to adulthood(pp. 62–81). Cambridge, England: Cambridge University Press [Google Scholar]
- Fontaine N, Carbonneau R, Barker ED, Vitaro F, Hébert M, Côté SM, … Tremblay RE (2008). Girls’ hyperactivity and physical aggression during childhood and adjustment problems in early adulthood: A 15-year longitudinal study. Archives of General Psychiatry, 65(3), 320–328. [DOI] [PubMed] [Google Scholar]
- Galéra C, Côté SM, Bouvard MP, Pingault J, Melchior M, Michel G, . . . Tremblay RE (2011). Early risk factors for hyperactivity-impulsivity and inattention trajectories from age 17 months to 8 years. Archives of General Psychiatry, 68(12), 1267–1275. [DOI] [PubMed] [Google Scholar]
- Gatzke-Kopp LM, Beauchaine TP, Shannon KE, Chipman J, Fleming AP, Crowell SE, … Johnson LC (2009). Neurological Correlates of Reward Responding in Adolescents With and Without Externalizing Behavior Disorders. Journal of Abnormal Psychology, 118(1), 203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granic I, & Dishion TJ (2003). Deviant talk in adolescent friendships: A step toward measuring a pathogenic attractor process. Social Development, 12(3), 314–334. [Google Scholar]
- Hechtman L, Weiss G, Perlman T, & Amsel R (1984). Hyperactives as young adults: Initial predictors of adult outcome. Journal of the American Academy of Child Psychiatry, 23(3), 250–260. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado A, Schrodek E, & Swanson EN (2012). Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology, 80(6), 1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AA (1975). Four-factor index of social status. Unpublished manuscript, Yale University, New Haven, CT. [Google Scholar]
- Humphreys KL, & Lee SS (2011). Risk taking and sensitivity to punishment in children with ADHD, ODD, ADHD+ODD, and controls. Journal of Psychopathology and Behavioral Assessment, 33(3), 299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp (2013). IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- Kessler RC (1994). Building on the ECA: The national comorbidity survey and the children’s ECA. International Journal of Methods in Psychiatric Research, 4(2), 81–94. [Google Scholar]
- Kooij SJJ, Bejerot S, Blackwell A, Caci H, Casas-Brugué M, Carpentier PJ, … Asherson P (2010). European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD. BMC Psychiatry, 10(1), 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke J, Rathouz PJ, & McBurnett K (2002). Waxing and waning in concert: Dynamic comorbidity of conduct disorder with other disruptive and emotional problems over 17 years among clinic-referred boys. Journal of abnormal psychology, 111(4), 556. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke JD, & Applegate B (2005). Predicting future antisocial personality disorder in males from a clinical assessment in childhood. Journal of Consulting and Clinical Psychology, 73(3), 389. [DOI] [PubMed] [Google Scholar]
- Lahey BB, McBurnett K, & Loeber R (2000). Are attention-deficit/hyperactivity disorder and oppositional defiant disorder developmental precursors to conduct disorder? In Sameroff AJ, Lewis M & Miller SM (Eds.), 2nd ed.; handbook of developmental psychopathology (2nd ed.) (2nd ed. ed., pp. 431–446, Chapter xxxi, 813 Pages) Kluwer Academic Publishers, Dordrecht. [Google Scholar]
- Lahey BB, & Willcutt EG (2010). Predictive validity of a continuous alternative to nominal subtypes of attention-deficit/hyperactivity disorder for DSM-V. Journal of Clinical Child and Adolescent Psychology, 39(6), 761–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SS, & Hinshaw SP (2004). Severity of adolescent delinquency among boys with and without attention deficit hyperactivity disorder: Predictions from early antisocial behavior and peer status. Journal of Clinical Child and Adolescent Psychology, 33(4), 705–716. [DOI] [PubMed] [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, & Glass K (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review, 31(3), 328–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R (1982). The stability of antisocial and delinquent child behavior: A review. Child Development, 53(6), 1431–1446. [PubMed] [Google Scholar]
- Loeber R, & Dishion T (1983). Early predictors of male delinquency: A review. Psychological Bulletin, 94(1), 68–99. [PubMed] [Google Scholar]
- Loeber R, Brinthaupt VP, & Green SM (1990). Attention deficits, impulsivity, and hyperactivity with or without conduct problems: Relationships to delinquency and unique contextual factors. Behavior disorders of adolescence: Research, intervention, and policy in clinical and school settings, 39–61. [Google Scholar]
- Loeber R, Green SM, Keenan K, & Lahey BB (1995). Which boys will fare worse? early predictors of the onset of conduct disorder in a six-year longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry, 34(4), 499–509. [PubMed] [Google Scholar]
- Loeber R, Stepp SD, Chung T, Hipwell AE, & White HR (2010). Time-varying associations between conduct problems and alcohol use in adolescent girls: The moderating role of race. Journal of Studies on Alcohol and Drugs, 71(4), 544–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig J (2010). The costs of crime. Criminology & Public Policy, 9, 307–311. [Google Scholar]
- Mannuzza S, Klein RG, Abikoff H, & Moulton John L. I.,II. (2004). Significance of childhood conduct problems to later development of conduct disorder among children with ADHD: A prospective follow-up study. Journal of Abnormal Child Psychology, 32(5), 565–573. [DOI] [PubMed] [Google Scholar]
- Masunami T, Okazaki S, & Maekawa H (2009). Decision-making patterns and sensitivity to reward and punishment in children with attention-deficit hyperactivity disorder. International Journal of Psychophysiology, 72(3), 283–288. [DOI] [PubMed] [Google Scholar]
- Mathias CW, Furr RM, Daniel SS, Marsh DM, Shannon EE, & Dougherty DM (2007). The relationship of inattentiveness, hyperactivity, and psychopathy among adolescents. Personality and Individual Differences, 43(6), 1333–1343. [Google Scholar]
- Meinzer MC, Pettit JW, Waxmonsky JG, Gnagy E, Molina BS, & Pelham WE (2016). Does childhood attention-deficit/hyperactivity disorder (ADHD) predict levels of depressive symptoms during emerging adulthood? Journal of Abnormal Child Psychology, 44(4), 787–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GA, & Chapman JP (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110(1), 40. [DOI] [PubMed] [Google Scholar]
- Miller S, Malone PS, & Dodge KA (2010). Developmental trajectories of boys’ and girls’ delinquency: Sex differences and links to later adolescent outcomes. Journal of Abnormal Child Psychology, 38(7), 1021–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milich R, Balentine AC and Lynam DR (2001), ADHD Combined Type and ADHD Predominantly Inattentive Type Are Distinct and Unrelated Disorders. Clinical Psychology: Science and Practice, 8: 463–488. [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, & Milne BJ (2002). Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology, 14(1), 179–207. [DOI] [PubMed] [Google Scholar]
- Moffitt TE (2006). Life-course-persistent versus adolescence-limited antisocial behavior In Cicchetti D, & Cohen DJ (Eds.), 2nd ed.; developmental psychopathology: Risk, disorder, and adaptation (vol. 3, 2nd ed.) (2nd ed. ed., pp. 570–598, Chapter xvi, 944 Pages) John Wiley & Sons Inc, Hoboken, NJ. [Google Scholar]
- Mordre M, Groholt B, Kjelsberg E, Sandstad B, & Myhre AM (2011). The impact of ADHD and conduct disorder in childhood on adult delinquency: A 30 years follow-up study using official crime records. BMC psychiatry, 11(1), 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS (1999). Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods, 4(2), 139–157. [DOI] [PubMed] [Google Scholar]
- Nagin D, & Tremblay RE (1999). Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Development, 70(5), 1181–1196. [DOI] [PubMed] [Google Scholar]
- Nagin DS, & Tremblay RE (2001). Parental and early childhood predictors of persistent physical aggression in boys from kindergarten to high school. Archives of General Psychiatry, 58(4), 389–394. [DOI] [PubMed] [Google Scholar]
- Odgers CL, Moffitt TE, Broadbent JM, Dickson N, Hancox RJ, Harrington H, . . . Caspi A (2008). Female and male antisocial trajectories: From childhood origins to adult outcomes. Development and Psychopathology, 20(2), 673–716. [DOI] [PubMed] [Google Scholar]
- Boyle MH, & Offord DR (1991). Psychiatric disorder and substance use in adolescence. The Canadian Journal of Psychiatry / La Revue Canadienne De Psychiatrie, 36(10), 699–705. [PubMed] [Google Scholar]
- Pardini DA, & Fite PJ (2010). Symptoms of conduct disorder, oppositional defiant disorder, attention-deficit/hyperactivity disorder, and callous-unemotional traits as unique predictors of psychosocial maladjustment in boys: Advancing an evidence base for DSM-V. Journal of the American Academy of Child & Adolescent Psychiatry, 49(11), 1134–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, & Barratt ES (1995). Factor structure of the barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774. 3.0. [DOI] [PubMed] [Google Scholar]
- Pingault JB, Côté SM, Booij L, Ouellet-Mohn I, Castellanos-Ryan N, Vitaro F, . . . Tremblay RE (2013). Age-dependent effect of the MAOA gene on childhood physical aggression. Molecular Psychiatry, 18(11), 1151–1152. [DOI] [PubMed] [Google Scholar]
- Renken B, Egeland B, Marvinney D, Mangelsdorf S, & Sroufe LA (1989). Early childhood antecedents of aggression and passive-withdrawal in early elementary school. Journal of Personality, 57(2), 257–281. [DOI] [PubMed] [Google Scholar]
- Reid MJ, Webster-Stratton C, & Baydar N (2004). Halting the development of conduct problems in Head Start children: The effects of parent training. Journal of Clinical Child and Adolescent Psychology, 33(2), 279–291. [DOI] [PubMed] [Google Scholar]
- Rivenbark JG, Odgers CL, Caspi A, Harrington H, Hogan S, Houts RM, Poulton R, Moffitt TE (2017). The high societal costs of childhood conduct problems: Evidence from administrative records up to age 38 in a longitudinal birth cohort. Journal of Child Psychology and Psychiatry, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz DB, & Rostain AL (2006). ADHD with comorbid anxiety: a review of the current literature. Journal of Attention disorders, 10(2), 141–149. [DOI] [PubMed] [Google Scholar]
- Seymour KE, Macatee R, & Chronis-Tuscano A (2016). Frustration Tolerance in Youth With ADHD. Journal of Attention Disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Gilliom M, Ingoldsby EM, & Nagin DS (2003). Trajectories leading to school-age conduct problems. Developmental Psychology, 39(2), 189–200. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Criss MM, Schonberg MA, & Beck JE (2004). The development of family hierarchies and their relation to children’s conduct problems. Development and Psychopathology, 16(3), 483–500. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Lacourse E, & Nagin DS (2005). Developmental trajectories of conduct problems and hyperactivity from ages 2 to 10. Journal of Child Psychology and Psychiatry, 46(9), 931–942 [DOI] [PubMed] [Google Scholar]
- Shaw DS, Hyde LW, & Brennan LM (2012). Early predictors of boys’ antisocial trajectories. Development and Psychopathology, 24(3), 871–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Biswas A, … Karch KM (2011). The delinquency outcomes of boys with ADHD with and without comorbidity. Journal of Abnormal Child Psychology, 39(1), 21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sitnick SL, Shaw DS, Weaver CM, Shelleby EC, Choe DE, Reuben JD, . . . Taraban L (2017). Early childhood predictors of severe youth violence in low-income male adolescents. Child Development, 88(1), 27–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA, Daleiden E, & Drabman RS (2000). Are parents accurate reporters of their child’s cognitive abilities? Journal of Psychopathology and Behavioral Assessment, 22(1), 61–77. [Google Scholar]
- Waschbusch DA (2002). A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin, 128(1), 118–150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


